Best Antipsychotic: How to Pick the Right One for You
When talking about best antipsychotic, the medicine that offers the highest balance of symptom control, tolerability, and practicality for serious mental health conditions. Also known as optimal antipsychotic therapy, it matters for anyone facing schizophrenia, a chronic brain disorder marked by hallucinations, delusions, and cognitive decline. Choosing the right drug isn’t just a medical decision; it’s a daily‑life choice that influences work, relationships, and overall wellbeing.
The antipsychotic landscape splits into two major families: atypical antipsychotics, second‑generation drugs that target dopamine and serotonin receptors and usually cause fewer movement problems and the older typical antipsychotics, first‑generation agents focused mainly on dopamine blockade, often linked with higher risk of tremor, stiffness, and tardive dyskinesia. A key semantic triple here is: Best antipsychotic encompasses efficacy, side‑effect profile, and cost. Another is: Atypical antipsychotics influence mood stabilization. And: Antipsychotic treatment requires dopamine receptor blockade to reduce psychosis. Understanding these relationships helps you weigh what matters most—whether it’s sharper thinking, fewer motor side‑effects, or a lower price tag.
Key Factors When Picking a Medication
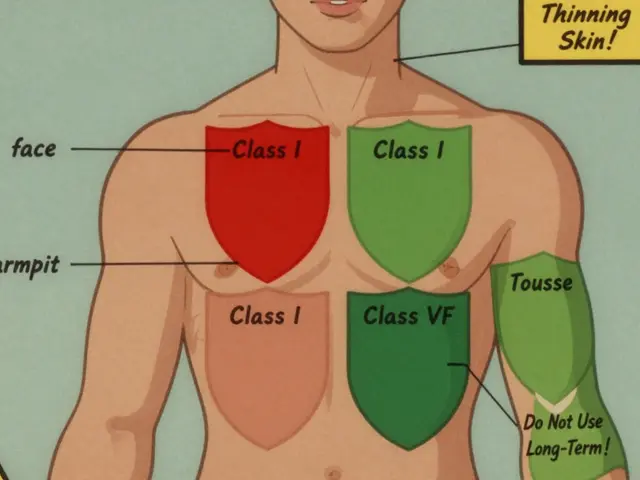
First, look at efficacy, how well the drug reduces core psychotic symptoms like hallucinations and delusions. Clinical trials rank clozapine, risperidone, and aripiprazole among the most potent for treatment‑resistant schizophrenia, but each carries its own monitoring needs. Second, weigh side effects, the unwanted reactions that can affect metabolism, heart rhythm, or movement. Atypicals such as olanzapine can cause weight gain and diabetes, while typicals like haloperidol may trigger extra‑pyramidal symptoms.
Third, consider cost and accessibility, the out‑of‑pocket expense and insurance coverage that dictate long‑term adherence. Generic versions of risperidone or quetiapine often cost a fraction of brand‑name options, making them practical for patients on a tight budget. Fourth, match the drug to the specific diagnosis. For bipolar disorder, medications that also stabilize mood—like quetiapine or lurasidone—are preferred over pure psychosis‑only agents. Finally, think about personal health history: liver function, cardiac health, and previous drug reactions shape the safety profile.
Real‑world experience shows that the “best” label shifts over time. A patient may start on an atypical for its smoother side‑effect curve, then switch to clozapine if symptoms linger despite multiple trials. Monitoring blood counts, lipid panels, and glucose levels becomes part of the therapeutic journey. This dynamic process underscores the triple: Best antipsychotic requires ongoing assessment and possible adjustment. It also explains why clinicians often pair medication with psychotherapy, lifestyle changes, and community support.
Below you’ll find a curated list of articles that dive deeper into specific drug comparisons, safety tips for buying generics, and practical guides for managing side effects. Whether you’re a patient, caregiver, or health professional, the collection offers actionable insights to help you navigate the complex world of antipsychotic therapy and move toward the most suitable option for your situation.

Seroquel vs Alternatives: Which Antipsychotic Fits You Best
Compare Seroquel (Quetiapine) with top antipsychotic alternatives, covering efficacy, side effects, dosage, and best-use scenarios in a clear, patient‑focused guide.
Read More