How to Verify Dose Changes and Avoid Miscommunication in Healthcare
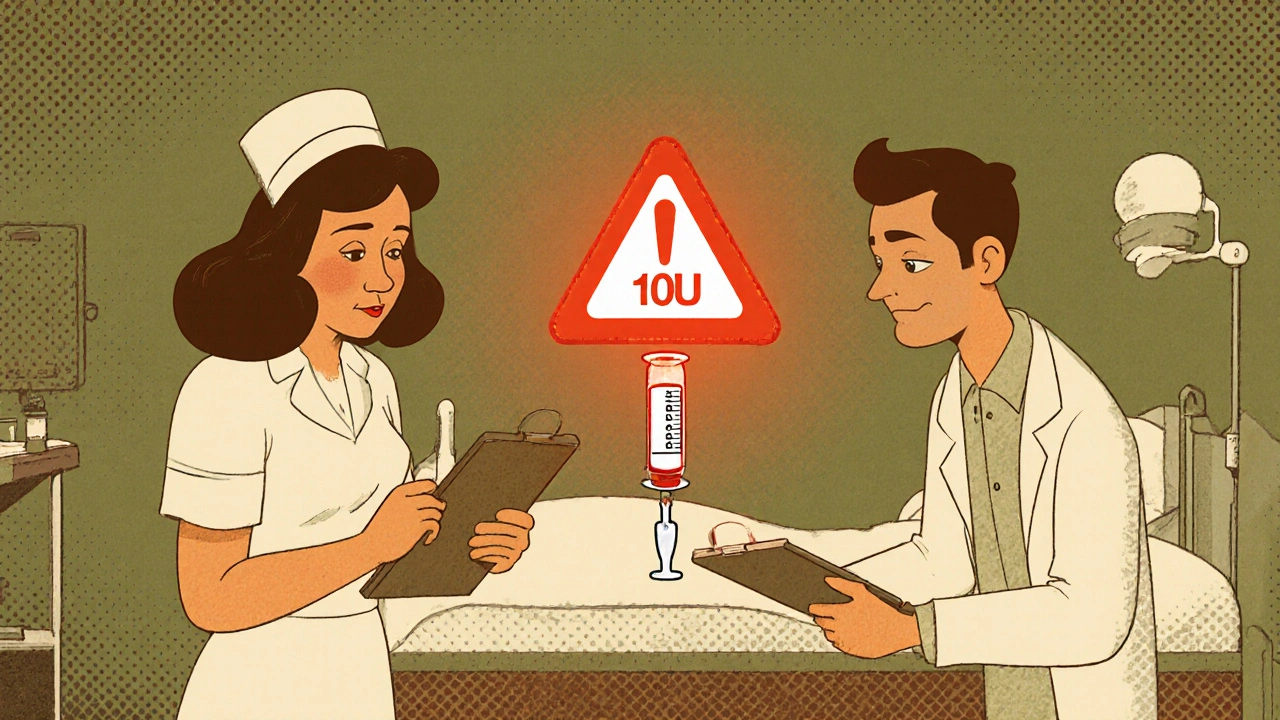
Getting a medication dose wrong isn’t just a mistake-it can kill. A patient meant to get 1 unit of insulin gets 10. A nurse misses a weight-based adjustment for a child. A doctor writes "10U" instead of "1.0U" and the system doesn’t catch it. These aren’t hypotheticals. In 2022 alone, over 1,200 reported incidents of incorrect dose changes led to nearly 300 cases of patient harm, according to the ECRI Institute. The problem isn’t always technology. It’s dose verification-or the lack of it-during handoffs, shift changes, and busy moments when communication breaks down.
Why Dose Changes Are the Most Dangerous Moment in Medication Safety
Most medication errors happen not when a drug is first prescribed, but when it’s changed. A patient’s kidney function drops. Their weight shifts. Their condition worsens. A new dose is ordered. That’s when the risk spikes. High-alert medications like insulin, heparin, morphine, and warfarin are especially dangerous because the margin between help and harm is razor-thin. A 10% error in insulin dosing can trigger a seizure. A wrong heparin dose can cause internal bleeding. The Joint Commission found that miscommunication during dose changes is the root cause of 65% of all medication-related sentinel events. And it’s not just doctors and nurses. Pharmacists, techs, and even patients themselves can be caught in the gap.The Three-Step Verification Protocol That Actually Works
The Institute for Safe Medication Practices (ISMP) doesn’t recommend blind double-checks for everything. That’s not just inefficient-it breeds complacency. Instead, they push for a targeted, three-step verification process that fits into real workflow:- Independent calculation - Two qualified staff members calculate the dose separately, without talking. For pediatric patients, that means verifying weight in kilograms and dose in mg/kg to the nearest 0.1mg/kg. For warfarin, it means confirming the INR target range was checked within the last 24 hours.
- Context check - Before giving the drug, verify the patient’s current condition. Is their creatinine clearance down? Did they just start a new antibiotic that interacts with their blood thinner? Did they miss meals? These aren’t just nice-to-knows-they’re critical. One nurse in Austin reported catching a 50% overdose because the patient’s recent lab showed acute kidney injury, and the original order didn’t reflect it.
- Barcode and bedside confirmation - Scan the patient’s wristband. Scan the medication. The system should flag mismatches in drug, dose, or route. But here’s the catch: barcode systems fail to catch 30% of wrong-dose errors if the concentration is entered correctly. That’s why human verification still matters.
This process takes about 5-7 minutes total. It’s not fast. But it’s the difference between a safe discharge and an ICU transfer.
Barcode Scanning vs. Human Double Checks: What Works Best
There’s a myth that technology alone can fix medication errors. It can’t. Barcode medication administration (BCMA) systems prevent 86% of wrong-drug and wrong-patient errors, according to a 2009 study in the Journal of the American Medical Informatics Association. But they’re blind to wrong-dose errors if the data input is wrong. One pharmacist in Texas saw a 10-fold overdose slip through because the system accepted the dose as “10 mg” - even though the correct dose was “1.0 mg.” The concentration was right, the drug was right, the patient was right. But the number? Off by a factor of ten.That’s where independent double checks shine. In sepsis simulations, double checks caught 100% of wrong-vial errors, while single checks missed 46%. They’re also the only method that reliably catches infusion pump programming mistakes-like setting a 10 mL/hour rate when it should be 1 mL/hour. The problem? Double checks are slow. Nurses spend 15-20% more time on med passes when doing them universally. And during peak hours, compliance drops to 45%.
The answer isn’t choosing one over the other. It’s combining them-smartly. ASHP guidelines say high-alert medications should require both barcode scanning AND independent double checks. But only for the highest-risk cases: insulin, opioids, heparin, IV potassium, and chemotherapy drugs. Don’t double-check every aspirin. Focus where it matters.

The Hidden Killer: Poor Communication During Handoffs
One of the most dangerous moments in a hospital is shift change. Between 6:00 and 8:00 AM and PM, 61% of verification failures occur, according to ECRI. Why? Because handoffs are rushed. Someone says, “The patient got more insulin.” That’s not enough. The nurse taking over doesn’t know why, how much, or what the plan is.That’s where SBAR (Situation, Background, Assessment, Recommendation) comes in. A 2020 study in the Journal of Patient Safety showed that using SBAR during dose change handoffs reduced communication errors by 41%. Instead of saying, “He got more insulin,” you say:
- Situation: “Mr. Smith’s morning glucose was 280, up from 160 yesterday.”
- Background: “He’s on sliding scale insulin. His last dose was 6 units at breakfast.”
- Assessment: “His renal function is stable, but he’s had reduced oral intake.”
- Recommendation: “I’m increasing his basal insulin to 10 units at bedtime and holding the sliding scale until tomorrow’s labs.”
That’s clear. That’s safe. That’s verifiable.
Why Nurses Skip Verification (And How to Fix It)
A 2022 American Nurses Association survey found that 73% of nurses admitted skipping verification steps because they were rushed. One nurse wrote: “I had 12 patients. Two were crashing. I didn’t have time to double-check the insulin.” That’s not negligence-it’s system failure.Studies show that when hospitals add just 15-20 minutes of protected “safety time” per nurse per shift, dose verification errors drop by 37%. Johns Hopkins did this in 2022. They didn’t add more staff. They just blocked time on the schedule. No charting. No calls. No interruptions. Just verification.
Another fix: stop the alert fatigue. Nurses get 15-20 alerts per shift from barcode systems. Most are false alarms-like a mismatched vial that’s actually correct. When systems are tuned to only trigger alerts for high-risk errors, compliance jumps. Epic’s 2023 DoseRange Advisor reduced inappropriate doses by 52% by learning from historical data and only flagging doses that deviate from normal ranges for that patient.

What’s Next: AI, Voice, and Blockchain
The future isn’t just more checks-it’s smarter checks. AI tools now predict which dose changes are most likely to be wrong based on patient history, lab trends, and prescribing patterns. Voice recognition systems let nurses verify doses by speaking into a headset instead of typing, cutting documentation time by 65%. And blockchain pilots at Mayo Clinic are creating tamper-proof logs of every dose change, so if something goes wrong, you know exactly who did what, when.But none of this replaces human judgment. AI can’t see that a patient looks pale. Voice tech won’t catch a typo in a handwritten order. Blockchain doesn’t know if a dose was calculated right. Technology supports. Humans verify.
What You Can Do Right Now
You don’t need a new system to make a difference. Start here:- Use SBAR for every dose change handoff. Even if it’s just one sentence: “I changed his insulin from 6 to 10 units because his AM glucose was over 250.”
- Only double-check high-alert meds. Insulin. Heparin. Opioids. IV potassium. That’s it. Don’t waste time on antibiotics or antihypertensives.
- Always verify weight for kids. Never assume. Always recalculate.
- Ask: “What’s the goal?” Before giving a new dose, ask: “Why are we changing this? What are we trying to fix?”
- Speak up. If you’re unsure, stop. Say, “I need a second pair of eyes.”
Medication safety isn’t about perfection. It’s about layers. One layer fails. Another catches it. And another. That’s how lives are saved-not by one hero nurse, but by a system that expects mistakes and plans for them.
What is the most common cause of dose verification failure?
The most common cause is poor communication during handoffs-especially shift changes between 6:00-8:00 AM and PM. Studies show 61% of verification failures happen during these times because information is rushed, incomplete, or lost. Using structured tools like SBAR reduces these errors by 41%.
Do barcode systems catch all dosing errors?
No. Barcode systems catch 86% of wrong-drug and wrong-patient errors but miss up to 30% of wrong-dose errors, especially when the concentration is entered correctly but the dose is wrong (e.g., 10 mg instead of 1.0 mg). Human verification is still required for dose accuracy.
Which medications need double checks?
The ISMP and ASHP recommend independent double checks only for high-alert medications: insulin, heparin, opioids, IV potassium, and chemotherapy drugs. Double-checking every medication leads to alert fatigue and reduces effectiveness.
Why do nurses skip verification steps?
Nurses skip verification due to time pressure, high patient loads, and alert fatigue from too many system warnings. A 2022 survey found 73% of nurses admitted skipping steps during busy shifts. Adding 15-20 minutes of protected safety time per shift can increase compliance by 37%.
Is there a legal requirement to verify dose changes?
Yes. The Joint Commission requires reliable processes for verifying high-risk medication dose changes under NPSG.01.01.01, effective January 1, 2024. Hospitals with more than 0.5% dose verification error rates face penalties from CMS. Failure to follow protocols can lead to liability in malpractice cases.






14 Comments
Levi Hobbs
November 17, 2025 at 23:44
I've seen this play out so many times-nurses rushing between rooms, alarms blaring, and someone just says, 'He got more insulin.' No context. No numbers. No follow-up. It's terrifying. The SBAR method isn't just bureaucracy-it's a lifeline. I started using it on my unit last month, and we've had zero dose-related near-misses since. It takes 30 seconds longer, but it saves lives. Simple as that.
henry mariono
November 19, 2025 at 02:29
Double-checks are great in theory, but when you're managing 18 patients and your EHR freezes every time you scan a barcode, it's not practical. We need better tech-not more steps. I get the intent, but the system is working against us, not for us.
Sridhar Suvarna
November 19, 2025 at 06:52
From India, I can say this: We face the same issues, but with even fewer resources. In rural hospitals, we don't have barcode scanners. We don't have AI. We have nurses who memorize weights, calculate doses on scrap paper, and rely on trust. This article? It's not just for the US. It's for every ICU in every developing country. The principles are universal. Human verification is non-negotiable. Technology is a tool-not a replacement.
Joseph Peel
November 20, 2025 at 15:18
There is a critical distinction between verification and validation. Verification confirms the math; validation confirms the clinical rationale. Most protocols focus only on the former. The context check described here is the only part that truly addresses the latter. This is the most underappreciated component in the entire medication safety framework.
Kelsey Robertson
November 22, 2025 at 08:12
Let’s be real: This whole ‘verification’ thing is just corporate theater. Hospitals care more about avoiding lawsuits than saving lives. They’ll make you check insulin doses but let you give a 500mg dose of amoxicillin to a patient allergic to penicillin because ‘it’s not high-alert.’ And don’t get me started on AI-those algorithms are trained on biased data. They’ll normalize dangerous practices and call it ‘efficiency.’ Wake up.
Joseph Townsend
November 22, 2025 at 19:08
Y’all are acting like this is the first time anyone’s ever thought about dose safety. I’ve been in this game since 2008. We had nurses writing ‘U’ for units back then-and people died. And now? Now we have fancy scanners, AI, blockchain, voice tech… and the same damn mistakes. Why? Because nobody wants to slow down. Nobody wants to admit they’re tired. We’re not fixing the problem-we’re just adding glitter to the corpse.
Bill Machi
November 24, 2025 at 17:26
Why are we letting nurses do math at all? This is America. We have computers. We have engineers. We have billions in healthcare spending. And yet, we still rely on overworked, underpaid staff to do calculations that a 10-year-old with a calculator can do? This isn’t safety-it’s negligence dressed in scrubs. We need automation. Full stop. No more human math. No more ‘double-checks.’ Let the machine do it. If it fails, fire the vendor.
Elia DOnald Maluleke
November 25, 2025 at 06:43
In the grand tapestry of human frailty, we are all flawed vessels-nurses, doctors, pharmacists, even the systems we build. Yet, we cling to protocols like they are divine law. But no algorithm, no barcode, no SBAR form can replace the quiet moment when a nurse looks into a patient’s eyes and thinks, ‘This doesn’t feel right.’ That is the last, sacred checkpoint. No technology can replicate that intuition. It is not inefficiency-it is wisdom.
satya pradeep
November 26, 2025 at 16:02
Man, I work in a hospital in Kerala and we dont even have barcode scanners. We write doses on paper, call the pharmacy, and wait. But we do one thing right-we say the dose out loud before giving it. Like, ‘Ten units of insulin for Mr. Rajan.’ And the next person repeats it. Sounds dumb? It saved my ass last month when the script said 100 units. I caught it because I said it out loud. Sometimes the dumbest thing works.
Prem Hungry
November 28, 2025 at 14:43
To all the nurses reading this-you’re not lazy. You’re exhausted. And the system is broken. But you’re still showing up. That matters. I’ve been where you are. I’ve skipped checks too. But I learned: one extra minute now saves ten hours in ICU later. Block that 15 minutes. Protect it. Your patient deserves it. And so do you.
Leslie Douglas-Churchwell
November 30, 2025 at 03:44
AI is watching you. Blockchain logs every dose. But who’s behind the curtain? Big Pharma. They don’t want you to double-check insulin-they want you to use their expensive pumps, their proprietary algorithms, their branded vials. They profit from complexity. The ‘verification’ protocol? It’s a distraction. The real solution? Public healthcare. Universal access. No profit motive. Then-and only then-will safety be the priority.
shubham seth
December 1, 2025 at 07:51
Let’s not pretend this is about safety. This is about liability. Hospitals don’t care if you live or die-they care if you sue them. That’s why they push SBAR and double-checks: not because it’s better for patients, but because it creates a paper trail that says, ‘We tried.’ The moment you stop documenting, the moment you stop checking, you’re not a nurse-you’re a scapegoat. This system rewards compliance, not competence.
Kathryn Ware
December 3, 2025 at 06:27
Just wanted to say thank you for writing this. I’m a new grad nurse and I was so overwhelmed my first month-I thought I was the only one missing things. I started using the SBAR script for every change, even if it was just one sentence. My preceptor thought I was being weird at first… but then she started doing it too. Last week, I caught a 10x insulin error because I asked, ‘Why are we changing this?’ And the answer was, ‘Oh, I didn’t know his creatinine was 4.2.’ We didn’t give it. He stayed out of the ICU. I’m not a hero. I just asked a question. That’s all it takes.
kora ortiz
December 3, 2025 at 17:39
This is exactly what we need-clear, practical, no fluff. The system isn’t broken. It’s just been neglected. You don’t need a revolution. You need consistency. One nurse. One shift. One SBAR. One double-check. It adds up. I’ve seen it. And I’ve seen the alternative. Choose the hard thing. Every time.