Itchy Skin & Allergies: How to Spot Triggers and Soothe Symptoms
When your skin itches nonstop, you’re probably dealing with itchy skin (pruritus) - an uncomfortable sensation that forces you to scratch and often points to an allergy or other irritation. It’s easy to blame dry air or a new detergent, but the real culprit might be hiding in the foods you eat, the pollen drifting outside, or even a hidden chemical on your favorite shirt. This guide walks you through how to identify the triggers, what tests can confirm them, and practical steps to calm the itch without turning skin into a battlefield.
What Exactly Is Itchy Skin?
Medical professionals call the urge to scratch pruritus. While a brief itch after a mosquito bite is normal, chronic pruritus is a sign that something in the body is over‑reacting. The skin’s nerve fibers release chemicals like histamine, which bind to receptors and send the itching signal to the brain. When an allergy is involved, the immune system produces IgE antibodies that recognize a specific allergen and trigger a cascade of histamine release.
How Allergies Spark the Itch
Allergies occur when the immune system mistakenly identifies a harmless substance as dangerous. The response usually shows up as sneezing, watery eyes, or a rash. In the case of skin, two common allergic conditions are urticaria (hives) and contact dermatitis. Both lead to redness, swelling, and relentless itching. Even eczema can flare up when allergens are present, creating a vicious cycle of dry, cracked skin that scratches itself even more.
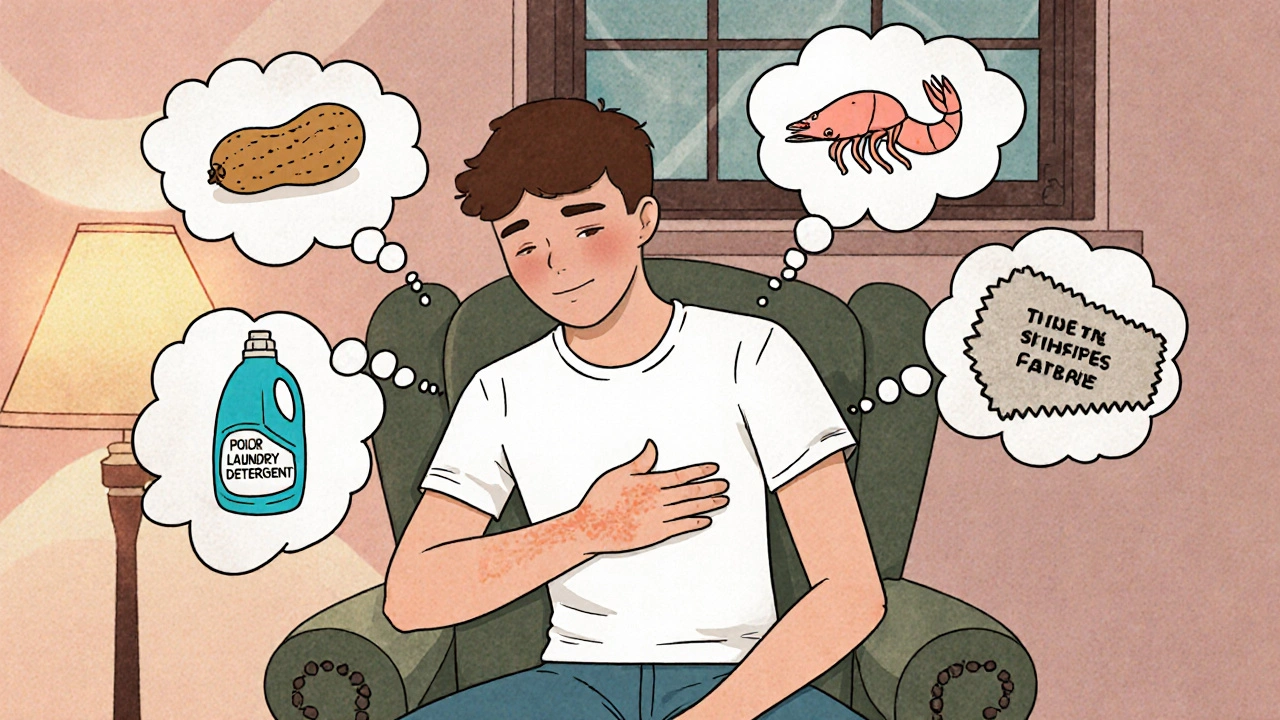
Common Triggers to Watch
Knowing what to look for saves you countless hours of frustration. Below is a quick snapshot of the most frequent offenders.
- Food allergens: peanuts, shellfish, dairy, eggs, and soy are top triggers for many adults and children.
- Environmental allergens: pollen, mold spores, dust mites, and pet dander can settle on skin or be inhaled, then circulate through the bloodstream.
- Contact irritants: harsh soaps, fragrances, nickel in jewelry, latex gloves, and even certain fabrics can provoke contact dermatitis.
It’s worth noting that some people react to multiple categories simultaneously, making a precise diagnosis essential.
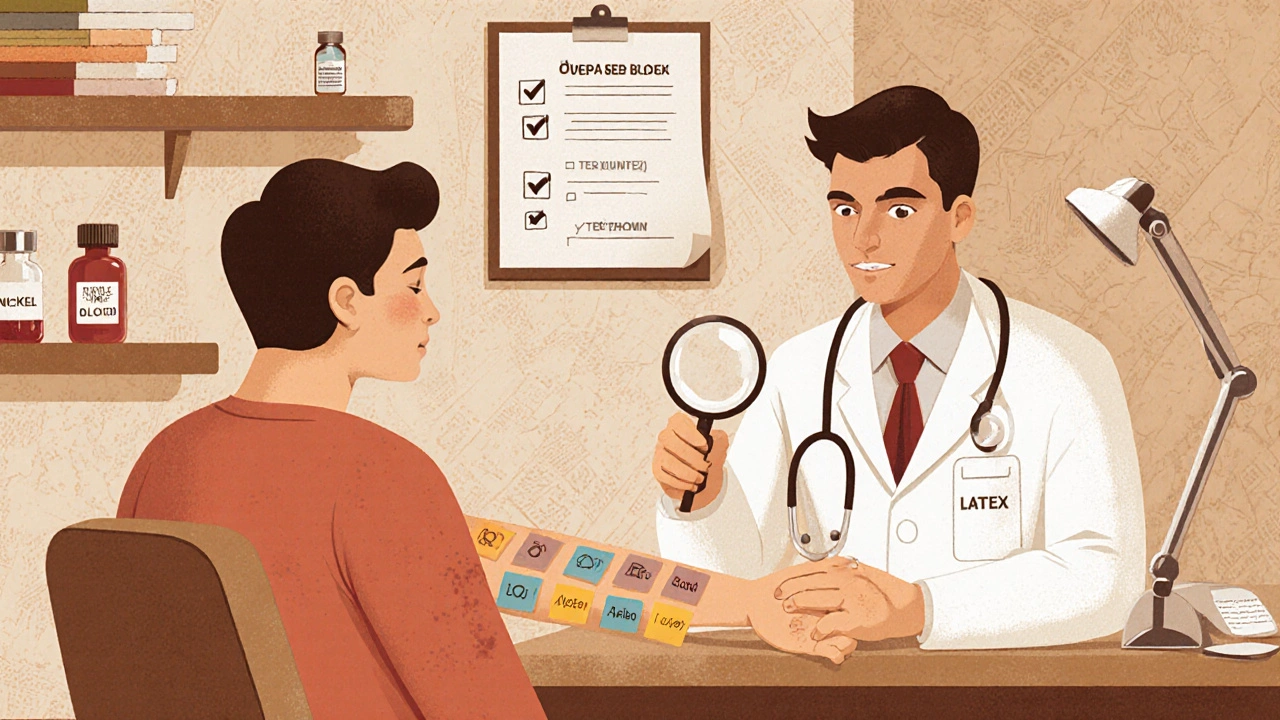
Diagnosing the Root Cause
Self‑diagnosis is tempting but often inaccurate. Here are the most reliable methods doctors use.
- Medical history review: A clinician will ask detailed questions about diet, recent changes in laundry products, pet exposure, and any previous allergy tests.
- Physical examination: Visual clues-like the shape of a rash or the distribution pattern-help differentiate between urticaria, eczema, and contact dermatitis.
- Patch testing: Small amounts of common allergens are placed on the skin under adhesive patches for 48 hours. A positive reaction usually appears within 48-72 hours.
- Blood tests: Measuring specific IgE levels can indicate whether a systemic allergy is at play, especially for food triggers.
If you notice a pattern-like itching after a new laundry detergent-bring that information to your dermatologist or allergist. Early detection prevents chronic skin damage.
Managing Symptoms Right Now
While you’re waiting for test results, there are several evidence‑based ways to tame the itch.
- Cold compress: Applying a clean, cool cloth for 10‑15 minutes narrows blood vessels and reduces histamine release.
- Gentle moisturizers: Fragrance‑free creams containing ceramides or oatmeal create a barrier that locks in moisture and calms nerve endings.
- Oral antihistamines: Non‑sedating options like loratadine or cetirizine block histamine receptors, providing relief for many allergy‑related itches.
- Topical corticosteroids: Low‑strength creams (1% hydrocortisone) reduce inflammation in localized flare‑ups. Use only as directed to avoid skin thinning.
- Prescription options: For severe cases, doctors may recommend oral steroids, immunomodulators, or newer biologic agents that target specific immune pathways.
Never scratch aggressively. Scratching breaks the skin’s protective layer, inviting infection and worsening inflammation.
Prevention Strategies to Keep Itch at Bay
Long‑term control hinges on removing or minimizing exposure to known triggers.
- Allergy‑proof your home: Use dust‑mite‑cover pillowcases, keep humidity below 50 % to deter mold, and wash bedding in hot water weekly.
- Read product labels: Look for “fragrance‑free,” “hypoallergenic,” and avoid known irritants like parabens or formaldehyde releasers.
- Adjust your diet: If food allergens are suspected, an elimination diet (under professional supervision) can pinpoint the problem.
- Choose skin‑friendly fabrics: Cotton, bamboo, or silk are less likely to cause contact dermatitis than synthetic blends.
- Regular skin care routine: Short, lukewarm showers, mild cleansers, and immediate moisturization keep the skin barrier intact.
When to Seek Professional Help
If any of the following occur, schedule an appointment with a dermatologist or allergist promptly:
- Itch persists for more than two weeks despite home measures.
- Rash spreads rapidly, looks blistered, or oozes fluid.
- Signs of infection appear-redness, swelling, warmth, or pus.
- You experience difficulty breathing, swelling of lips or tongue, or hives covering large areas (possible anaphylaxis).
Professional evaluation can prevent complications like chronic eczema, skin thickening from repeated scratching, or secondary bacterial infections.

Quick Reference Checklist
- Identify recent changes in products, diet, or environment.
- Track flare‑ups in a diary: date, location, suspected trigger.
- Use a cool compress and fragrance‑free moisturizer at the first sign of itch.
- Try a non‑sedating antihistamine for 24‑48 hours; note improvement.
- Schedule a patch test or blood test if the cause remains unclear.
- Follow up with a dermatologist if symptoms linger or worsen.
Comparison of Common Triggers and Recommended First‑Line Treatments
| Trigger Type | Typical Manifestation | Immediate Relief | Long‑Term Control |
|---|---|---|---|
| Food allergens | Widespread itching, hives, sometimes GI upset | Antihistamine + cool compress | Elimination diet + allergy testing |
| Environmental (pollen, dust) | Itchy patches on exposed skin, seasonal flare‑ups | Antihistamine, nasal spray | Air purifiers, dust‑mite covers, seasonal avoidance |
| Contact irritants | Localized redness, blisters, sharp itching | Cold compress, topical steroid | Switch to hypoallergenic products, patch testing |
| Eczema flare‑up (often allergy‑driven) | Dry, scaly patches that itch intensely | Moisturizer + antihistamine | Barrier repair creams, trigger avoidance, specialist care |
Bottom Line
Persistent itchy skin rarely solves itself without a plan. By pinpointing the allergen, using proven symptom‑relief methods, and building a trigger‑avoidance routine, you can break the itch‑scratch cycle and protect your skin’s health for the long haul.
What is the difference between a rash and simple itching?
A rash includes visible changes like redness, bumps, or blisters, while simple itching may occur without any skin alteration. Rashes often signal an underlying irritation or allergy that needs targeted treatment.
Can stress cause itchy skin?
Yes. Stress releases cortisol and other hormones that can heighten inflammation and make nerve endings more sensitive, worsening existing itching or even triggering new flare‑ups.
How long should I wait before using a steroid cream?
If the itch is intense, a low‑strength over‑the‑counter steroid (1% hydrocortisone) can be applied for up to 7 days. For stronger prescriptions, a doctor will set a specific duration to avoid skin thinning.
Is it safe to take antihistamines every day?
Non‑sedating antihistamines are generally safe for daily use, but long‑term reliance should be discussed with a healthcare provider to rule out underlying conditions.
What should I do if my skin becomes infected after scratching?
Clean the area with mild soap and water, apply an antibiotic ointment, and see a doctor promptly. Oral antibiotics may be needed if the infection spreads.




8 Comments
Kelvin Egbuzie
October 23, 2025 at 23:21
Oh sure, the “simple” itch you’re feeling is just the result of a rogue detergent, not a massive, covert operation by the skincare industry to sell you more moisturizers. 😒 They probably spiked your lotion with nanobots that tickle your nerves for profit. If you think patch testing is harmless, think again-someone’s definitely watching the data. Just remember, the only real cure is staying off the grid and using oat‑infused water straight from the tap. 🙄
Katherine Collins
November 9, 2025 at 15:09
lol u soundt mad, i just use plain water n hope for the best 😂
Taylor Nation
November 26, 2025 at 07:57
Hey folks, great rundown! If you’re itching, start a simple diary-note the time, what you ate, and any new soaps. Spotting patterns can cut weeks off the trial‑and‑error phase. Also, keep showers lukewarm and slap on a fragrance‑free moisturizer within three minutes; that locks in moisture and calms nerves. Let’s get those itch cycles broken! 💪
Shermaine Davis
December 13, 2025 at 00:45
Thx Tay! I alwys forget to do the 3‑min rule, sooo helpful 😅
tatiana anadrade paguay
December 29, 2025 at 17:33
Everyone’s skin is unique, so it’s important to approach trigger‑identification as a team effort. Start by involving family members who share your living space-they might notice subtle changes you miss. Also, consider swapping to organic cotton bedding; it reduces potential nickel or chemical exposure that’s often invisible. Remember, staying patient and compassionate with yourself makes the process less stressful.
Kristin Violette
January 15, 2026 at 10:21
When we interrogate pruritus through the epistemological lens of immunology, we quickly realize that the itch response is not a mere peripheral phenomenon but a distributed network of neuro‑immune crosstalk. Histamine, while prominently featured, is merely the tip of the iceberg; cytokines such as IL‑31 and thymic stromal lymphopoietin orchestrate a cascade that sensitizes cutaneous nociceptors. The ontogeny of this sensitization can be traced to epithelial barrier dysfunction, wherein filaggrin mutations precipitate transepidermal water loss and subsequent allergen permeation. Moreover, the microbiome exerts a modulatory effect, with dysbiosis amplifying Th2 skewing and perpetuating chronic itch. From a systems‑theoretic standpoint, one must consider feedback loops: scratching breaches the stratum corneum, inviting opportunistic pathogens that further inflame, thereby reinforcing the itch–scratch cycle. Environmental xenobiotics, such as volatile organic compounds in fragranced personal care products, act as exogenous adjuvants, potentiating antigen presentation. In clinical praxis, patch testing serves as a controlled perturbation, revealing latent hypersensitivities through a delayed‑type hypersensitivity response. Yet, purely mechanistic approaches overlook psychosocial variables; stress hormones like cortisol can upregulate mast cell degranulation, intertwining affective states with somatic symptoms. Consequently, a biopsychosocial management plan is paramount, integrating antihistaminic pharmacotherapy with barrier‑restorative moisturizers and cognitive‑behavioral strategies aimed at reducing compulsive scratching. Emerging biologics targeting the IL‑4Rα axis-dupilumab, for instance-demonstrate that precision immunomodulation can decouple the neuroimmune axis, offering sustained remission. However, accessibility and cost remain barriers, highlighting the socioeconomic stratification inherent in dermatologic care. Therefore, patient education regarding trigger avoidance, diligent skin care routines, and judicious use of topical corticosteroids remains the cornerstone of first‑line intervention. In summary, the pathogenesis of chronic pruritus is a multifactorial tapestry woven from immunologic, neurologic, environmental, and psychological threads, each demanding targeted attention for effective amelioration. Future research should focus on delineating the molecular signatures that predict therapeutic response, thereby personalizing treatment algorithms. Until then, interdisciplinary collaboration between dermatologists, allergists, and mental health professionals remains essential.
Diane Larson
February 1, 2026 at 03:09
Kristin nailed it-especially the part about IL‑31. In practice, I start patients on a daily liberal moisturizer plus a second‑generation antihistamine before considering biologics. If you’ve ruled out contact irritants, a short course of low‑dose prednisone can break the cycle, but always taper slowly to avoid rebound.
Michael Kusold
February 17, 2026 at 19:57
i’ve tried the cold compress trick and it actually chills the itch for a few minutes, super easy hack.