How to Read Medication Labels: Understand Dosage and Directions for Safe Use
Medication labels aren’t just paperwork-they’re your safety net.
Every pill bottle, inhaler box, or liquid medicine container has a label that tells you exactly how to use it safely. But most people skip reading it. They grab the bottle, guess the dose, and hope for the best. That’s how mistakes happen. Every year, over 1.5 million preventable drug errors occur in the U.S., and half of them come from people misunderstanding the label. You don’t need a medical degree to read it right. You just need to know what to look for.
What’s on a prescription label?
Prescription labels follow strict federal rules. They must include your name, the drug name, the strength (like 500mg), how many pills are in the bottle, and clear instructions on how to take it. But the most important part is Section 2: Dosage and Administration. This isn’t just ‘take one pill daily.’ It tells you when to take it (with food? on an empty stomach?), how often (every 6 hours? once a day?), and what to do if you miss a dose. It also warns you about interactions-like if you’re on blood pressure meds, this drug might make them work too well. If you have kidney or liver issues, the label will say if you need a lower dose. Skip this part, and you could be in danger.
What’s on an OTC (over-the-counter) label?
OTC meds-like Tylenol, Advil, or allergy pills-use the Drug Facts format. It’s standardized, so it looks the same no matter the brand. There are seven key sections:
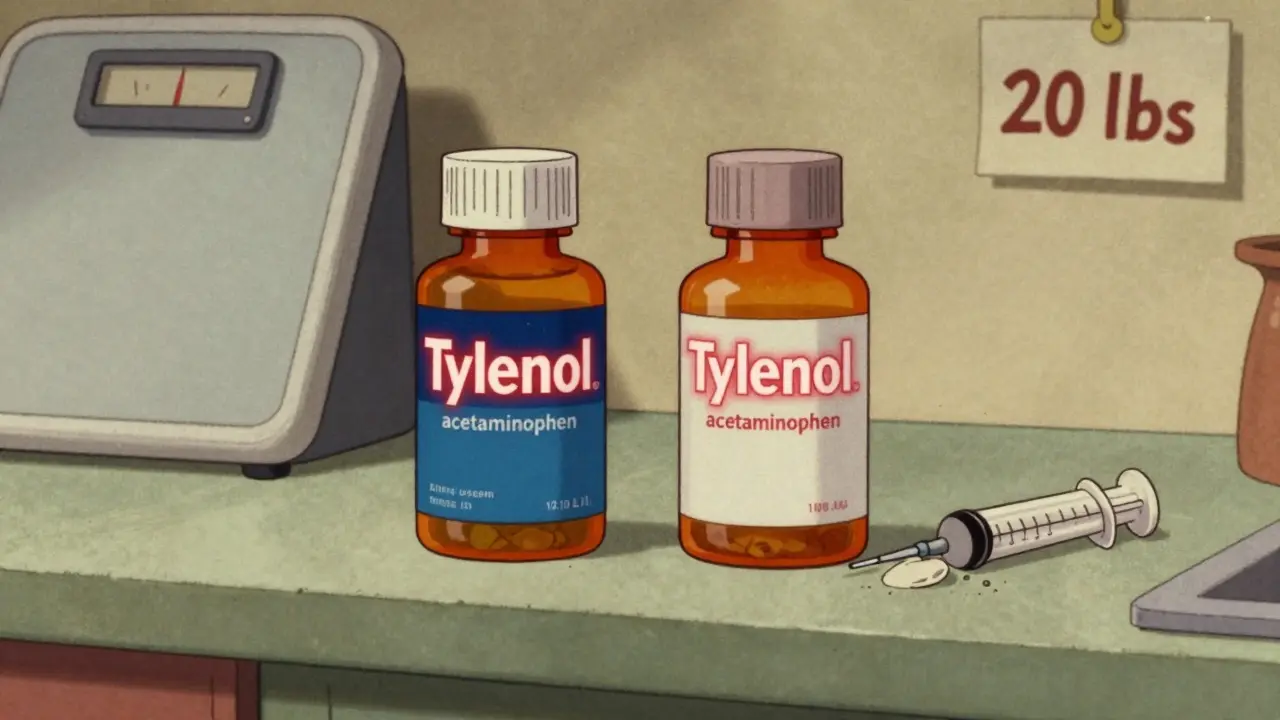
- Active Ingredient: This is the medicine itself. If you’re taking more than one OTC product, check this first. Many cold and flu pills contain acetaminophen. Taking two of them could mean you’ve hit the max safe dose-5,000mg a day-and risk liver damage.
- Purpose: What the drug does. Is it a pain reliever? A sleep aid? A decongestant?
- Uses: What symptoms it treats. Don’t assume it works for something not listed.
- Warnings: This is where most people skip. It tells you who shouldn’t take it (pregnant women? people with asthma?), what side effects to watch for, and when to call a doctor.
- Dosage: This is the core. It says how much to take, how often, and the max per day. Example: ‘Take 2 tablets every 4 to 6 hours. Do not exceed 8 tablets in 24 hours.’ That’s not a suggestion-it’s a limit.
- Inactive Ingredients: These are fillers, dyes, or flavorings. If you’re allergic to sulfa, dye, or gluten, check here.
- Expiration Date: Expired meds don’t just lose strength-they can break down into harmful substances. Don’t use them.
Why dosage isn’t just ‘one pill’
Many people think dosage means ‘one pill.’ But it’s more complex. Liquid meds are especially tricky. A label might say: ‘350 mg per 5 mL’. That means each teaspoon (5 mL) has 350 mg. If your doctor ordered 700 mg, you need two teaspoons-not one. People often guess. They use kitchen spoons. That’s dangerous. A teaspoon from your kitchen can hold anywhere from 2.5 mL to 7.3 mL. That’s a 200% difference. Always use the measuring cup or syringe that came with the medicine. If it didn’t come with one, ask the pharmacy for one. They’ll give it to you free.
For kids, weight matters more than age. A 20-pound baby needs a different dose than a 40-pound child-even if they’re both 2 years old. If the label says ‘based on weight,’ you need to know your child’s exact weight in pounds or kilograms. Don’t guess. Weigh them if you’re unsure.
Common mistakes-and how to avoid them
Here’s what most people get wrong:
- Taking two meds with the same active ingredient. Example: You take Tylenol for a headache, then take a cold medicine that also has acetaminophen. You’ve just doubled your dose. Always check the ‘Active Ingredient’ section on every label.
- Ignoring warnings. 47% of people don’t read them. If the label says ‘avoid alcohol’ or ‘may cause drowsiness,’ it’s not a suggestion. It’s a safety rule.
- Assuming ‘as needed’ means ‘whenever I feel like it.’ ‘Take as needed for pain’ doesn’t mean ‘take every hour.’ It means take only when pain is present, and never more than the max daily limit.
- Using old prescriptions. If your doctor changed your dose last month, don’t use the old bottle. Labels change. Always check the current one.
What to do if you’re confused
Don’t guess. Don’t ask a friend. Don’t Google it and pick the first answer. Call your pharmacist. They’re trained to explain labels in plain language. If you’re on multiple meds, ask for a medication review. Many pharmacies offer this for free. They’ll look at all your pills, check for interactions, and tell you exactly what to take and when.
For high-risk drugs-like insulin, blood thinners, or opioids-the pharmacy is required to give you a separate Medication Guide. These are printed booklets with step-by-step instructions. Read them. Keep them. They’re not optional.
The future of medication labels
Labels are getting smarter. By 2024, some prescriptions will have QR codes. Scan it with your phone, and you’ll get a video showing how to take the medicine, an interactive dosage calculator, and a list of side effects in plain language. The FDA is pushing for this because studies show it cuts errors by 37%. Color-coding for high-alert drugs is also coming. Think red for opioids, yellow for insulin-so you can spot danger at a glance.
Five steps to read any label safely
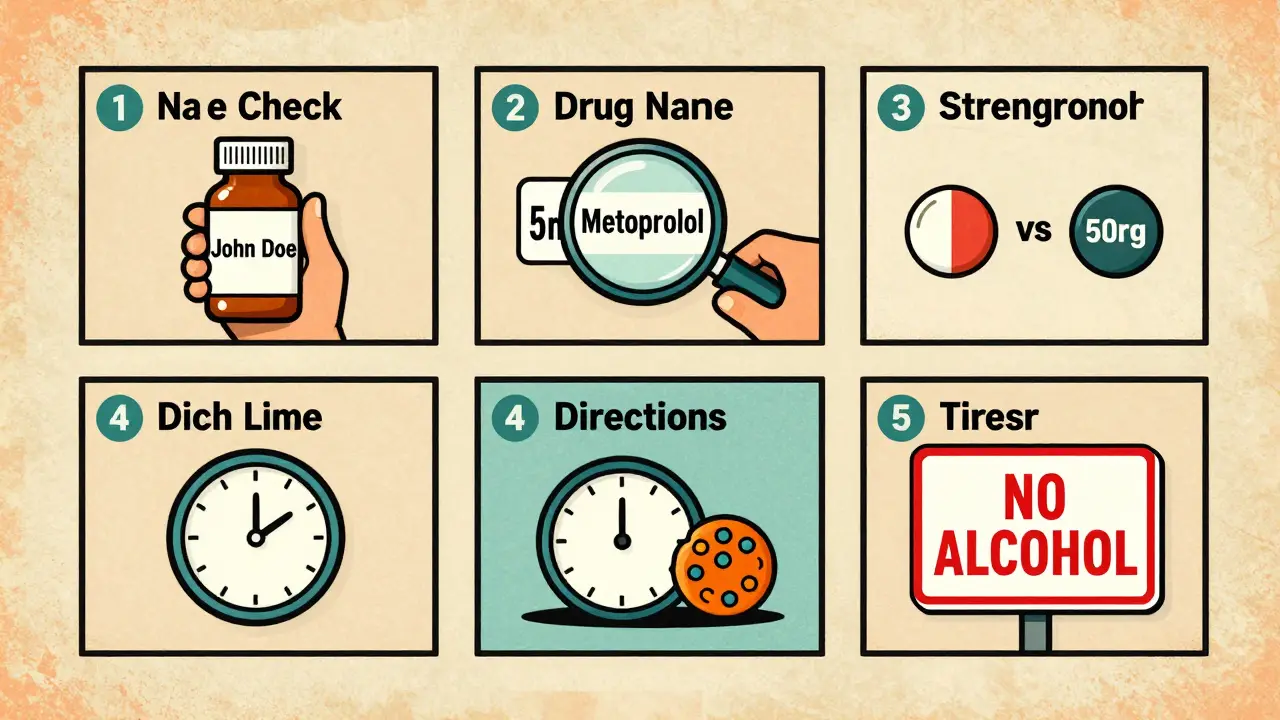
- Check your name. Make sure it’s yours. Mix-ups happen, especially in hospitals or pharmacies.
- Match the drug name. Is it spelled right? Is it the one your doctor prescribed?
- Confirm the strength. Is it 5mg or 50mg? A mistake here can be deadly.
- Read the directions. How many times a day? With food? At bedtime?
- Scan the warnings. Are there food, alcohol, or activity restrictions? Any red flags?
If you do these five steps every time you pick up a new prescription or OTC medicine, you’ve just cut your risk of a dangerous error by more than 80%.
Why this matters more than you think
Medication errors don’t just cause side effects-they send people to the ER. In 2022, 27% of medication-related ER visits were from people misunderstanding dosage. That’s not a rare accident. It’s a pattern. And it’s avoidable. You don’t need to be a doctor. You just need to take five minutes. Read the label. Ask one question. Save your life.
What should I do if I can’t read the label?
If the print is too small or blurry, ask your pharmacist for a large-print version. Many pharmacies offer this for free. You can also request an audio version or a translated label if you speak another language. Don’t try to guess the dosage. Always get help before taking the medicine.
Can I trust the expiration date on my medicine?
Yes, but with a caveat. Manufacturer expiration dates are tested and reliable. Pharmacy-labeled expiration dates for prescriptions are usually one year from when the bottle was filled. After that, the medicine may lose strength. Never use expired insulin, antibiotics, or nitroglycerin-they can become dangerous. For most other meds, using them a few months past the date isn’t usually harmful, but it’s not guaranteed to work.
Why do some labels say ‘take with food’ and others say ‘take on an empty stomach’?
Some drugs are absorbed better with food-it helps them enter your bloodstream. Others can irritate your stomach if taken without food. Some need an empty stomach so food doesn’t block absorption. Always follow the label. Taking a drug the wrong way can make it useless or cause side effects.
What if I accidentally take too much?
Call Poison Control at 1-800-222-1222 immediately. Don’t wait for symptoms. Even if you feel fine, some overdoses take hours to show up. Have the medicine bottle ready so you can tell them the exact name and dose you took.
Are generic drugs labeled the same way as brand names?
Yes. By law, generic drugs must have the same active ingredient, strength, dosage form, and directions as the brand name. The label may look different, but the key info-dosage, warnings, and instructions-is identical. You can safely switch between them as long as the active ingredient and dose match.







16 Comments
Trevor Whipple
January 13, 2026 at 03:07
ok but like… why does every label have tiny ass print? my grandpa can’t read it and neither can i after 3 cups of coffee. also why is ‘acetaminophen’ spelled like a spell from harry potter? it’s tylenol. just say tylenol. and stop making us decode medical latin. i’m not a pharmacist, i’m just trying not to die.
Lethabo Phalafala
January 13, 2026 at 12:23
I just lost my aunt last year because she took two cold meds that both had acetaminophen. She didn’t read the label. She trusted the bottle. And now she’s gone. This post? It’s not just info. It’s a lifeline. Please. For the love of everyone you know who’s ever been sick-read the damn label. I’m not yelling. I’m begging.
Lance Nickie
January 14, 2026 at 15:13
lol the FDA doesn’t care. they’re too busy regulating avocado toast.
Milla Masliy
January 16, 2026 at 10:28
I’m from the U.S. but my mom’s from Mexico and she used to read every label out loud in Spanish before taking anything. She said, ‘If you don’t understand it, you’re not taking it.’ I’ve carried that with me. Even when I’m stressed, I pause. Read. Ask. It’s not extra work-it’s self-respect.
Damario Brown
January 17, 2026 at 12:49
you’re all missing the real issue. the pharmaceutical industry *wants* you to mess up. more ER visits = more profit. they design labels to be confusing. the ‘active ingredient’ section? buried. the warnings? in 6pt font. they’re not trying to help you-they’re trying to protect themselves from lawsuits while you overdose on ibuprofen because you thought ‘every 6 hours’ meant ‘whenever I feel like it.’
and don’t even get me started on how they use ‘as needed’ as a loophole to sell more pills. it’s predatory capitalism wrapped in a white pill.
sam abas
January 18, 2026 at 00:19
look, i get it. reading labels is a chore. but let’s be real-most people don’t even know what ‘QID’ means. or ‘PO.’ or ‘PRN.’ and honestly? the FDA should just make everything pictogram-based. like a traffic light system: green = safe, yellow = caution, red = don’t touch. why are we still using words? we’re a species that communicates with memes. stop pretending we’re 19th-century pharmacists. also, why do all the warnings say ‘may cause drowsiness’ like it’s a bonus feature? it’s not a tea. it’s a chemical that knocks you out. call it what it is.
and the QR code thing? cool. but what about people without smartphones? or older folks who think ‘scan’ is a type of fish? this isn’t progress. it’s exclusion dressed up as innovation.
also, i’ve seen people use a tablespoon for liquid meds. a TABLESPOON. that’s like 15ml. if the dose is 5ml? congrats, you just gave your kid 3x the lethal dose. and no, the pharmacy won’t send you a syringe unless you ask. they assume you’re competent. we’re not. we’re all just winging it.
and why is ‘inactive ingredients’ even a thing? who cares if it has titanium dioxide? unless you’re allergic to glitter. then yes, i care. but no one ever says that. it’s all ‘may contain traces of soy.’ like, cool. i’m not a peanut. i’m just trying to sleep.
and the expiration date? i’ve got a bottle of amoxicillin from 2018. it’s still in the cabinet. i didn’t throw it out because ‘what if i need it?’ and now i’m terrified i’m gonna accidentally give it to my dog. also, why do some labels say ‘keep refrigerated’ and others say ‘store at room temp’? who decided this? a wizard? a committee of drunk chemists? i need answers.
and don’t even get me started on generics. they look different. same active ingredient? sure. but why does the generic one make me feel like i swallowed a battery? is it the dye? the filler? the soul of the person who packed it? i don’t know. but i know i hate it. and no one tells me why.
and why is the dosage chart for kids based on weight? because we’re all supposed to weigh our toddlers every time we give them tylenol? i have a 2-year-old. i don’t know what she weighs. i just know she’s small. and that’s enough. i’m not a vet. i’m a parent. stop pretending we’re scientists.
and why do they put the ‘do not operate heavy machinery’ warning on cough syrup? who’s taking cough syrup and then going to drive a forklift? is there a secret population of drugged warehouse workers? i need to know.
and why do they say ‘consult your doctor’ like that’s a solution? my doctor doesn’t answer texts. i have to wait 3 weeks for an appointment. meanwhile, my kid’s fever is at 103. so i’m Googling ‘can i give my kid half a pill?’ and that’s how people die.
we need a national app. like a barcode scanner that tells you, in plain English, ‘this will kill you if you take it with alcohol.’ not ‘may interact.’ just say ‘DANGER.’ like a warning on a pack of cigarettes. but for pills. because pills are the new cigarettes.
John Pope
January 18, 2026 at 19:59
the real tragedy isn’t that people don’t read labels-it’s that we’ve outsourced our own agency to corporations and pharmacists. we’ve turned medicine into a ritual of obedience. ‘take one pill’-but who decided one? who authorized it? what if the label is wrong? what if the doctor made a typo? what if the pharmacy filled it wrong? we don’t question. we just swallow. and that’s the real poison.
we’re not patients. we’re consumers. and the label? it’s the fine print on a contract we never read. and now we’re surprised when the system eats us alive.
you want to fix this? stop telling people to ‘read the label.’ start telling corporations to make labels that don’t require a PhD to decode.
Clay .Haeber
January 19, 2026 at 15:13
oh wow. another ‘read the label’ PSA. how original. next you’ll tell us to breathe in and out. maybe we should all just stop taking medicine and start meditating. or better yet-let’s just let the pharmaceutical CEOs take our pills. they’re the ones who designed them anyway. maybe they’ll finally feel the pain they’ve monetized.
also, ‘scan the QR code’? cute. i’m sure the 78-year-old with arthritis and no smartphone is just thrilled. ‘Oh thank you, FDA, for making my medicine require a TikTok tutorial.’
and ‘color-coded labels’? brilliant. now we can have red pills for opioids. because nothing says ‘this will kill you’ like a bright red cap. like a candy. because we all know toddlers don’t go for red things.
you want to save lives? stop making medicine look like a carnival game.
Priyanka Kumari
January 21, 2026 at 04:53
I’ve worked in community health in India for 12 years. In villages, people often take leftover antibiotics because they can’t afford a new prescription. They don’t read labels because they can’t read at all. But when we teach them with pictures-this pill for fever, this one for infection, this one red = stop if you feel dizzy-they remember. It’s not about literacy. It’s about clarity. This post? It’s the same principle. Just make it visual. Make it simple. And for God’s sake, stop using Latin.
Avneet Singh
January 22, 2026 at 17:35
the entire premise is flawed. labels are not the problem. the problem is the commodification of healthcare. when medicine is treated like a consumer product, you get labels designed for liability, not safety. also, ‘active ingredient’? that’s a euphemism. it’s the profit center. the rest is filler. and you wonder why people don’t trust it?
also, QR codes? how quaint. we’re still in the analog era of pharmaceutical regulation. the real innovation would be AI-driven personalized dosage alerts based on your genetic profile, medical history, and current medications. but no-let’s just give people more paper.
Adam Vella
January 24, 2026 at 11:08
the notion that medication labels are the primary vector for preventable errors is statistically misleading. according to the Institute of Medicine, 80% of medication errors occur at the prescribing or dispensing stage, not at the patient reading stage. this article, while well-intentioned, misattributes causality and thereby misdirects public policy. the burden of comprehension should not rest on the layperson when the system fails upstream.
furthermore, the reliance on ‘pharmacist consultation’ as a panacea ignores the systemic underfunding of pharmacy services in the U.S., where pharmacists are often overworked, underpaid, and unable to provide individualized counseling. this is not a literacy issue-it is a structural failure.
to suggest that reading a label reduces error by 80% is not only empirically unsupported but dangerously simplistic.
Nelly Oruko
January 26, 2026 at 10:08
my grandma used to say: ‘If it doesn’t say it plain, don’t take it.’ She never went to college. But she knew how to read a label. And she lived to 94. Maybe the answer isn’t more tech. Maybe it’s just… slower. quieter. more careful.
vishnu priyanka
January 26, 2026 at 14:51
in my village back home, we use a system: if the bottle has a picture of a spoon, we use the spoon. if it has a line, we fill to the line. if it has no picture? we ask the neighbor who went to city once. no QR codes. no apps. just people. maybe that’s the real tech.
Angel Tiestos lopez
January 28, 2026 at 13:51
bro i just scanned the qr code on my azithromycin and it played a 2-minute video of a guy in scrubs saying ‘take this with food, not with pizza.’ 🤣 i’m not mad. i’m impressed. also, the video had a dog in it. 🐶
Alan Lin
January 30, 2026 at 09:32
if you’re taking medication without understanding the dosage, you’re not just risking your health-you’re risking your dignity. This isn’t about convenience. It’s about responsibility. Every pill you take is a choice. Make it an informed one. Don’t wait for an ER visit to learn the lesson. Start today. Read the label. Ask the pharmacist. Write it down. Do it for yourself. Do it for the people who love you. You owe them that much.
Trevor Whipple
January 31, 2026 at 00:31
^this. i just called my pharmacist. she sent me a giant-print label with emojis. 🩹💊⏱️. i cried. i didn’t know that was a thing. thanks, stranger.