Ambrisentan and the LGBTQ+ Community: Bridging Gaps in PAH Treatment
Treatment for pulmonary arterial hypertension (PAH) can feel overwhelming. Now, throw in being a member of the LGBTQ+ community and the road gets even bumpier. You’d think in 2025, getting the right meds—like ambrisentan—would just be about health. Turns out, there’s more to it.
Ambrisentan helps folks with PAH breathe easier and live better, but research shows that LGBTQ+ patients often face extra hoops to jump through. Stuff like care providers not taking gender identity seriously, health insurance confusion, or even subtle bias can leave some folks behind. And when you’re dealing with a lifelong condition like PAH, every little delay or misunderstanding matters.
The goal isn’t just to shoo away stigma—it’s about practical steps, like finding doctors who are actually informed about LGBTQ+ health and double-checking pharmacy support for specific meds. Even picking up ambrisentan at the pharmacy can turn awkward or complicated if the system gets your name or gender wrong on the script.
If any of this sounds familiar, you’re not alone. The real fix has to be both big and small: better training for providers, clearer insurance rules, those everyday conversations where you don’t have to educate your doctor before you even get to your symptoms. Let’s talk about what actually makes a difference—where things stand, the real-life barriers, and ways to get around them.
- PAH and Ambrisentan in Plain Terms
- Why Disparities Hit the LGBTQ+ Community
- Everyday Barriers at Clinics and Pharmacies
- Ways Forward: Tips and System Solutions
PAH and Ambrisentan in Plain Terms
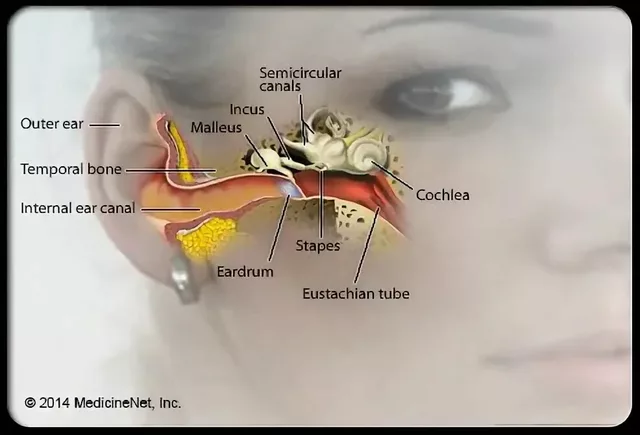
Let’s keep it simple: pulmonary arterial hypertension, or PAH, messes with the arteries in your lungs. These arteries get tight and narrow, which means your heart has to work a lot harder just to push blood through. Over time, that’s tough on the heart. You might catch yourself feeling short of breath, getting tired fast, or feeling a weird pressure in your chest even if you’re just climbing stairs.
Treating PAH isn’t just about popping one pill and forgetting about it. It usually takes a mix of medications, lifestyle changes, and lots of doctor appointments. This is where ambrisentan comes in—it’s one of the go-to prescription drugs specialists use because it directly helps open up those small, tight arteries. Ambrisentan blocks a certain hormone called endothelin, which is what makes arteries squeeze too much. By blocking it, blood can flow more freely and your heart doesn’t have to work as hard.
What’s cool is the numbers back this up. Studies show ambrisentan can lift exercise capacity (meaning you might actually walk further, or do more before running out of steam) and put the brake on some of the nasty changes PAH causes in the heart and lungs. Here’s a peek at some key facts:
| Fact | Details |
|---|---|
| FDA Approval | 2007 for PAH |
| Main use | Improves exercise ability, slows symptoms |
| Common side effects | Flushing, swelling in legs, stuffy nose |
Taking ambrisentan once a day (usually as a tablet) keeps things straightforward, especially compared to some therapies needing continuous infusions or oxygen tanks. But just because it’s simple to take doesn’t mean folks shouldn’t watch out for side effects—like swelling in the ankles or possible liver issues—so regular blood work is a thing your doctor might order.
Most insurers cover ambrisentan, but there are still headaches with getting the prescription filled, which usually means dealing with specialty pharmacies rather than just strolling into your local drugstore. This stuff matters for everyone, but sorting it out gets crucial when communities like LGBTQ+ folks are already more likely to deal with awkward questions or insurance mix-ups.
Why Disparities Hit the LGBTQ+ Community
Let’s be real—healthcare isn’t always a level playing field, and that gets even more obvious if you’re part of the LGBTQ+ community needing PAH treatment like ambrisentan. Shockingly, a 2023 survey from the American Heart Association found that LGBTQ+ folks are 2.5 times more likely to delay or avoid medical care than non-LGBTQ+ peers, especially when it comes to chronic conditions. That ends up affecting everything from how fast diagnosis happens to whether or not the right drugs get prescribed in the first place.
Why does this happen? There’s not just one culprit. Plenty of LGBTQ+ patients report that doctors seem uncomfortable with their identity or just skip over important details. This matters a lot with ambrisentan: for example, hormone therapy for transgender people might interact with PAH meds, but not every doctor takes this into account—sometimes because they simply don’t ask the right questions.
Another big piece is insurance. Some insurance plans dragged their feet until just a few years ago when it came to covering meds like ambrisentan for LGBTQ+ people, especially those whose legal names or genders didn’t match their documents. Imagine being denied medicine just because the system has you listed with an old name or gender. Sounds wild, but these things are still happening in some places.
And then there’s the more subtle stuff, like the stress of having to out yourself—again—to a new specialist, or having to explain your health needs in ways straight, cisgender people usually never deal with. Studies keep showing that minority stress—just the day-to-day feeling of not being welcome—can literally mess with your health and make you less likely to stick with tough regimens like daily ambrisentan.
| Barrier | How It Shows Up |
|---|---|
| Provider Bias | Skipping key questions about gender, sexuality, or medications |
| Insurance Problems | Delays due to mismatched names/genders on coverage |
| Communication Gaps | Patient doesn’t feel safe or heard, leading to info gaps |
Tackling these gaps isn’t just about paying lip service. It takes practical fixes—making clinics more inclusive, getting providers up to speed, and using technology to make sure paperwork actually reflects who people are. Until more of that happens, those disparities aren’t going anywhere fast.

Everyday Barriers at Clinics and Pharmacies
Walking into a clinic or pharmacy to get ambrisentan can feel like a minefield when you’re part of the LGBTQ+ community. It’s not just about prescriptions—it’s about how you’re seen, spoken to, and even how your insurance details are handled. Surveys show that around 16% of LGBTQ+ patients have avoided medical care due to concerns about discrimination, with even higher rates for transgender people.
Picture this: you share your gender identity with a new provider, and suddenly they’re shuffling around and awkward instead of just treating your PAH. Or you head to the pharmacy, and your prescription doesn’t match your legal paperwork because of a name change. Now, what should’ve been a quick pickup turns into a drawn-out headache. These aren’t rare bad days—they’re a pattern for many.
"Too many LGBTQ+ patients face extra steps just to get medications like ambrisentan, from battling insurance codes that don’t match their gender to navigating staff who aren’t trained in LGBTQ+ health needs." — Dr. Brian Hurley, president of GLMA: Health Professionals Advancing LGBTQ+ Equality
Insurance is another beast. Some LGBTQ+ folks get denied coverage for certain medications, like ambrisentan, if their official gender marker doesn’t fit the system’s old rules about who gets what meds. And if you have to explain or correct something every visit, that wears you down fast.
- Accurate name and gender information: If clinic or pharmacy records aren’t up-to-date, getting ambrisentan can turn into a paperwork mess.
- Provider knowledge gaps: Some doctors and pharmacists just don’t know much about LGBTQ+ health, which can lead to mistakes or awkward moments.
- Insurance glitches: Gender marker mismatches or relationship status confusion can lead to slowdowns or denials, making it harder to get covered for your medication.
- Feeling safe and welcome: It’s tough to be open about your health if you worry you’ll get judged or misunderstood. That leads some people to delay or skip important care.
Here’s the kicker: delays in PAH treatment make things worse. According to a study from the American Heart Association, untreated or delayed therapy for PAH increases the risk of hospitalization and shortens life expectancy. That’s why these everyday barriers at clinics and pharmacies matter so much—they’re not just annoyances, they affect real outcomes.
Ways Forward: Tips and System Solutions
Every person with PAH deserves straightforward, respectful treatment. But if you’re in the LGBTQ+ crowd, you know it’s not always that smooth. Taking action—both on your own and at the system level—can make a big difference in getting the most from meds like ambrisentan.
If you’re looking for practical ways to make things easier, here are some steps:
- Find affirming care teams: Some clinics and doctors specialize in, or at least advertise, LGBTQ+ friendly care. Word of mouth, online directories, and local community centers are good places to check before booking an appointment.
- Double-check prescription details: Minor slip-ups—wrong gender marker, a deadname on records, unclear dosage—can hold up your ambrisentan at the pharmacy. Bring it up, even if it feels awkward. Pharmacists can fix the script details faster than most folks expect.
- Bring support if you want it: A friend, partner, or advocate can help you ask questions, spot issues, or back you up if bias pops up. I’ve seen first-hand how having someone like Lillian in my corner turns difficult appointments around.
- Know your insurance rights: Transgender and gender-diverse folks sometimes get tripped up by insurance systems that don’t match their identity info with their health needs. The National Center for Transgender Equality lays out tips for handling claim denials and name/gender mismatches.
Bigger fixes usually have to come from the healthcare system, but patients—and their friends and families—can push for change. Community feedback helps clinics get their training in line. If you run into discrimination or confusion, consider reporting it through patient advocacy offices or state health agencies. It’s not about getting someone in trouble—it’s about making your experience count so the next person has it easier.
| Barrier | Percent Reporting Difficulty |
|---|---|
| Name/Gender Mismatch | 22% |
| Poor Clarity on Covered Drugs | 30% |
| Delayed Authorizations | 18% |
A handful of major insurers started rolling out digital tools in late 2024 that let patients update their names and pronouns themselves. It’s not perfect, but it’s a step in the right direction for anyone taking meds like ambrisentan.
The bottom line: Know your options, speak up when needed, and lean on LGBTQ+ community groups for recommendations and support. Even small wins—like making it out of the pharmacy with your medicine and your dignity—matter more than people think.




12 Comments
Glenda Rosa
July 18, 2025 at 05:07
Honestly, it’s surprising that even in 2024 we still have to talk about disparities in a treatment as critical as for PAH in the LGBTQ+ community. The article points out systemic obstacles, yes, but I think it underestimates the sheer complexity of these healthcare barriers. Stigma, misinformation, implicit biases—they all interweave into a tapestry that often leaves LGBTQ+ patients marginalized. Ambrisentan might be effective, but access and appropriate care coordination are just as important!
Also, I’d argue the article glosses over how the healthcare system itself resists tailored approaches due to bureaucratic inertia. It’s not just about patient advocacy; providers need thorough cultural competency training that actually sticks. Only then can we even start leveling the playing field.
But hey, acknowledging the problem is the first step, I guess.
lata Kide
July 19, 2025 at 20:33
OMG, totally agree! 🙌🙌 And let’s not forget how emotionally draining it is for many LGBTQ+ individuals just to step into a doctor’s office, right? The mental toll alone can worsen PAH symptoms. The article touched on this, but not deeply enough.
Plus, I’ve seen way too many cases where trans patients had to battle for correct dosages or had their identities outright ignored by healthcare staff. That kind of neglect can cost lives. 😡
Patients need allies everywhere, from doctors to pharmacists, to even fellow patients sharing their stories. Community support is everything in these battles.
Anyone else experience or witness these frustrations firsthand?
Francisco Garcia
July 22, 2025 at 18:00
Such a crucial discussion here. I’d like to point out that focusing on medications like ambrisentan is great, but the larger context involves social determinants of health — things like housing stability, discrimination, and access to insurance, which disproportionately impact the LGBTQ+ community.
It’s not enough to just offer a drug if folks can’t even get to their appointments or afford copays. Policy reforms are also essential alongside clinical strategies. How do we advocate more effectively for such changes on both local and national levels?
Collaboration between patient groups, healthcare providers, and lawmakers is vital if we want any real progress.
KAYLEE MCDONALD
July 24, 2025 at 13:03
This article is important, but it felt a little light on concrete advice on how patients can self-advocate, which is something I focus on a lot. It’s one thing to recognize systemic barriers; it’s another to empower individuals with clear tools to navigate those barriers.
For example, patients can prepare detailed symptom logs, bring support persons to visits, and request referrals to LGBTQ+-friendly providers. Knowing rights and speaking up respectfully also makes a difference.
And healthcare teams should welcome and nurture this patient assertiveness rather than feel threatened by it. Partnership is key to better outcomes.
Aaron Perez
July 27, 2025 at 09:06
Ah, the eternal dance between medicine and identity politics! But let’s not be naïve here: is ambrisentan truly the be-all and end-all for PAH across the LGBTQ+ spectrum, or is it just a token nod in a larger, performative effort to appear inclusive?
Healthcare often dangles cutting-edge meds before marginalized groups, but do institutions shift their foundational biases? Doubtful. The system may improve drug delivery pipelines, but social acceptance? That’s a greater mountain.
We also have to scrutinize the pharma industry’s motivations. Is this care, or calculated market expansion using social justice rhetoric?
charlise webster
July 30, 2025 at 14:53
To build off what’s been said, sometimes I feel such discussions get bogged down by jargon and platitudes. The article tries to strike a balance, but I found some parts overly simplistic for the complexities involved.
Disparities in PAH treatment aren’t just medical; they’re cultural, political, and economic. It’d be refreshing to see deeper dives into these nuances rather than broad statements. Maybe a series of patient interviews instead?
As much as I appreciate raising awareness, I’m also a bit skeptical about how much actually changes without upheaval.
Alec McCoy
August 1, 2025 at 22:26
I'm encouraged to see this topic gaining spotlight. Representation in healthcare matters immensely, and ambrisentan’s role in PAH treatment is critical, but bridging the gap requires holistic strategies. Training healthcare providers in LGBTQ+ cultural competence isn’t just 'nice to have' — it’s essential.
Also, it's important to remember intersectionality. LGBTQ+ folks often face compounded challenges when race, socioeconomic status, and disability enter the picture. Tailored approaches must be flexible, inclusive, and patient-centered.
Community advocacy, physician education, and policy reform have to move in tandem for sustained impact.
William Mack
August 3, 2025 at 07:46
Does anyone know if there's ongoing research specifically studying ambrisentan's efficacy or side effects tailored for LGBTQ+ patients? Like, are clinical trials making sure to include diverse sexual orientations and gender identities?
I think that would be a game changer. If pharmaceutical research continues to overlook these populations, the data just won't reflect true effectiveness or risks. Real inclusivity means all the way through R&D, not just marketing.
KAYLEE MCDONALD
August 4, 2025 at 11:33
Replying to the question about research inclusivity — great point! From what I’ve seen, medical trials often lack robust LGBTQ+ representation, so data can be skewed or incomplete.
This makes it harder for clinicians to confidently tailor treatments like ambrisentan. It's a vicious cycle: lack of data leads to hesitancy, which means fewer specific recommendations, further marginalizing the community.
We need more advocacy pressing trial designers to collect this data intentionally and respectfully.
Francisco Garcia
August 7, 2025 at 22:53
I want to highlight how mental health integration is another critical component. PAH itself is physically taxing, but when combined with the psychological stress from societal stigma and discrimination, treatment adherence and outcomes can suffer.
This article touches on systemic obstacles, but integrating mental health support into PAH care—especially for LGBTQ+ patients—deserves more emphasis.
Patrick Renneker
August 10, 2025 at 06:26
Allow me to pontificate at length on this matter: while the article commendably brings to light important issues related to LGBTQ+ disparities in PAH treatment, one must consider whether the focus on a drug like ambrisentan oversimplifies a problem entrenched in social determinants and institutional inertia. The pharmacological advancements, laudable as they are, cannot in isolation remedy the complex matrix of challenges faced by marginalized communities.
Moreover, the tacit suggestion that patient self-advocacy alone is a panacea risks shifting responsibility onto the vulnerable rather than institutional structures that perpetuate inequity. It behooves us to pursue systemic reforms with the same vigor as scientific innovation, lest we merely apply a superficial salve to a deep wound.
Evan Riley
August 17, 2025 at 02:20
Not to pour cold water, but sometimes I can't help but wonder whether the coverage of such topics serves any purpose beyond the surface. I mean, who really benefits when we talk about bridging gaps? Because if big pharma, bureaucrats, or insurance companies aren't being held accountable in concrete ways, are we just playing into their hands?
Also, with all this talk, is there any guarantee that these meds reach the people who need them most, without catch-22 obstacles? I smell a rat in many of these social justice healthcare pushes—profit often masquerades as progress.