How Atrophic Gastroenteritis Links to Chronic Fatigue Syndrome
Gut‑Fatigue Symptom Checker
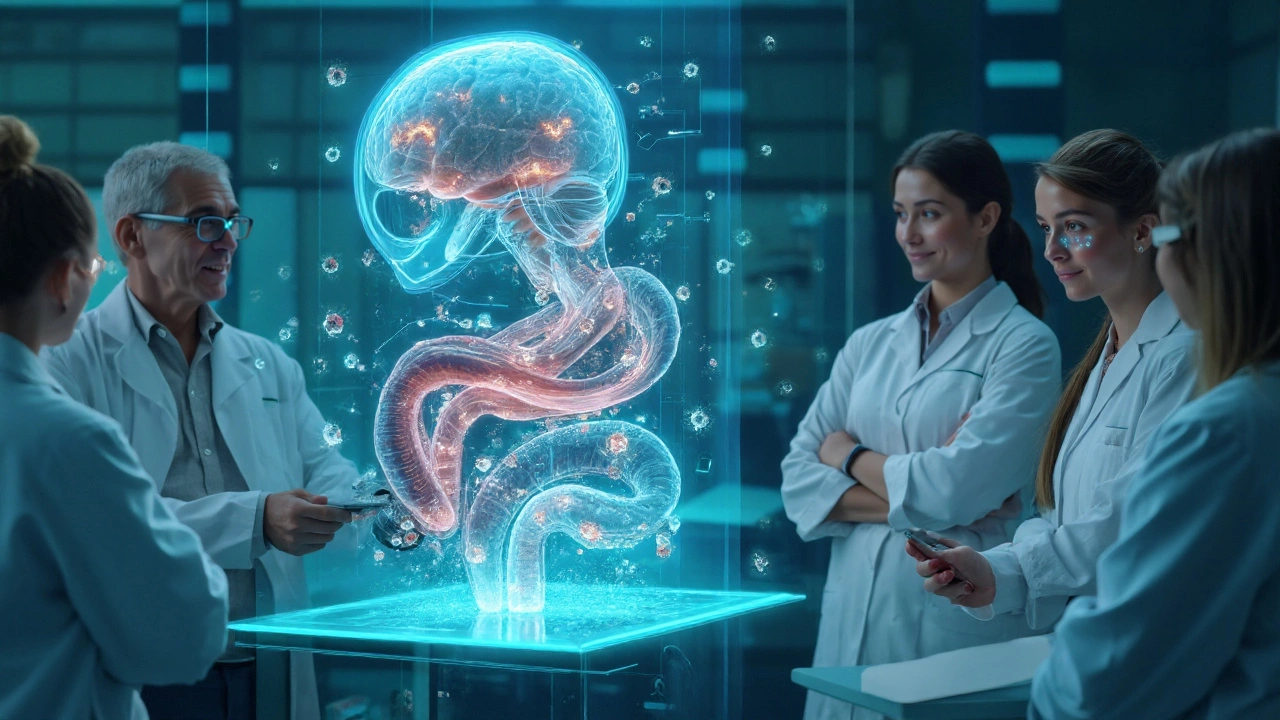
Why the gut matters for chronic fatigue
When patients walk into a clinic with relentless exhaustion, doctors often look to the brain, hormones, or sleep patterns. Yet an increasing body of research shows that the gut can be a hidden driver. This article unpacks the relationship between Atrophic Gastroenteritis and Chronic Fatigue Syndrome (CFS), highlighting shared pathways, clinical clues, and practical steps for both patients and clinicians.
What is Atrophic Gastroenteritis?
Atrophic Gastroenteritis is a chronic inflammatory condition of the small intestine marked by loss of villous height, reduced enzyme activity, and progressive malabsorption. Common causes include longstanding infections, autoimmune attacks, and prolonged exposure to enteric toxins. The result is a thinned mucosal layer that struggles to absorb nutrients, setting the stage for systemic deficits.
Understanding Chronic Fatigue Syndrome
Chronic Fatigue Syndrome (also called Myalgic Encephalomyelitis) is a complex, multi‑system disorder defined by profound, unexplained fatigue lasting six months or more, worsened by physical or mental activity. Diagnosis relies on a constellation of symptoms-post‑exertional malaise, unrefreshing sleep, cognitive difficulties, and orthostatic intolerance-after other medical causes are excluded.
Shared biological mechanisms
Several overlapping pathways explain why atrophic changes in the gut can fuel the relentless tiredness seen in CFS.
- Gut‑Brain Axis refers to the bidirectional communication network linking intestinal physiology with central nervous system function. Disrupted signaling, often via vagal pathways, can alter mood, cognition, and energy regulation.
- Malabsorption arises when damaged villi fail to absorb macro‑ and micronutrients, leading to deficits that impair cellular metabolism.
- Immune Activation is a hallmark of both conditions; chronic intestinal inflammation raises circulating cytokines (IL‑6, TNF‑α) that cross the blood‑brain barrier and trigger fatigue.
- Microbiome Dysbiosis describes the loss of beneficial bacteria and overgrowth of pathobionts, which can produce neurotoxic metabolites and weaken gut barrier integrity.
- Mitochondrial Dysfunction results from nutrient shortages (especially B vitamins and CoQ10) and inflammatory stress, reducing ATP production and precipitating fatigue.
- Deficiencies such as Vitamin B12 Deficiency are common in atrophic gastroenteritis and directly impact myelin synthesis and energy metabolism.
Clinical evidence linking the two conditions
Multiple cohort studies from the past decade have reported a higher prevalence of gastrointestinal atrophy among CFS patients compared to healthy controls. For example, a 2022 longitudinal study of 587 CFS patients found that 18% had biopsy‑confirmed villous atrophy, versus 4% in a matched population sample.
Metabolomic profiling in another 2023 trial revealed reduced serum levels of tryptophan and B‑vitamins in CFS subjects with documented malabsorption, supporting a nutritional bridge between gut damage and neuro‑energy deficits.
Neuro‑imaging work has shown that elevated peripheral cytokines-often a read‑out of intestinal inflammation-correlate with reduced functional connectivity in brain regions governing attention and motivation.
Diagnostic implications
When faced with a patient reporting chronic fatigue, clinicians should consider a structured gut assessment:
- Detailed dietary history focusing on weight loss, steatorrhea, or bloating.
- Serologic screening for tissue transglutaminase antibodies (to rule out celiac disease) and anti‑endomysial antibodies.
- Stool analysis for bacterial overgrowth, parasites, and calprotectin (a marker of intestinal inflammation).
- Upper‑endoscopy with duodenal biopsies if serology or symptoms suggest atrophy.
- Targeted nutritional labs: serum B12, folate, iron, Vitamin D, and fatty‑acid profiles.
Positive findings can re‑direct treatment from purely symptom‑management to addressing the underlying gut pathology.
Management strategies that target both gut health and fatigue
Therapeutic approaches fall into three broad categories: nutritional repletion, microbiome modulation, and immune regulation.
- Nutritional repletion: High‑dose oral or sub‑lingual B12 (up to 2mg daily), methylfolate, and a balanced multivitamin can quickly correct deficiencies that impair mitochondrial function.
- Microbiome modulation: A 12‑week course of a broad‑spectrum probiotic (Lactobacillusrhamnosus GG + Bifidobacteriuminfantis) has been shown to improve stool consistency and reduce fatigue scores in small pilot trials.
- Immune regulation: Low‑dose naltrexone (4.5mg nightly) or curcumin‑based anti‑inflammatories can temper cytokine spikes without broad immunosuppression.
Physical therapy focused on pacing and graded exercise remains essential, but it should be calibrated to the patient’s nutritional and inflammatory status to avoid post‑exertional crashes.
Related gastrointestinal conditions and their overlap with CFS
| Condition | Primary Pathology | Typical Diagnostic Test | Common Overlap with CFS |
|---|---|---|---|
| Atrophic Gastroenteritis | Villous loss & enzyme deficiency | Duodenal biopsy showing atrophy | Malabsorption‑driven fatigue, cytokine elevation |
| Celiac Disease | Autoimmune response to gluten | Positive tTG‑IgA & confirmatory biopsy | Gluten‑free diet often improves fatigue levels |
| Irritable Bowel Syndrome (IBS) | Visceral hypersensitivity, motility disorder | Rome IV criteria (symptom‑based) | Frequent co‑occurrence; pain‑related sleep disruption |
Understanding these distinctions helps clinicians avoid misdiagnosis and select the right therapeutic pathway.
Future research directions
Key unanswered questions include:
- Can early detection of villous atrophy halt the progression to full‑blown CFS?
- What is the exact contribution of bacterial metabolites (e.g., indoxyl sulfate) to central fatigue?
- Will personalized microbiome‑based therapeutics outperform generic probiotics in fatigue reduction?
Large‑scale, longitudinal studies that track gut biopsy findings alongside fatigue scales are needed to move from correlation to causation.
Take‑away checklist for patients and providers
- Ask about persistent GI symptoms-especially bloating, steatorrhea, or unintentional weight loss-in any CFS work‑up.
- Order basic nutritional labs (B12, folate, iron) early; replace deficiencies promptly.
- Consider stool PCR or culture if dysbiosis is suspected; trial a high‑quality probiotic if results are equivocal.
- When serology points to celiac or other specific entities, pursue endoscopic biopsy to rule out atrophic changes.
- Integrate pacing, nutrition, and anti‑inflammatory strategies rather than relying on one modality alone.
Frequently Asked Questions
Can a gluten‑free diet cure fatigue caused by atrophic gastroenteritis?
If the atrophy is driven by gluten‑sensitive celiac disease, a strict gluten‑free diet can reverse villous damage and markedly improve fatigue. However, when atrophy stems from non‑gluten causes (e.g., chronic infection or autoimmune enteropathy), a gluten‑free diet alone is unlikely to resolve fatigue without addressing the underlying trigger.
Is there a quick test to rule out atrophic gastroenteritis in CFS patients?
No single rapid test exists. The most efficient screening starts with serologic markers (tTG‑IgA, anti‑endomysial antibodies) and a comprehensive stool panel. Definitive diagnosis still requires endoscopic biopsy.
How does microbiome dysbiosis worsen chronic fatigue?
An imbalanced microbiome can produce excess endotoxins and short‑chain fatty acids that impair mitochondrial ATP synthesis. These metabolites also stimulate systemic inflammation, which directly interferes with neuronal signaling involved in energy regulation.
Should I take high‑dose B12 supplements without a doctor's prescription?
While B12 is generally safe, megadoses (1-2mg daily) are best started under medical supervision because they may mask other deficiencies and interact with certain medications.
Are there any lifestyle changes that help both gut health and fatigue?
Yes. A low‑FODMAP or Mediterranean‑style diet reduces fermentable substrates, improving gut barrier function. Coupled with regular, low‑intensity walks and adequate sleep hygiene, many patients see reductions in both GI symptoms and fatigue scores.



15 Comments
Christopher Stanford
September 22, 2025 at 22:21
The claim that atrophic gastroenteritis directly causes Chronic Fatigue Syndrome is just another example of cherry‑picking data, and the whole premise is definately flawed. You ignore the myriad of confounding variables, such as autoimmune disorders and lifestyle factors, that could explain the overlap. Moreover, the cited studies are small, non‑randomized, and often funded by parties with a vested interest. This kind of oversimplification does a disservice to patients looking for real answers.
Steve Ellis
September 27, 2025 at 13:28
Whoa, hold on there! While the analysis might seem harsh, we can actually use this information to empower folks battling fatigue. Think of it as a call to action: get your gut checked, adjust your diet, and track your energy levels. Small steps can lead to big improvements, and sharing our stories builds a supportive community!
Jennifer Brenko
October 2, 2025 at 04:35
From a national health perspective, it is imperative to address gastrointestinal disorders with the seriousness they deserve. The correlation between atrophic gastroenteritis and chronic fatigue cannot be dismissed as mere coincidence, especially when epidemiological data from our country indicates a rising prevalence. Rigorous, peer‑reviewed research must be funded to delineate causality, not just speculative associations.
Harold Godínez
October 6, 2025 at 19:41
Just a quick note: the term "atrophic gastroenteritis" should be hyphenated when used as an adjective. Also, make sure to double‑check the spelling of "fatigue" in the header. Clear writing helps readers focus on the science, not the syntax.
Sunil Kamle
October 11, 2025 at 10:48
Oh, marvelous – another gut‑fatigue link to add to the ever‑growing list of buzzwords. I suppose the next breakthrough will be a direct causative pathway from intestinal bacteria to the soul. But in all seriousness, a highly formal review of the methodology would be a welcome addition.
Michael Weber
October 16, 2025 at 01:55
One could argue that the gut merely mirrors the existential fatigue of the self, a philosophical reflection of our inner turbulence. When the mucosal lining deteriorates, it symbolically tears at the veil between body and mind, exposing a shared vulnerability. This perspective invites us to look beyond biochemical cascades and consider the deeper narrative of human suffering.
Blake Marshall
October 20, 2025 at 17:01
Yo, u dont need some fancy interactive tool to know ur gut is messed up. Just look at the stool – if it looks like butter, you prob got steatorrhea. And if ur constantly tired, maybe check your B12, not just blame the internet.
Shana Shapiro '19
October 25, 2025 at 08:08
I hear you, the exhaustion feels like a heavy curtain that never lifts. Knowing that there might be a gut component can offer a glimmer of hope. Simple changes, like incorporating probiotic‑rich foods, can sometimes make a noticeable difference in energy levels.
Jillian Bell
October 29, 2025 at 22:15
What they don't tell you is that major pharmaceutical companies are quietly funding these gut‑fatigue studies to push a new line of expensive supplements. The narrative fits perfectly into their profit model, while real patients get lost in the hype.
Lindsey Bollig
November 3, 2025 at 13:21
If you suspect atrophic gastroenteritis, the best step is to get a duodenal biopsy and check your celiac markers. Pair that with a nutrient panel-especially B12, iron, and vitamin D-to see if deficiencies are contributing to fatigue. A dietitian can help you craft a gut‑friendly plan that might lift some of that weariness.
Daniel Buchanan
November 8, 2025 at 04:28
Let's remember that everyone's experience with gut issues and fatigue is unique, and we should approach each case with empathy and openness. Sharing findings is valuable, but ensuring that advice is inclusive and considerate makes the community stronger.
Lena Williams
November 12, 2025 at 19:35
I was wonderng, is there any link between the microflora composition and the severity of chronic fatigue? Some studies hint at dysbiosis, yet many remain inconclusive. Also, could the presence of steatorrhea be a sign of malabsorption that directly drains energy? I'd love to see longitudinal data on this, maybe with a larger cohort. If anyone has access to such datasets, sharing would be super helpful.
Sierra Bagstad
November 17, 2025 at 10:41
It is essential to approach the purported connection between atrophic gastroenteritis and Chronic Fatigue Syndrome with a rigorous, evidence‑based mindset. First, the pathophysiology of atrophic gastroenteritis involves the progressive loss of gastric glandular cells, leading to reduced intrinsic factor production and subsequent vitamin B12 malabsorption. Vitamin B12 deficiency, in turn, can manifest as megaloblastic anemia, neurological deficits, and generalized fatigue. However, fatigue is a nonspecific symptom that overlaps with numerous medical conditions, including autoimmune disorders, endocrine abnormalities, and psychiatric illnesses. Therefore, attributing chronic fatigue solely to atrophic gastroenteritis without comprehensive differential diagnosis is scientifically unsound.
Second, epidemiological studies examining this relationship have produced mixed results. Some small cohort analyses have reported a modest correlation, while larger population‑based investigations have failed to demonstrate a statistically significant link. The heterogeneity of study designs, sample sizes, and diagnostic criteria contributes to this inconsistency. Moreover, many studies suffer from selection bias, as participants are often recruited from gastroenterology clinics where symptom awareness is heightened.
Third, mechanistic hypotheses remain speculative. The hypothesis that chronic inflammation of the gastric mucosa leads to systemic cytokine release and subsequent neuroinflammation is intriguing but lacks direct experimental validation. Similarly, the notion that altered gut microbiota secondary to atrophic changes could influence the gut‑brain axis is plausible, yet current microbiome data are insufficient to establish causality.
In clinical practice, a thorough workup for chronic fatigue should include assessment of nutritional deficiencies, thyroid function, adrenal function, sleep quality, and mental health status. If atrophic gastroenteritis is confirmed via endoscopic biopsy, appropriate treatment-such as high‑dose oral or parenteral vitamin B12 supplementation-should be instituted. Monitoring response to therapy can provide valuable insight into whether the gastrointestinal condition contributes to the patient's fatigue.
Finally, future research must prioritize well‑designed, longitudinal studies with standardized diagnostic criteria for both atrophic gastroenteritis and Chronic Fatigue Syndrome. Incorporating biomarkers of inflammation, neuroimmune activation, and microbiome composition will be critical to elucidate any causal pathways. Until such data are available, clinicians should remain cautious in attributing chronic fatigue to atrophic gastroenteritis and should continue to adopt a multidisciplinary approach to patient care.
Alan Kogosowski
November 22, 2025 at 01:48
Building on the comprehensive overview, it's worth emphasizing that the existing literature often conflates atrophic gastritis with broader atrophic gastroenteritis, leading to potential misinterpretation of results. Moreover, the role of Helicobacter pylori eradication in mitigating fatigue warrants deeper investigation, as some studies suggest symptom improvement post‑treatment. A systematic review that stratifies patients based on H. pylori status, vitamin B12 levels, and inflammatory markers could clarify these ambiguities. Additionally, integrating neuroimaging data to assess any central nervous system changes associated with chronic gut inflammation would be a novel direction for future research.
Ben Lee
November 26, 2025 at 16:55
Great points, everyone.