Antihypertensive Combination Generics: What’s Available and How to Get It
Why combination pills for high blood pressure matter
Most people with high blood pressure don’t need just one pill. They need two, sometimes three. That’s not opinion-it’s science. About 70% to 80% of patients can’t get their blood pressure under control with a single medication. The Joint National Committee on Hypertension laid this out back in 2003, and nothing’s changed since. That’s why doctors now routinely prescribe antihypertensive combination generics-single pills that pack two or even three blood pressure drugs into one tablet.
It’s not just about convenience. Taking fewer pills means people actually remember to take them. Studies show adherence jumps 15% to 25% when patients switch from three separate pills to one combo pill. And for someone trying to avoid a stroke or heart attack, that’s huge.
What’s in these combo pills?
These aren’t magic pills. They’re smart combinations of proven drugs from different classes that work together better than alone. The most common pairings you’ll see in generic form:
- ACE inhibitor + thiazide diuretic (like lisinopril and hydrochlorothiazide)
- ARB + thiazide diuretic (like losartan and HCTZ)
- Calcium channel blocker + ACE inhibitor (like amlodipine and benazepril)
- Triple combos (amlodipine + valsartan + HCTZ)
These are the same drugs you’d get as separate pills, just packaged together. The FDA requires that generic versions match the brand-name version within 80% to 125% of the same blood levels-meaning they work just as well. No guesswork. No hidden ingredients.
Cost comparison: combo vs. separate generics
Here’s where it gets messy. A few years ago, combo pills were cheaper than buying the individual drugs. That’s not always true anymore.
Take amlodipine and valsartan. If you buy them separately as generics, you’re looking at about $4.50 and $7.80 per month respectively. That’s $12.30 total. The combo pill? Around $18.75. Same drugs. Same effectiveness. But the combo costs more.
But here’s the twist: if your insurance covers the combo pill at $10 a month but charges you $5 per separate pill, then the combo wins. It all depends on your plan. GoodRx data from October 2023 shows some combo generics like Hyzaar (losartan/HCTZ) as low as $10.60 a month. Others, like Lotensin HCT (benazepril/HCTZ), still hover around $38. Prices vary wildly by pharmacy, location, and insurance.
Why your insurance might not cover the combo
One of the biggest frustrations patients report isn’t cost-it’s confusion. Many insurance plans still treat combo pills as brand-name drugs, even when the ingredients are generic. You might pay $5 for amlodipine, $5 for losartan, and $5 for HCTZ-but then get hit with $45 for the same three drugs in one pill.
Why? Because insurers often have preferred lists (formularies) that favor individual generics. They don’t always update these lists when combo generics become available. Some plans even require you to try the separate pills first before approving the combo. That’s backwards. If you’re taking three pills a day, why make you jump through hoops?
Patients on Reddit and PatientsLikeMe say this is a common roadblock. One user wrote: “My pharmacy costs $12 for the combo. My insurance charges me $45. I switched back to three pills. I forget one every other day.”
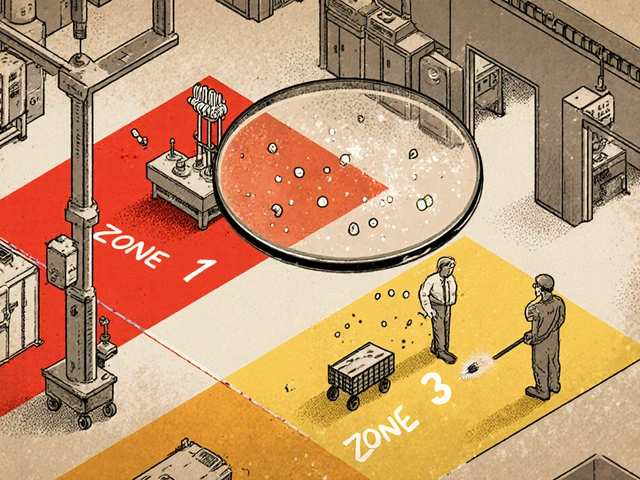
What doses are actually available?
Not every combination comes in every dose. That’s the hidden limitation.
Take Azor (amlodipine + olmesartan). It’s available as 5mg/20mg or 10mg/40mg. But what if your doctor wants you on 2.5mg of amlodipine and 40mg of olmesartan? That combo doesn’t exist. You’d have to take two pills-one for each drug.
This rigidity is a real problem. Many patients need fine-tuned doses. If your combo doesn’t match your prescription, you’re stuck. And not all pharmacies stock every variation. Some only carry the most common doses, like amlodipine/benazepril 5mg/20mg. If you need 2.5mg/10mg, you might have to order it or switch brands.
Always check the exact dose before filling. A pill that looks the same might not be the right strength. Pharmacists can help, but they’re not always trained to catch these mismatches.
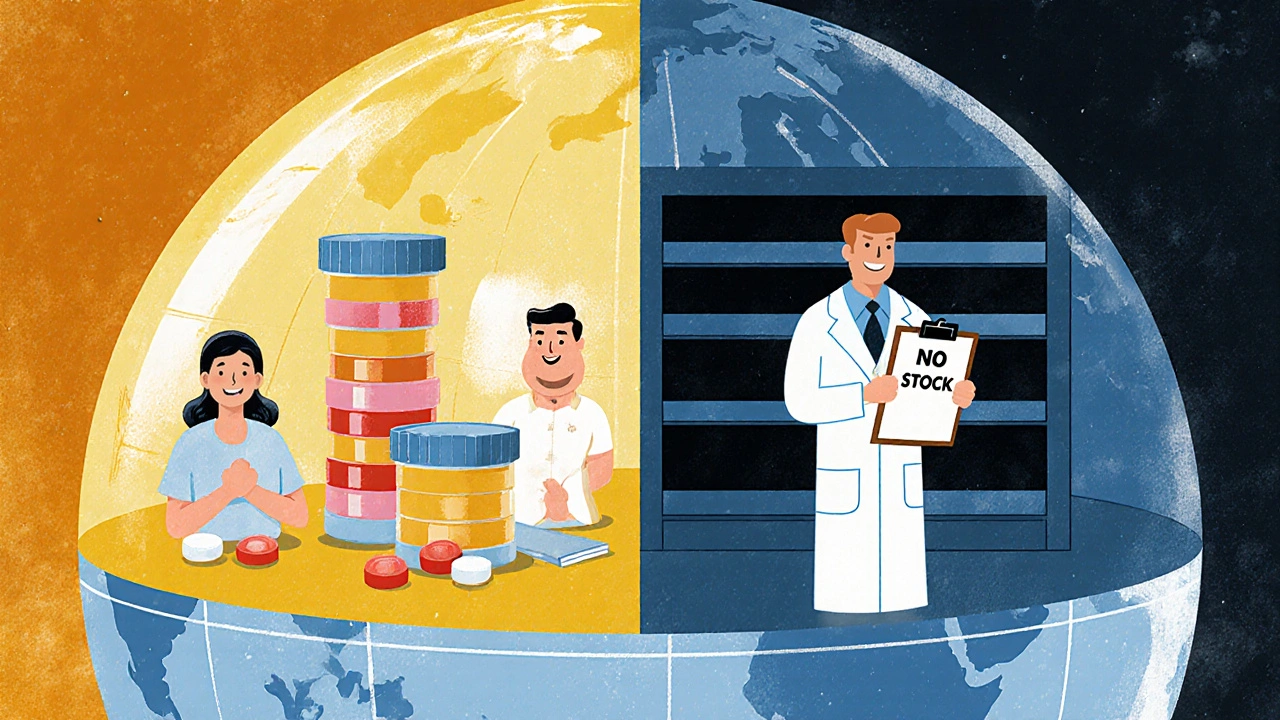
Global availability: it’s not the same everywhere
In the U.S., about 85% of antihypertensive combo prescriptions are generic. That’s high. But globally, it’s a different story.
A 2021 study looked at 26 low- and middle-income countries. Only 20 had confirmed access to generic combo pills. In places like Ethiopia, Afghanistan, and Turkey, even basic combinations were hard to find. The World Health Organization says 46% of low-income countries have less than 50% availability of essential antihypertensive medicines-including combos.
That’s not just a supply issue. It’s a policy failure. Even when the pills are available, they’re often not in national treatment guidelines. Doctors don’t know to prescribe them. Pharmacies don’t stock them. Patients don’t ask for them.
In high-income countries, combo pills cut hospitalizations for uncontrolled hypertension by nearly a third. In low-income countries, only 7% of people with high blood pressure get it under control. Access to these pills is one of the biggest reasons why.
What’s changing in 2025?
The FDA released new draft guidance in September 2023 to make it easier to approve new generic combo pills. That means more options are coming. Triple-combination pills (three drugs in one) are already growing fast. One 2022 study predicted they could reduce the global hypertension treatment gap by 35% if widely available.
But here’s the catch: availability doesn’t equal access. Even if a pill is approved and manufactured, it won’t help if it’s too expensive, not in guidelines, or not stocked locally. Real progress means better pricing, provider education, and inclusion in public health programs-not just more FDA approvals.
How to get the right combo pill
If you’re on multiple blood pressure meds, ask your doctor: “Is there a generic combo pill that matches my current doses?”
Then, check prices:
- Use GoodRx or SingleCare to compare cash prices for the combo vs. individual pills.
- Call your pharmacy and ask: “What’s the cash price for amlodipine/losartan 10mg/100mg?”
- Ask your insurer: “Do you cover this combo as a Tier 1 generic?”
- If the combo is more expensive than the separate pills, ask your doctor to prescribe the individual generics.
Don’t assume the combo is cheaper. Don’t assume your insurance will cover it. Do the math. Ask questions. Your blood pressure-and your wallet-will thank you.
What to watch out for
- Dose mismatch: If your combo doesn’t match your exact dose, you might need to split pills or take two.
- Insurance traps: Some plans charge more for the combo even when the ingredients are cheap.
- Stock shortages: Not all pharmacies carry every combo. Call ahead.
- Side effects: Combos can increase side effects like dizziness or low potassium. Monitor with your doctor.
There’s no one-size-fits-all solution. But with the right combo pill, you can simplify your routine, save money, and take control of your health-without extra pills or confusion.





15 Comments
Joe bailey
November 26, 2025 at 05:58
I switched to a combo pill last year and my BP dropped like a rock. Also, I actually remember to take it. No more pill organizer chaos. Life changed.
Amanda Wong
November 27, 2025 at 01:47
This is pure pharmaceutical industry propaganda. Combo pills are designed to lock you in. They’re not cheaper. They’re not better. They’re just more profitable for Big Pharma.
james thomas
November 28, 2025 at 20:17
Let’s be real-insurance companies are the real villains here. I paid $5 for lisinopril and $6 for HCTZ separately. The combo? $42. Same exact chemicals. They just repackaged it and called it a ‘premium product’. Pure scam.
Deborah Williams
November 29, 2025 at 13:43
It’s funny how we treat medicine like a grocery store. ‘Oh, let me compare prices on this life-saving combo pill.’ We’ve turned human health into a spreadsheet. And yet we’re shocked when people stop taking their meds because they can’t afford the math.
Kaushik Das
December 1, 2025 at 07:09
In India, we’ve got these combos for like $2 a month. Seriously. Amlodipine + telmisartan? Under 100 rupees. Meanwhile, Americans are paying $40 for the same thing. The global inequality in healthcare isn’t just a statistic-it’s someone’s grandfather skipping doses because he can’t afford the combo.
Asia Roveda
December 2, 2025 at 15:08
If you’re not taking three separate pills, you’re not serious about your health. Combo pills are for lazy people who want to avoid responsibility. My grandfather took six pills a day and lived to 92. You think he cared about convenience?
Micaela Yarman
December 3, 2025 at 07:08
The clinical evidence supporting fixed-dose combinations is robust, well-documented, and endorsed by the American Heart Association. Adherence rates improve significantly, and cardiovascular event reduction is statistically significant. The economic argument is secondary to the clinical imperative.
Aaron Whong
December 4, 2025 at 12:13
The pharmacokinetic synergy of RAS inhibitors with CCBs and diuretics creates a non-linear reduction in arterial stiffness and endothelial dysfunction. The combo isn’t just additive-it’s synergistic. The data from the ALLHAT and ACCOMPLISH trials are unequivocal.
Sanjay Menon
December 5, 2025 at 05:59
I used to think combo pills were a gimmick. Then I tried them. Now I feel like I’m living in a dystopian healthcare system where the only thing more expensive than the medicine is the moral compromise it takes to accept it.
Cynthia Springer
December 5, 2025 at 22:07
Does anyone know if there’s a combo pill with spironolactone? My doctor says it’s the best for my type of hypertension, but I can’t find any. Is it just not available, or am I missing something?
Rachel Whip
December 7, 2025 at 14:39
If you’re on amlodipine and lisinopril, check if your pharmacy has the combo version under $10. I found it at Walmart for $8.99. GoodRx saved me $30 a month. Seriously, always check.
Ali Miller
December 8, 2025 at 00:41
The government lets Big Pharma get away with this because they’re too busy kissing up to lobbyists. Meanwhile, my neighbor died from a stroke because she couldn’t afford her meds. This isn’t healthcare. It’s a blood sport.
JAY OKE
December 8, 2025 at 02:39
I take a combo. It’s $12. My other pills were $18. I’m not mad. I just take it. Life’s too short to count pills.
Stephen Adeyanju
December 8, 2025 at 21:20
Combo pills are the future why are we even arguing this my dad took three pills and forgot them all the time now he takes one and his BP is perfect end of story
mohit passi
December 10, 2025 at 15:49
In my village in Punjab, the local clinic gives out combo pills for free. No insurance. No pharmacy. Just a doctor and a box of pills. We don’t need fancy apps or GoodRx. We need the same system here. 🌍❤️