Chronic Conditions: How to Adjust to Generic Maintenance Medications Without Compromising Your Health
Switching from a brand-name medication to a generic version for a chronic condition can feel scary. You’ve been taking the same pill for years. It works. You know how your body reacts to it. Then your pharmacy calls: "Your prescription is now generic. Your copay is $5 instead of $75." You’re relieved about the price-but nervous. Will it still work? Will you feel worse? Is this safe?
The short answer: For most people, yes, generics are just as safe and effective. But it’s not always simple. If you’re managing diabetes, high blood pressure, thyroid disease, depression, or asthma, and you’ve been handed a generic version of your maintenance medication, here’s what you need to know-straight from real-world data, patient experiences, and medical guidelines.
What Exactly Are Maintenance Medications?
Maintenance medications aren’t for quick fixes. They’re the drugs you take every day-sometimes for life-to control long-term conditions. These aren’t antibiotics for an infection or painkillers for a headache. They’re the pills that keep your blood sugar steady, your thyroid balanced, your blood pressure under control, or your asthma from flaring up.
Common examples include:
- Atorvastatin (for high cholesterol)
- Levothyroxine (for hypothyroidism)
- Metformin (for type 2 diabetes)
- Losartan or lisinopril (for high blood pressure)
- Sertraline or escitalopram (for depression and anxiety)
- Fluticasone inhalers (for asthma)
- Warfarin (for blood clot prevention)
These drugs are taken consistently. Missing a dose or switching brands can cause small but meaningful changes in how your body responds. That’s why switching to a generic version needs attention-even when it’s the right financial move.
Why Generics Are Just as Effective (Most of the Time)
The FDA doesn’t approve generics lightly. To get the green light, a generic drug must prove it delivers the exact same active ingredient, in the same strength, and at the same rate into your bloodstream as the brand-name version. This is called bioequivalence.
Here’s what that means in real numbers: The FDA requires that the generic’s absorption in your blood falls within 80% to 125% of the brand-name drug’s levels. That’s a wide enough range to account for normal body variation-but tight enough to ensure the effect is the same.
For most people, this works perfectly. In fact, 90% of all prescriptions filled in the U.S. are for generics. For chronic conditions, that number is around 85%. And here’s the kicker: Patients on generics are 12-15% more likely to stick with their medication because it’s affordable. That leads to 23% fewer hospital visits for complications like heart attacks, strokes, or diabetic emergencies.
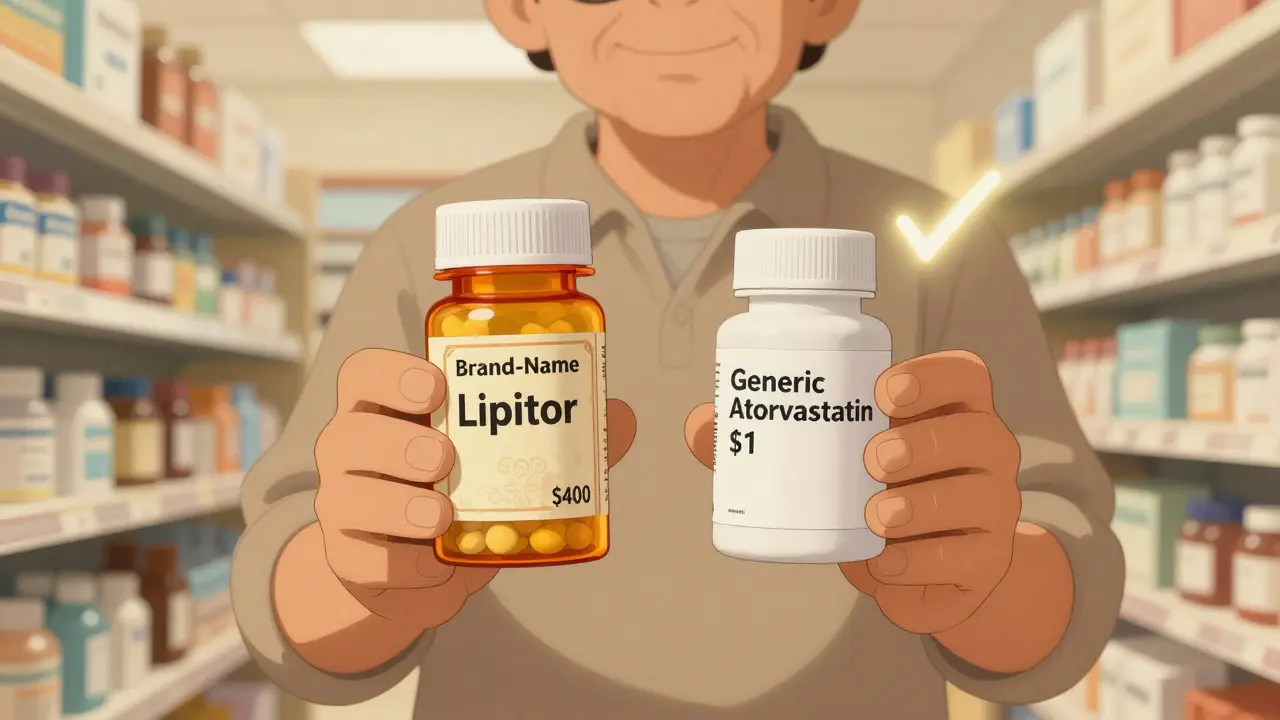
Cost difference? Stark. A 30-day supply of brand-name Lipitor (atorvastatin) used to cost nearly $400. The generic? Less than $1. For insulin, brand-name Lantus was $345. The authorized generic? Under $100. That’s not a minor savings-it’s life-changing for people on fixed incomes.
When Generics Can Cause Problems
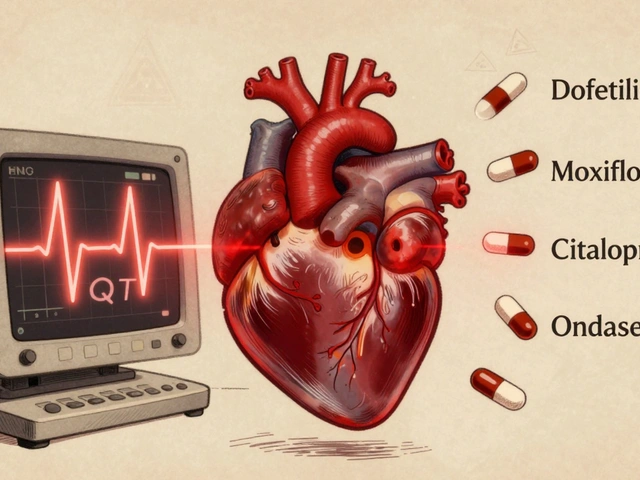
Not all medications are created equal when it comes to switching. Some drugs have a narrow therapeutic index. That means the difference between a dose that works and one that’s too high-or too low-is tiny. For these, even small changes in how your body absorbs the drug can throw things off.
These are the big ones:
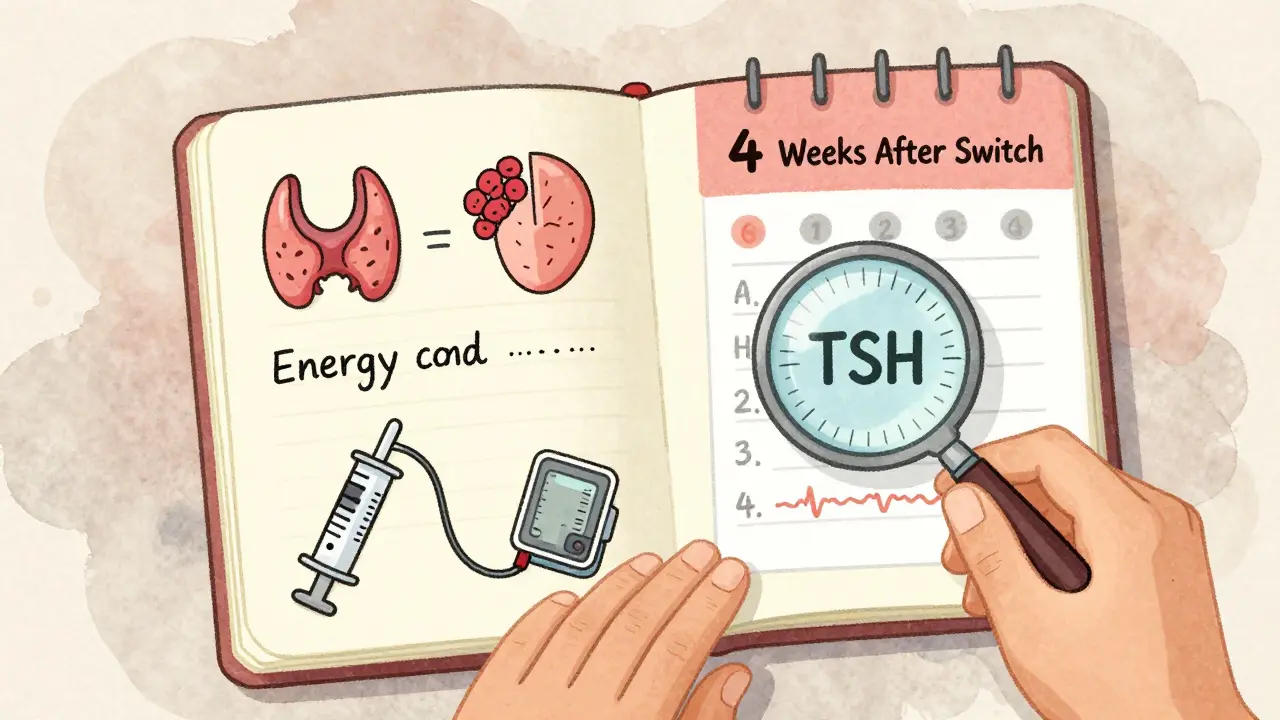
- Levothyroxine (for thyroid): Even small changes in absorption can cause your TSH levels to swing. Studies show 5-8% of patients have noticeable fluctuations when switching between generic manufacturers. That’s why many endocrinologists recommend sticking with the same brand or generic version once you’re stable.
- Warfarin (blood thinner): A slight change in absorption can increase your risk of clotting or bleeding. Many patients on warfarin are advised to stay on one version.
- Phenytoin (for seizures): Similar risks. Neurologists often prefer consistency here.
Also, some patients report issues with generic antidepressants. A 2023 survey by the National Alliance on Mental Illness found 34% of patients worried generics wouldn’t work as well-even though clinical trials show no difference. The problem? Placebo effect, yes-but also real differences in inactive ingredients like dyes or fillers that can affect gut absorption or cause mild side effects like nausea or headaches.
And then there’s the MS drug issue. Some patients report more fatigue or muscle spasms after switching from brand-name to generic disease-modifying therapies. But neurologists point out: MS symptoms naturally fluctuate. It’s hard to prove the drug changed-unless you’re tracking your symptoms daily.
What Patients Are Saying
Reddit threads, patient forums, and survey data tell a mixed story.
On r/Pharmacy, a thread about switching from Synthroid to generic levothyroxine got over 140 comments. Sixty-three percent said they felt worse-fatigue, brain fog, weight gain. Thirty-seven percent said they felt fine-or even better.
A Drugs.com survey of 2,450 people taking maintenance meds found:
- 41% noticed no difference at all
- 32% said the generic was cheaper and worked just as well
- 19% had minor side effects (headache, stomach upset) that faded in 2-4 weeks
- 8% stopped the generic because they felt it wasn’t working
And here’s something important: The people who felt worse? Most of them switched between different generic manufacturers. Not from brand to generic. From one generic to another.
That’s the real issue-not generics vs. brand. It’s switching manufacturers.
How to Make the Switch Safely
If your doctor or pharmacy switches you to a generic, here’s how to handle it without stress:
- Ask which generic you’re getting. Not all generics are made by the same company. Ask for the manufacturer name. Write it down.
- Don’t switch manufacturers unless you have to. If your first generic works, stick with it. Avoid swapping between different generic brands. Consistency matters more than the label.
- Track your symptoms. Use the FDA’s free Medication Tracker app-or a simple notebook. Note energy levels, sleep, mood, heart rate, weight, or any new symptoms. Do this for at least 30 days.
- Get a blood test if needed. For thyroid, kidney, liver, or blood thinner meds, ask your doctor to check levels 4-6 weeks after switching. TSH, INR, creatinine, or glucose levels can tell you if the drug is working the same way.
- Talk to your pharmacist. They know the fillers and dyes in each version. If you’re allergic to red dye or lactose, they can tell you if the generic contains it.
- Don’t panic if you feel off. Your body might just need 2-3 weeks to adjust. But if symptoms persist beyond a month, or get worse, call your doctor.
What Your Insurance and Doctor Can Do
Most insurance plans now require you to try generics first. Blue Cross Blue Shield of Kansas, for example, mandates generic substitution for all maintenance drugs unless there’s a medical reason not to.
But you can fight back-if you have to. If you’ve tried two different generics and still feel unwell, your doctor can file a prior authorization request for the brand-name drug. Approval rates are low-only 14%-but it’s possible if you have documented evidence: lab results, symptom logs, or a letter from your specialist.
Some drugs, like inhalers for asthma, require special care. The American Lung Association recommends working with a respiratory therapist when switching. Sometimes, it’s not the drug-it’s how you’re using the inhaler. A small technique change can mimic a drug failure.
What’s Changing in 2026
The FDA is cracking down on generic quality. Under its GDUFA III program (started in 2022), manufacturers of complex generics-like inhalers, patches, and injectables-must now prove their products work just as well as the brand in real-world conditions.
Also, new generics are hitting the market fast. In early 2023, the FDA approved the first generic versions of Jardiance (for diabetes) and Entresto (for heart failure). More are coming. Eliquis, a top blood thinner, loses its patent in 2026. That means prices could drop by 90%.
And the Inflation Reduction Act now caps insulin at $35 per month for Medicare patients. That’s accelerating the shift to generics and biosimilars.
Bottom Line: You Can Trust Generics-If You Stay Smart
For the vast majority of people with chronic conditions, switching to a generic maintenance medication is not just safe-it’s smart. It saves money. It improves adherence. It reduces hospital visits. And it doesn’t compromise your health.
But trust doesn’t mean ignorance. Stay involved. Know which generic you’re taking. Track your body’s response. Don’t switch manufacturers unless you have to. And if something feels off-speak up. Your doctor and pharmacist are your allies.
Generics aren’t second-rate. They’re science-backed, FDA-approved, and proven to work. The only difference? The price tag-and your peace of mind.




10 Comments
Jessie Ann Lambrecht
January 6, 2026 at 16:32
Let me tell you something-I switched my levothyroxine from Synthroid to a generic last year and barely noticed a difference. My TSH stayed rock solid, and I saved $200 a month. The key? Stick with the same generic manufacturer. I got mine from Teva and never looked back. Your body isn’t a magic box-it’s chemistry. And if the FDA says it’s bioequivalent, trust the science, not the fear-mongering.
Aparna karwande
January 7, 2026 at 06:25
Oh please. You people treat generics like they’re some kind of sacred cow. In India, we’ve been using generics for decades-because we have to. And let me tell you, some of them are pure garbage. Pills that crumble in your hand, fillers made from who-knows-what. The FDA? A joke. Big Pharma bribes regulators. You think they care if your thyroid swings? No. They care about the bottom line. And you’re just another data point.
Kyle King
January 8, 2026 at 11:40
Wait… so you’re telling me the government didn’t just let Big Pharma create a monopoly on thyroid meds so they could jack up prices… and then suddenly say ‘oh wait here’s a generic’… and we’re supposed to believe this isn’t a controlled experiment on the American public? 🤔 I’ve got a cousin who went from 100mcg Synthroid to a generic and started having panic attacks. Coincidence? Or did the fillers trigger a hidden immune response? The FDA doesn’t test for that. They test for ‘bioequivalence’-whatever that means when your brain’s on fire.
Rachel Steward
January 9, 2026 at 16:44
Here’s the uncomfortable truth nobody wants to admit: the placebo effect isn’t just psychological-it’s physiological. Your brain expects a certain pill, with a certain color, a certain shape, a certain brand logo-and when that’s gone, your autonomic nervous system glitches. That’s why people report side effects even when the active ingredient is identical. The body doesn’t just absorb molecules-it absorbs meaning. And when meaning shifts, physiology follows. So yes, generics work… but not because of chemistry alone. Because of belief. And belief is the most powerful drug of all.
Also, the 80–125% bioequivalence range? That’s not ‘tight.’ That’s a canyon. Two people taking the same generic could be absorbing drugs at 82% and 124% respectively. That’s not equivalence. That’s a lottery.
Elen Pihlap
January 11, 2026 at 07:11
i just switched to generic sertraline and i feel like a zombie now. like my emotions are muted. like i’m watching my life through a foggy window. i dont know if its the drug or if im just depressed about the switch. but i miss feeling things. even the bad ones. why does everything have to be cheaper?
Sai Ganesh
January 12, 2026 at 03:00
My father has been on warfarin for 12 years. He switched from brand to generic once, and his INR went from 2.3 to 4.8 in three weeks. We almost lost him to internal bleeding. Now he only takes the same generic from one company. I’ve seen what happens when you treat life-saving medicine like a commodity. It’s not about cost. It’s about control. And your body doesn’t care about your insurance plan.
LALITA KUDIYA
January 12, 2026 at 11:13
generics are fine if you stay with one brand. i switched from brand to generic and felt nothing. then my pharmacy changed to a different generic and i got headaches for two weeks. went back to the first one and boom, fine. its not the generic its the switching. peace out 🌿
Poppy Newman
January 14, 2026 at 01:10
Just had to comment because I’m a pharmacist in London and we see this ALL the time. The real issue? Patients switching between generics because the pharmacy changes suppliers every month. It’s not the generic-it’s the chaos. I always tell patients: pick one, stick with it, and write down the manufacturer name. If your blood pressure starts acting up? Check the pill’s imprint. It’s not magic. It’s logistics. 💊✨
Anthony Capunong
January 15, 2026 at 04:23
Let’s be real. This whole ‘generics are fine’ narrative is a corporate lie. The FDA lets companies use fillers that are banned in Europe. Dyes linked to ADHD. Lactose in pills for people who are lactose intolerant. And you think your insurance cares? They don’t. They just want you to stop complaining and take the cheapest thing on the shelf. This isn’t healthcare. It’s cost-shifting with a smiley face.
Kamlesh Chauhan
January 15, 2026 at 13:37
bro i took generic metformin and my stomach felt like it was being eaten by ants for a week. i went back to brand and boom. no more pain. why do we even have to go through this. its 2024. why cant we just get the good stuff without fighting our own government and insurance companies. i just want to live without my guts screaming at me every morning