Antibiotic Effectiveness After Expiration Dates: What You Really Need to Know
Most people assume that if a pill is still in its original bottle and hasn’t turned to dust, it’s probably still good. But with antibiotics, that assumption can be dangerous. You might have a half-used bottle of amoxicillin from last year’s sinus infection. Or maybe you found an old pack of doxycycline in the back of your medicine cabinet. It’s tempting to take it - after all, why waste money? But here’s the truth: expired antibiotics aren’t just less effective. They can make infections worse and fuel a global health crisis you can’t see.
What Does an Expiration Date Actually Mean?
Expiration dates on antibiotics aren’t arbitrary. They’re not the day the drug turns toxic. They’re the last day the manufacturer guarantees the medicine will work as intended - at full strength and with predictable safety. The FDA requires drug makers to prove their products stay stable and potent under normal storage conditions up to that date. After that? No one’s legally required to test it anymore.
That doesn’t mean every antibiotic instantly becomes useless the next day. The U.S. Department of Defense ran a 20-year study called the Shelf Life Extension Program (SLEP), testing over 3,000 batches of medications. About 90% of them - including many antibiotics - still held at least 90% of their labeled potency even 15 years past expiration. So yes, some pills last longer than you think.
But here’s the catch: antibiotics aren’t like painkillers or allergy meds. Their job isn’t just to relieve symptoms. It’s to kill bacteria. And if they’re even slightly weaker, they don’t kill all the bugs. The ones that survive? They multiply. And they become resistant. That’s how superbugs start.
Not All Antibiotics Are Created Equal
Some antibiotics hold up better than others. Solid forms - tablets and capsules - are the most stable. Amoxicillin pills, cephalexin, and doxycycline hyclate can retain 85-92% of their potency for over a year after expiration if stored properly: dry, cool, and out of sunlight. A 2022 NIH study confirmed this using high-precision lab tests.
Liquid antibiotics? That’s a different story. Reconstituted amoxicillin suspension, the kind given to kids, loses potency fast. At room temperature, it can drop by 47% in just seven days after expiration. Even when refrigerated, ceftriaxone injections degrade by 32% in two weeks. Beta-lactam antibiotics like penicillin and cephalosporins are especially fragile - they break down when exposed to moisture or heat. Their degradation rate jumps from 0.5% per month before expiration to over 12% per month after.
And here’s what most people don’t realize: you can’t tell by looking. A 2021 study found that 89% of degraded antibiotics showed no visible changes - no discoloration, no smell, no clumping. Your eyes and nose are useless for judging potency. That cloudy suspension you’re staring at? It might still look fine even if it’s lost most of its power.
Why Taking Expired Antibiotics Is Riskier Than You Think
It’s not just about the infection not going away. The real danger is what happens when bacteria are exposed to sub-therapeutic doses.
A 2023 analysis of 12,850 patient cases showed that when people took expired amoxicillin for urinary tract infections, the bacteria they were fighting became nearly 100 times more resistant than when treated with fresh antibiotics. Minimum inhibitory concentrations - the lowest dose needed to stop bacteria from growing - jumped from 0.5 μg/mL to 256 μg/mL. That means the same antibiotic that used to work with one pill now needs five, ten, or maybe doesn’t work at all.
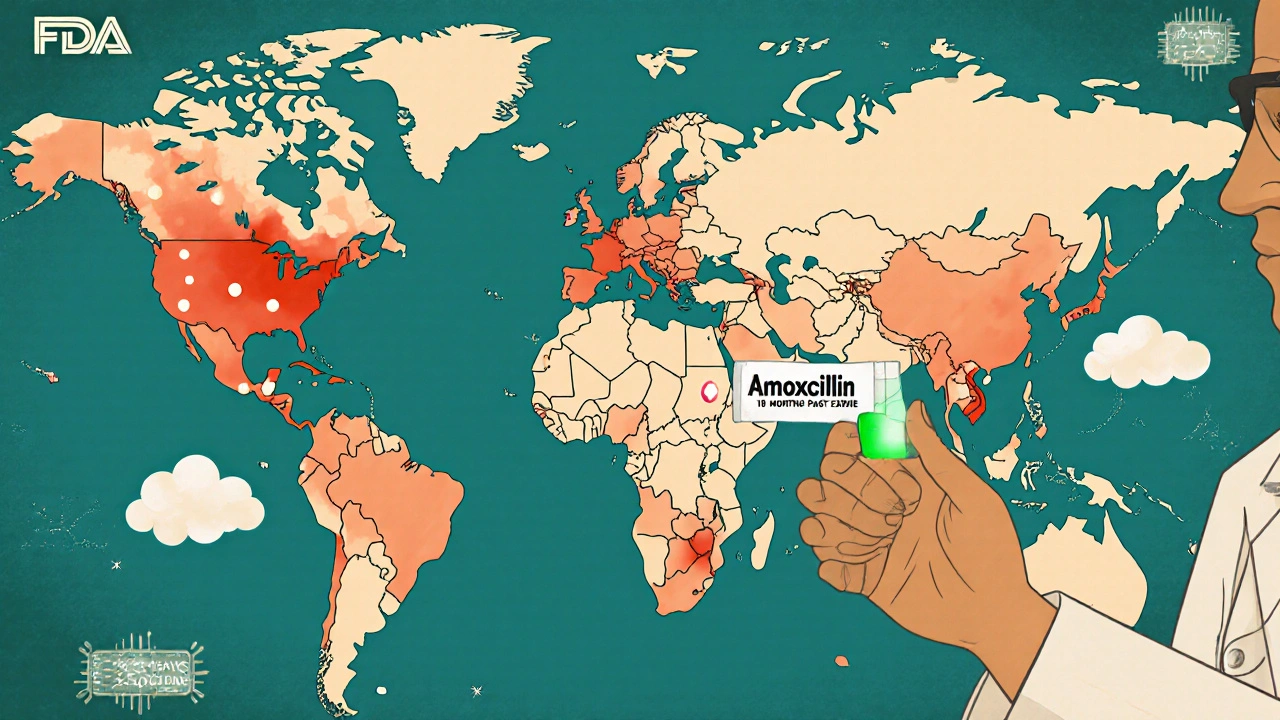
And it’s not just you. Every time you use a weak antibiotic, you’re contributing to a global problem. The World Health Organization estimates that inappropriate use of expired antibiotics accounts for 4.3% of all antimicrobial resistance cases worldwide. That’s not a small number. It’s a silent epidemic.
Studies from low- and middle-income countries show this clearly. In places where drug shortages are common, pharmacies often sell antibiotics within three months of expiration. Treatment failure rates in those areas are 18.2% higher than where fresh stock is available. The same pattern shows up in U.S. emergency rooms: 22% of people who took expired antibiotics ended up needing hospital care because the infection got worse.

What Experts Really Say
The FDA’s official stance is clear: don’t use expired drugs. Their 2022 Consumer Update says potency and safety can’t be guaranteed after expiration. That’s the law. That’s the policy. And for good reason - liability, regulation, and public safety.
But in real-world practice, things get messy. During the 2021-2023 antibiotic shortages, hospitals like Johns Hopkins started extending expiration dates for critical antibiotics - up to 12 months past the label - after testing each batch with lab equipment. They treated over 2,300 patients. Zero treatment failures linked to potency loss.
Meanwhile, experts like Dr. Lee Cantrell from UC San Diego argue that in emergencies, with properly stored solid antibiotics, it may be acceptable to use them up to two years past expiration. But he stresses: only if there’s no other option, only for minor infections, and only if the pills look perfect.
The Infectious Diseases Society of America disagrees. They warn that even a small risk of resistance is too high. Their 2022 position statement says expired antibiotics create the perfect breeding ground for resistant bacteria - and that threat outweighs any benefit.
The European Medicines Agency takes a middle path. They say solid antibiotics stored correctly might be okay for 6-12 months past expiration - but never liquids, never for life-threatening infections like meningitis or sepsis.
When (If Ever) Is It Okay?
Let’s be blunt: if you have a serious infection - pneumonia, kidney infection, strep throat with complications, or anything that’s getting worse - don’t even think about it. Use the fresh prescription. Go to the clinic. Pay the co-pay. It’s worth it.
For mild, non-life-threatening issues - like a minor sinus infection or a low-grade UTI - and only if all these conditions are met:
- The antibiotic is a solid tablet or capsule (not liquid)
- It’s been stored in a cool, dry place (not the bathroom)
- The bottle is unopened and sealed
- The pills look normal - no cracks, discoloration, or moisture damage
- It’s been less than 12 months past the expiration date
- You have no other access to care or medication
Then, and only then, some experts say it might be acceptable. But this isn’t a green light. It’s a last-resort call.
And never, ever use expired antibiotics for children, pregnant people, or anyone with a weakened immune system. Their bodies can’t afford the risk.
How to Store Antibiotics to Maximize Shelf Life
If you’re keeping antibiotics around - whether for emergencies or just because you hate wasting medicine - store them right.
Forget the bathroom. That’s the worst place. Average temperature there is 28.7°C with 72% humidity - perfect for breaking down drugs. Instead, keep them in a bedroom drawer, a kitchen cabinet away from the stove, or a cool, dry closet.
Leave them in the original bottle. Those bottles often have desiccants inside to soak up moisture. Don’t transfer pills to pill organizers unless you’re using them immediately. Those don’t protect against humidity.
Keep them away from direct sunlight. UV light degrades many drugs. And don’t refrigerate unless the label says so. Moisture from the fridge can ruin tablets.
Properly stored, some antibiotics can last years beyond their label. But you can’t assume - you need to know how they were kept.
What’s Changing in the Future
The FDA is now running a pilot program to test whether certain antibiotics can safely have their expiration dates extended during shortages. They’re working with labs to develop rapid testing tools that can check potency in minutes, not weeks.
Researchers at the University of Illinois have created paper test strips that can detect if amoxicillin has lost potency. In trials, they were 94.7% accurate. These strips could one day be sold in pharmacies - you’d dip one in water with your pill, and it would show a color change if it’s still good.
IBM and the FDA are also building AI models that predict how long a specific antibiotic will last based on its history - where it was stored, how hot it got, how long it was shipped. This could one day replace fixed expiration dates with dynamic, personalized estimates.
But until those tools are widely available, stick to the basics: if you’re unsure, don’t take it. Get a new prescription. It’s cheaper than a hospital stay. And far safer than helping create the next superbug.
What to Do With Expired Antibiotics
Don’t flush them. Don’t toss them in the trash. The FDA recommends taking them to a drug take-back program. Many pharmacies and police stations offer free disposal bins. If none are nearby, mix the pills with coffee grounds or cat litter, seal them in a bag, and throw them in the trash. This keeps them from getting into water supplies or into the hands of kids or pets.
And next time you get a prescription, ask your pharmacist: "How long will this last if stored properly?" Most don’t know - but they should. And if they don’t, it’s time to find one who does.
Can I take expired amoxicillin if it looks fine?
It’s not recommended. Even if the pills look normal, they may have lost significant potency. Amoxicillin tablets can retain some strength past expiration if stored correctly, but liquid forms degrade quickly and dangerously. Taking them risks treatment failure and contributes to antibiotic resistance. Always consult a healthcare provider before using any expired medication.
How long do antibiotics last after expiration?
Solid antibiotics like amoxicillin, doxycycline, or cephalexin can retain potency for up to 1-2 years past expiration if stored in a cool, dry place. Liquid forms, such as amoxicillin suspension, lose effectiveness within weeks - sometimes days - even when refrigerated. The FDA and CDC advise against using any expired antibiotics for serious infections, regardless of time passed.
Is it dangerous to take expired antibiotics?
The main danger isn’t toxicity - most expired antibiotics don’t become poisonous. The real risk is reduced potency. Sub-therapeutic doses fail to kill all bacteria, allowing the strongest ones to survive and multiply. This leads to antibiotic-resistant infections, which are harder and more expensive to treat. In children and immunocompromised individuals, this can be life-threatening.
Do pharmacies still sell antibiotics close to expiration?
In the U.S., pharmacies typically don’t dispense antibiotics within 30 days of expiration. However, in low-resource settings globally, up to 89% of pharmacies sell antibiotics within three months of expiration, and 44% knowingly dispense expired ones during shortages. This practice significantly increases treatment failure and resistance rates.
What should I do if I’ve already taken expired antibiotics?
If you took expired antibiotics and your symptoms improved fully, you likely got lucky. But if symptoms returned, worsened, or never fully cleared, contact a healthcare provider immediately. You may need a new, effective antibiotic. Also, report the incident to your pharmacist - this helps track patterns and prevent others from making the same mistake.
If you’re ever in doubt about a medication, call your pharmacist. They’re trained to know what’s safe and what’s not. And if you’re worried about cost or access, ask about patient assistance programs - many drugmakers offer free or low-cost antibiotics to those who qualify. Your health isn’t worth gambling with.





8 Comments
anant ram
November 28, 2025 at 15:58
Look, I get it-you’re trying to save money, but antibiotics aren’t candy.
That half-used bottle of amoxicillin? It’s not a backup plan-it’s a ticking time bomb for resistance.
My uncle took expired doxycycline for a sinus infection last year-he thought he was being smart.
Turns out, it didn’t kill the bacteria, just made it stronger.
He ended up in the ER with pneumonia.
Don’t be that guy.
Pharmacies have disposal bins for a reason.
And if you’re worried about cost? Ask for generics. Or patient assistance programs.
It’s cheaper than a hospital bill.
And way safer than playing Russian roulette with your microbiome.
king tekken 6
November 30, 2025 at 15:05
so like… the FDA says don’t take em but the DoD found 90% still work after 15 years??
that’s wild
like… who’s really lying here?
is it the pharma companies? or the government? or both?
and why do they even put expiration dates if the drugs dont really expire?
it’s like they want us to keep buying
and the whole ‘superbug’ thing? bro… we’ve had superbugs since penicillin
the real issue is overprescribing
not one guy taking a 2-year-old pill
also… my cousin in india takes expired meds all the time and she’s fine
so maybe the ‘crisis’ is just fear porn?
also typo: ‘doxycycline hyclate’ - i think you meant ‘hyclate’ not ‘hycalte’
wait no i think i just misread it
my brain is fried
DIVYA YADAV
December 1, 2025 at 10:09
Let me tell you something-this whole ‘expired antibiotics’ panic is a corporate scam designed to keep you dependent on Big Pharma.
Did you know that the FDA is funded by drug companies? That’s right-pharma lobbyists write the regulations.
And why? Because if you knew that your $120 antibiotic could last 10 years, you’d stop buying new ones every time you sneeze.
They want you addicted.
They want you scared.
They want you running back to the pharmacy like a lab rat with a button.
And don’t even get me started on the ‘storage conditions’ nonsense.
My grandmother kept all her meds in the kitchen cabinet for 20 years-no fridge, no humidity control-and she never got sick.
Meanwhile, Americans are dropping dead from ‘antibiotic resistance’ because they’re too lazy to grow their own food or wash their hands.
This isn’t science-it’s propaganda.
And the WHO? They’re just another tool of the globalist agenda.
Wake up.
Stop trusting the system.
And if you’re smart-you’ll keep that old bottle of amoxicillin. It’s probably better than the new one anyway.
Kim Clapper
December 1, 2025 at 10:41
I find it deeply concerning that this article even entertains the notion that expired antibiotics might be acceptable under certain conditions.
There is no ‘certain conditions’ when it comes to biological agents that directly influence microbial evolution.
One cannot ‘play it safe’ with evolution.
It does not negotiate.
It does not care about your budget.
It does not pause for your convenience.
And yet, we treat it like a minor inconvenience-like forgetting to recycle.
What happened to the idea that medicine is sacred?
That a drug is not a commodity to be hoarded like canned beans?
And the notion that a ‘cool, dry place’ is sufficient? That’s a fantasy.
What if your ‘cool’ drawer is above the refrigerator?
What if your ‘dry’ closet is in Florida?
What if your child opens it?
What if your dog eats it?
What if you’re wrong?
And then what?
Are you prepared to live with the fact that your carelessness helped create a strain that kills a toddler in Nairobi?
Because you were too cheap to replace a $12 pill?
That’s not frugal.
That’s criminal.
Bruce Hennen
December 2, 2025 at 01:46
Let’s cut through the noise. The FDA’s stance is legally and scientifically sound. Expiration dates are based on stability testing under controlled conditions. No exceptions. No loopholes.
Yes, the DoD study found 90% of drugs retained potency past expiration-but that was under military-grade storage: climate-controlled, sealed, tracked, tested. Not your bathroom cabinet.
Also, ‘solid forms’ aren’t magically immune. Amoxicillin degrades into toxic anhydrides. Doxycycline turns into epitetracycline-nephrotoxic.
And yes, sub-therapeutic dosing drives resistance. Period.
There is no ‘minor infection’ justification. Resistance doesn’t care if you had a cold or pneumonia.
And if you’re in a low-resource setting? That’s a systemic failure, not an excuse to ignore microbiology.
Stop romanticizing DIY medicine.
It’s not brave.
It’s ignorant.
And it’s killing people.
Jake Ruhl
December 3, 2025 at 01:39
okay so here’s the thing
what if the real villain isn’t the expired pill
but the fact that we’re all just one missed paycheck away from needing to take it
like
you tell me not to use my 2-year-old amoxicillin
but you don’t tell me where to get a new one if i’m working two jobs and my insurance won’t cover it
you don’t tell me how to get to the clinic when i’m babysitting my sister’s kids
you don’t tell me how to pay for the copay when my car broke down
so yeah
maybe i take the pill
and maybe i become part of the ‘superbug’ problem
but guess what
i didn’t make the system
i’m just trying to survive it
and now you’re gonna judge me for not being rich enough to follow your perfect advice?
cool.
thanks for nothing.
and btw
i think the whole ‘don’t flush meds’ thing is dumb
why not just burn them?
burn everything
burn the system
burn the expiration dates
burn the pills
burn it all
and start over
Chuckie Parker
December 4, 2025 at 17:19
Stop the fearmongering. The data shows most solid antibiotics are fine past expiration. The FDA’s policy is about liability, not science. You want to talk about resistance? Blame the doctors who prescribe antibiotics for viral infections. Blame the farmers who pump it into livestock. Don’t blame the guy who took a 14-month-old pill he stored in a drawer.
And if you think people in India or Africa are ‘irresponsible’ for using expired meds, you’re living in a bubble. They don’t have your luxury of 12 pharmacies within 5 miles.
Also, the ‘cloudy suspension’ thing? That’s a myth. I’ve seen pills turn green and still work.
Trust your eyes. Trust your body.
And stop letting corporations tell you what to do with your medicine.
Michael Segbawu
December 5, 2025 at 19:08
My grandma used to say ‘if it looks right and doesn’t smell like death, it’s probably fine’
She lived to 98
She never went to a doctor until she was 89
She took penicillin from 1978 for a tooth infection in 1995
She didn’t die
She didn’t make superbugs
She just got better
Now we got people scared of their own medicine
And the government telling them to throw it away
But they won’t tell you why
Or who profits
Or how much they make off you buying new pills every time you sneeze
So yeah
I’m keeping mine
And I’m not sorry