Insulin Reduction: Strategies, Tips, and Medication Insights
When talking about insulin reduction, the process of lowering excess insulin in the bloodstream to improve metabolic health. Also known as insulin lowering, it matters for weight management, heart health, and preventing long‑term complications.
One of the biggest groups affected is people with type 2 diabetes, a chronic condition where the body’s cells become resistant to insulin. Managing this condition often starts with insulin reduction because high insulin can drive hunger, fat storage, and inflammation. Lifestyle changes, medication tweaks, and monitoring work together to keep blood sugar steady.
How Blood Sugar Monitoring Shapes Insulin Reduction
Accurate blood sugar control, tracking glucose levels before and after meals, during exercise, and at night is the backbone of any insulin‑lowering plan. When you see spikes, you can adjust carbs, activity, or meds right away. This feedback loop directly influences how much insulin the pancreas needs to produce, creating a clear cause‑and‑effect link.
Dietary choices are the next big lever. dietary interventions, low‑glycemic foods, fiber‑rich meals, and balanced macronutrients have been shown to blunt insulin spikes. Swapping refined carbs for whole grains, adding healthy fats, and timing protein around workouts are practical steps most readers can try today.
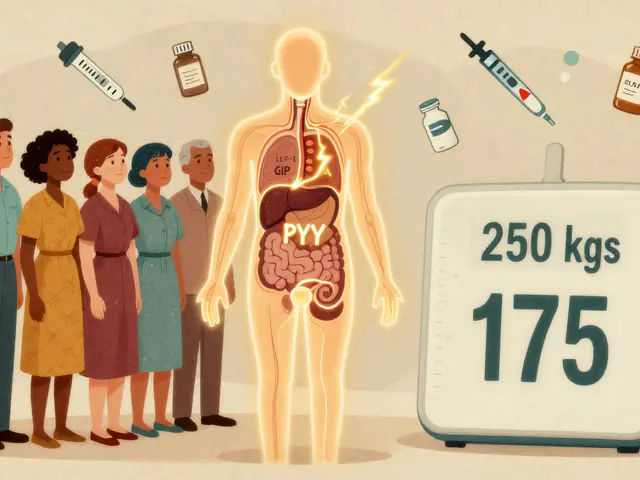
Exercise isn’t just about burning calories; it’s a powerful insulin sensitizer. Regular aerobic activity, strength training, and even short walks after meals increase the muscles’ ability to take up glucose without extra insulin. This relationship forms a semantic triple: exercise influences insulin reduction, which improves blood sugar control.
Medication options also play a role. Some drugs, like metformin, directly lower hepatic glucose output, indirectly reducing insulin demand. Others, like SGLT2 inhibitors, help the kidneys excrete glucose, easing the insulin load. Knowing which medication fits your health profile can speed up the reduction process.
Natural supplements can complement the plan, but safety matters. Ingredients like berberine, cinnamon extract, and alpha‑lipoic acid have modest evidence for improving insulin sensitivity. Always check for interactions with prescribed meds before adding any supplement to your routine.
Stress management rounds out the picture. Chronic cortisol spikes push the body to release more insulin. Simple practices—mindful breathing, short meditation, or a hobby you enjoy—can lower stress hormones, making insulin reduction easier.
Putting all these pieces together means you’ll have a toolbox that includes blood sugar monitoring, smart food choices, regular movement, appropriate meds, safe supplements, and stress relief techniques. Below you’ll find a curated list of articles that dive deeper into each of these topics, from medication comparisons to natural remedy guides, helping you build a personalized insulin‑lowering strategy.

Vidagliptin and Insulin Reduction in Type 2 Diabetes: What the Evidence Says
Explore how vidagliptin, a DPP‑4 inhibitor, can lower insulin needs in type 2 diabetes, backed by trial data, safety info, and practical tips.
Read More