Verifying Your Prescription at the Pharmacy: A Patient Checklist to Prevent Medication Errors
Why You Should Always Check Your Prescription Before Leaving the Pharmacy
Every year, over 1.5 million people in the U.S. are harmed by medication errors. Many of these mistakes happen at the pharmacy - not because the doctor wrote the wrong script, but because the wrong pill was handed out. You might think pharmacists catch all the errors. They do most of them. But prescription verification is your last line of defense. And it only takes three minutes.
Studies show that when patients actively check their medications before leaving, they catch up to 37% of errors that would’ve gone unnoticed. That’s not just helpful - it’s life-saving. A 2022 CMS audit found that 12.7% of pharmacy claims had errors that could’ve been stopped if the patient had asked a simple question. You don’t need to be a doctor. You just need to know what to look for.
The Seven Things You Must Check on Every Prescription
Don’t just take the bottle and go. Stop. Look. Confirm. Here’s what to check every single time:
- Your name and date of birth - Make sure they match your ID exactly. One wrong letter or number can mean you get someone else’s medicine. In 2023, 18.3% of pharmacy errors were due to wrong patient identification.
- The medication name - Is it the same as what your doctor told you? Watch out for look-alike names like Hydroxyzine and Hydralazine. If it looks unfamiliar, ask. Generic names (like metoprolol) are fine, but if you were prescribed Lopressor and got something else, speak up.
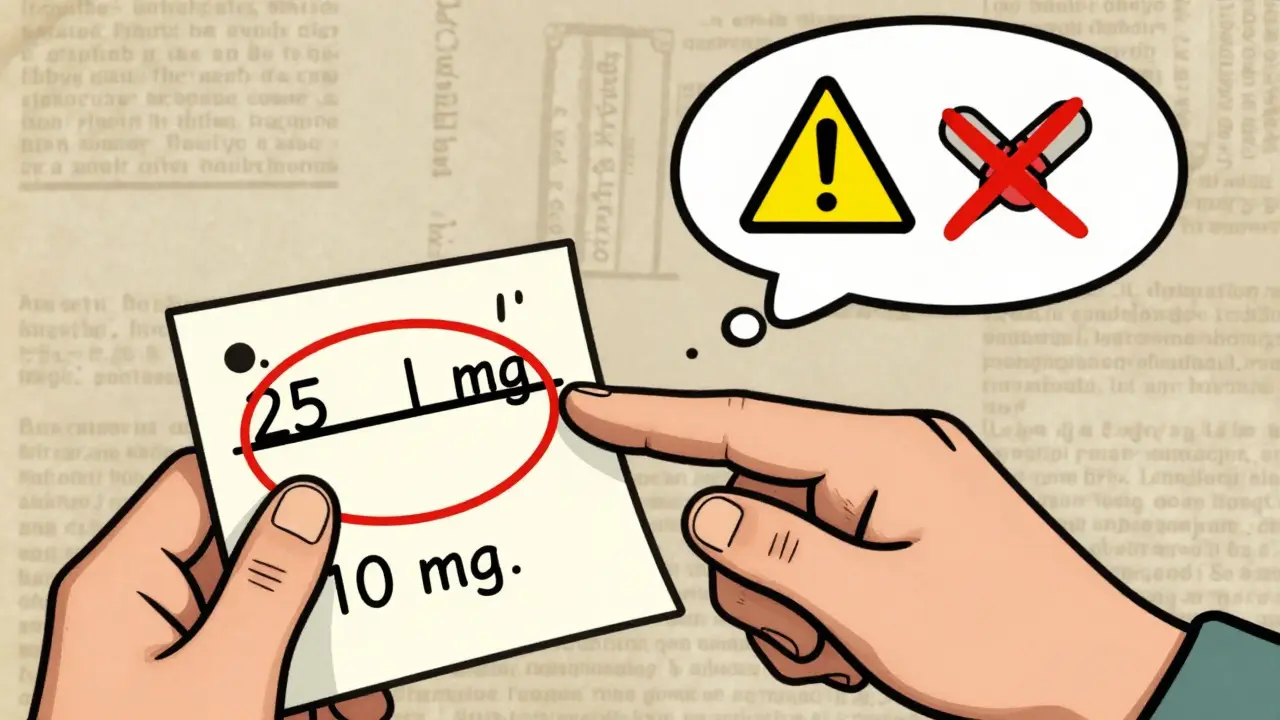
- The strength and dosage - This is the #1 error type. If your doctor prescribed 10 mg and the bottle says 25 mg, that’s a problem. Dosage mistakes make up over one-third of all prescription errors.
- The quantity - Count the pills. If you were supposed to get 30 tablets and there are only 27, ask why. A 2022 Providence Health study found that 22.8% of quantity errors are caught only when patients count immediately.
- The instructions - Does it say “take one tablet by mouth twice daily”? Or does it say “take one tablet by mouth qid”? If you don’t understand the directions, ask the pharmacist to explain. Illegible or unclear instructions cause nearly 19% of errors.
- The expiration date and packaging - Is the bottle sealed? Is the date still valid? Expired or damaged meds can be ineffective or dangerous. In 2023, 4.1% of recalled medications reached patients because no one checked.
- The NDC number - It’s the 11-digit barcode on the label. You don’t need to memorize it, but if you have a smartphone, open the FDA’s NDC directory and search for it. If the drug name or strength doesn’t match what’s on the bottle, it’s a red flag.
What to Say - The Three Questions Every Patient Should Ask
Pharmacists don’t mind questions. In fact, 92% of them encourage patients to ask. Here are the three questions the FDA says you should always ask:
- What is this medication for? - If you’re unsure why you’re taking it, you might miss warning signs. For example, if you’re given a new pill for “joint pain” but your doctor never mentioned arthritis, double-check.
- How and when should I take it? - Some meds need to be taken with food. Others can’t be taken with grapefruit juice. Timing matters. Taking a blood pressure pill at night instead of morning can cause dizziness or falls.
- What side effects should I watch for? - Not all side effects are dangerous. But if you’re told “drowsiness is normal” and you’re a truck driver, that’s a problem. Know what’s expected - and what’s not.
Pro tip: Write these questions down before you go. Don’t rely on memory. You’re already stressed. Let your phone or a note card do the work.
Common Problems - And How to Fix Them
You’re not alone if you’ve struggled with any of these:
- Small print on the label - Over 64% of patients over 65 say they can’t read the small text. Ask for a magnifying glass - most pharmacies keep them behind the counter. Or take a photo with your phone and zoom in.
- Generic vs. brand confusion - If your doctor wrote “Lisinopril” but you’ve always taken “Zestril,” that’s okay - they’re the same drug. But if you get a pill that looks nothing like your usual one, ask why. A 2022 ISMP report found 38.7% of first-time users didn’t recognize their generic meds.
- Time pressure from staff - Pharmacies are busy. But if someone rushes you, say: “I need a minute to check this.” You have the right to take your time. No one should make you feel bad for protecting your health.
- Pharmacists dismiss your concerns - If you raise a red flag and they say, “Oh, that’s fine,” walk out. Call the pharmacy’s corporate office. In 2023, CMS found that 63% of patients who reported errors were ignored or told they were wrong.
What’s Changing - And Why It Matters
Pharmacies are getting better at catching errors - but not because they’re nicer. They’re being forced to.
Since 2023, the Drug Supply Chain Security Act requires every prescription to have a unique product identifier with NDC, serial number, lot number, and expiration date. That means if a bottle gets recalled, they can trace it down to the exact pill you got.
Most pharmacies now use barcode scanners to match your script to the bottle. In 2015, only 45% had them. Today, 87% do. That’s cut identification errors by over 80%. But scanners don’t catch everything. They can’t tell if the strength is wrong or if the instructions are confusing.
Some pharmacies - like CVS and Walgreens - now have “verification stations” with tablets where you can scan your prescription and see a picture of the actual pill before you pick it up. It’s not everywhere yet, but it’s coming.

Why This Matters More Than You Think
Medication errors don’t just cause discomfort. They lead to hospital visits, falls, organ damage, and even death. The cost? Over $200 billion a year in the U.S. alone.
But here’s the good news: every dollar spent on patient verification saves $8.73 in avoided hospital stays and emergency care. That’s why Medicare now penalizes pharmacies with error rates above 0.85%. They’re being fined for mistakes you could’ve stopped.
And it’s not just about saving money. It’s about trust. A 2023 Trustpilot analysis found that pharmacies rated 4.2 stars or higher were 3.7 times more likely to encourage patients to check their meds. The ones that say, “Let me show you the bottle,” are the ones you want to go to.
What to Do If You Spot an Error
If you catch something wrong:
- Don’t leave the pharmacy.
- Stay calm. Say: “I think there might be a mistake here. Can we double-check?”
- Point to exactly what’s wrong - the name, the strength, the count.
- Ask to speak with the pharmacist in charge if the first one brushes you off.
- If they refuse to fix it, call the pharmacy’s corporate hotline. Most have a 24/7 patient safety line.
And if you’re ever unsure - even a little - take the bottle home. Call your doctor’s office. Ask for clarification. Better safe than sorry.
Final Reminder: You’re the Last Line of Defense
Pharmacists are trained professionals. But they’re human. They work fast. They get interrupted. They make mistakes. And if you don’t check your prescription, no one else will.
Don’t wait for a disaster to happen. Make checking your meds part of your routine - like buckling your seatbelt. It takes less than three minutes. But it could save your life.




10 Comments
Dana Termini
January 6, 2026 at 05:09
I never thought to check the NDC number until my mom got the wrong blood thinner. Turned out the barcode scanned fine but the strength was off by 5x. She ended up in the ER. Now I always double-check. It’s not paranoia-it’s survival.
Pavan Vora
January 7, 2026 at 18:19
In India, we don't have this luxury... Pharmacies often just hand you the bottle and say 'take it'. No one checks. I once got a cough syrup labeled as 'paracetamol' but it was actually a steroid. Took me three days to realize I was swelling like a balloon. No one believed me until I showed the bottle to a doctor. Please, if you're lucky enough to live somewhere with checks-USE THEM.
Stuart Shield
January 9, 2026 at 00:49
I love how this post breaks it down like a checklist-so practical. The part about the NDC directory? Genius. I used to just assume the pharmacist knew what they were doing. Turns out, I was just hoping. Now I whip out my phone and verify every time. It feels like having a superpower. And honestly? The pharmacists seem kinda impressed. Like, ‘Oh, you actually know what an NDC is?’ Yeah, I do now.
Ashley S
January 9, 2026 at 03:50
This is why people are so dumb. If you can’t read a pill bottle, maybe you shouldn’t be taking pills. Stop being so helpless. Just trust the system.
Jeane Hendrix
January 10, 2026 at 22:17
I’ve been using this checklist since my last med mix-up-turns out ‘Metoprolol’ and ‘Metoprolol Succinate’ are different formulations and I was taking the wrong one for months. The pharmacy said ‘it’s close enough.’ Close enough to cause atrial fibrillation, apparently. Now I screenshot the FDA page for each med and compare. It’s a pain, but I’d rather be annoying than dead. Also, the ‘qid’ thing? I had no idea that meant four times a day. So much jargon. So dangerous.
Kelly Beck
January 11, 2026 at 10:40
Y’ALL. I just started using this checklist and OMG it changed my life. 🙌 I caught a 2x overdose on my thyroid med last week because I counted the pills. The pharmacist was like, ‘Whoa, how’d you catch that?’ I said, ‘Because I’m not dying today.’ She gave me a free bag of gummies. I’ve never felt so powerful. Seriously, if you’re reading this and you’re still just grabbing your script and running-STOP. BREATHE. CHECK. You’re worth it. 💪❤️
Beth Templeton
January 12, 2026 at 17:21
Wow. A 3-minute checklist. What a revolutionary idea. Next you'll tell us to wash our hands before eating.
Cam Jane
January 13, 2026 at 23:43
I work at a pharmacy. I see this every day. People rush in, grab their meds, leave. Then they come back a week later with rashes, dizziness, or worse. We’re not trying to be rude-we’re swamped. But if you ask, ‘Is this right?’ we’ll stop everything. Seriously. We want you to ask. We’re not robots. We’re humans who want you to live. So ask. Always ask. Even if you’re embarrassed. Even if you think you’re being annoying. You’re not. You’re saving your own life.
Indra Triawan
January 14, 2026 at 15:05
We are all just temporary vessels for chemical signals, aren't we? The pills, the labels, the NDC numbers-they’re all illusions of control. The body knows what it needs. The pharmacy is just a modern temple of doubt. What if the real error is believing we need to verify anything at all?
Susan Arlene
January 15, 2026 at 06:32
I used to think this was overkill. Then my aunt died from a wrong dose of warfarin. They gave her 10mg instead of 1mg. No one noticed. Not her. Not the pharmacist. Not the doctor. Just me, reading the bottle two days later. Now I check everything. Even if I’m in a hurry. Even if I’m tired. Even if I’m crying. I check. Because I learned the hard way: if you don’t, no one else will.