Combivir (Lamivudine & Zidovudine) vs Other HIV Antiretrovirals - 2025 Comparison Guide
HIV Regimen Decision Tool
Choose Your Treatment Considerations
Recommendation
Quick Takeaways
- Combivir is a twice‑daily NRTI combo (lamivudine + zidovudine) approved for treatment‑naïve adults.
- Modern single‑tablet regimens (e.g., Biktarvy, Descovy) offer once‑daily dosing and fewer drug‑drug interactions.
- Cost varies widely: generic Combivir ~ $30 / month, while brand‑name integrase‑inhibitor combos can be $1,200 / month.
- Resistance patterns differ - zidovudine resistance emerges faster than with newer agents.
- Side‑effect profiles: Combivir can cause anemia and mitochondrial toxicity; newer options tend toward milder GI and neuro‑psychiatric effects.
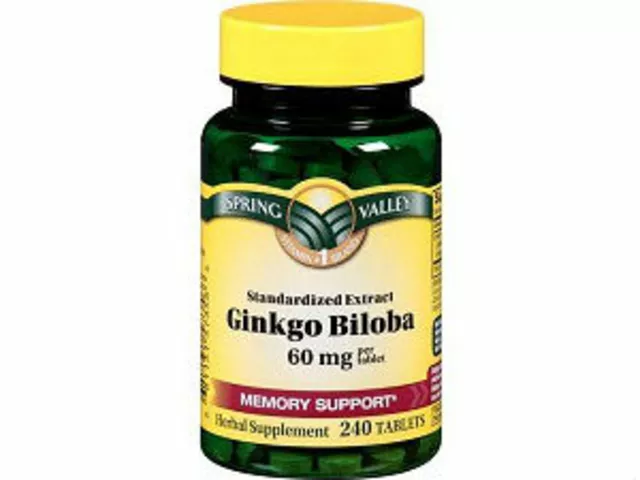
When it comes to antiretroviral therapy (ART) for HIV, Combivir is a fixed‑dose combination of two nucleoside reverse transcriptase inhibitors (NRTIs): Lamivudine and Zidovudine. The brand name Combivir combines these agents in a single tablet taken twice daily.
What Is Combivir?
Combivir was first approved by the FDA in 1997. Its purpose is to block the HIV reverse transcriptase enzyme, preventing the virus from copying its RNA into DNA. By delivering both lamivudine (3TC) and zidovudine (AZT) together, the pill raises the genetic barrier to resistance compared with using either drug alone.
Key attributes:
- Formulation: 150 mg lamivudine + 300 mg zidovudine per tablet.
- Dosing: 2 tablets per day (usually 600 mg AZT total).
- Typical cost (2025 US): $30‑$45 for a month’s supply of generic tablets.
- Common side effects: anemia, neutropenia, nausea, headache, mitochondrial toxicity.
How Combivir Works in the Body
Both lamivudine and zidovudine are incorporated into the growing viral DNA chain. Once added, they act as chain terminators, halting further elongation. The dual‑NRTI backbone is usually paired with a third drug - either a non‑nucleoside reverse transcriptase inhibitor (NNRTI) or an integrase strand transfer inhibitor (INSTI) - to form a full ART regimen.
Because zidovudine has a relatively short intracellular half‑life, the twice‑daily schedule helps maintain effective drug levels. Lamivudine, on the other hand, stays in cells longer, which is why some clinicians keep it in regimens even after switching away from zidovudine.
Modern Alternatives to Combivir
Since the early 2000s, newer ARVs have reshaped the treatment landscape. Below are the most common alternatives you’ll encounter in 2025.
- Tenofovir disoproxil fumarate (TDF) - a nucleotide reverse transcriptase inhibitor (NtRTI) with strong potency and once‑daily dosing.
- Emtricitabine (FTC) - a lamivudine‑like NRTI that pairs well with tenofovir.
- Truvada (TDF + FTC) - a once‑daily backbone used in many first‑line regimens.
- Biktarvy (bictegravir + emtricitabine + tenofovir alafenamide) - a single‑tablet, once‑daily regimen with a high barrier to resistance.
- Descovy (emtricitabine + tenofovir alafenamide) - similar to Truvada but with lower kidney‑ and bone‑impact.
- Kivexa (lamivudine + abacavir) - an alternative NRTI combo for patients with HLA‑B*5701 negative status.
- Dolutegravir‑based regimens (e.g., Triumeq) - integrate an INSTI with two NRTIs for a potent, once‑daily option.
Side‑Effect Profiles Compared
Understanding tolerability is crucial when picking a regimen. Below is a high‑level view of the most common adverse events.
- Combivir: anemia, neutropenia, nausea, mitochondrial toxicity (rare lactic acidosis).
- Truvada/Descovy: mild GI upset, potential renal phosphate loss (more with TDF), weight gain (especially with TAF‑based combos).
- Biktarvy: generally well‑tolerated; occasional insomnia or headache.
- Dolutegravir‑based regimens: insomnia, weight gain, rare neuropsychiatric effects.
Cost Comparison (2025 US Market)
| Regimen | Composition | Dosing Frequency | Typical Monthly Cost | Resistance Barrier |
|---|---|---|---|---|
| Combivir + NNRTI/INSTI | Lamivudine + Zidovudine | Twice daily | $30‑$45 (generic) | Medium - zidovudine resistance can emerge quickly |
| Truvada + INSTI (e.g., Bictegravir) | TDF + Emtricitabine | Once daily | $150‑$250 | High - tenofovir has a strong barrier |
| Descovy + INSTI | TAF + Emtricitabine | Once daily | $200‑$300 | High - TAF improves safety profile |
| Biktarvy | Bictegravir + Emtricitabine + TAF | Once daily | $250‑$350 | Very high - integrase inhibitor plus strong NRTI backbone |
| Kivexa + Dolutegravir | Lamivudine + Abacavir | Once daily | $180‑$260 | High - abacavir adds robustness |
Decision Guide - When to Choose Combivir vs Modern Regimens
Use the following checklist to see if Combivir still makes sense for a patient.
- Cost‑sensitivity: If insurance coverage is limited or the patient pays cash, the generic price of Combivir can be a decisive factor.
- Pregnancy or Breastfeeding: Zidovudine has a long safety record in pregnancy, making Combivir a viable option when newer agents lack robust data.
- Renal or Bone Health: Patients with chronic kidney disease may avoid TDF/TAF‑based combos; Combivir does not strain the kidneys.
- Resistance History: If the virus already has zidovudine‑associated mutations, move away from Combivir.
- Adherence Capacity: Twice‑daily dosing requires reliable routines; if missed doses are a concern, favor once‑daily single‑tablet options.
If most of the above points are “no,” a modern once‑daily regimen is likely the better choice.
Potential Pitfalls & How to Manage Them
- Anemia: Monitor hemoglobin at baseline and after 4‑6 weeks. If drops >2 g/dL, consider switching zidovudine.
- Mitochondrial Toxicity: Watch for peripheral neuropathy or lactic acidosis; these are rare but serious.
- Drug Interactions: Zidovudine is metabolized minimally by CYP enzymes, so interactions are few, but watch for drugs that affect bone marrow (e.g., chemotherapy).
- Adherence Challenges: Use pillboxes, set alarms, or combine with a once‑daily backbone to simplify regimens.
Frequently Asked Questions
Is Combivir still recommended as first‑line therapy in 2025?
Guidelines now favor once‑daily integrase‑inhibitor regimens for most treatment‑naïve adults because they are simpler and have fewer side effects. Combivir may still be used when cost or specific pregnancy considerations dictate.
Can I switch from Combivir to Biktarvy without a wash‑out period?
Yes. Current DHHS guidelines allow a direct switch from a dual‑NRTI backbone to a single‑tablet INSTI regimen, provided the viral load is < 100,000 copies/mL and the patient has no documented resistance to the new drugs.
What monitoring is required after starting Combivir?
Baseline CBC, liver enzymes, and renal function are standard. Follow‑up CBC at 4‑6 weeks helps catch anemia early. Viral load should be checked at week 4 and month 3 to ensure suppression.
How does the resistance profile of zidovudine compare to tenofovir?
Zidovudine resistance can develop after 6‑12 months of monotherapy and often involves the M184V mutation. Tenofovir has a higher genetic barrier; resistance usually requires multiple mutations and is far less common.
Are there any food restrictions with Combivir?
Zidovudine absorption is slightly reduced with high‑fat meals, but the effect isn’t clinically significant. Taking the pills with a light snack can help reduce nausea.
Choosing the right HIV regimen is a balance of efficacy, safety, convenience, and cost. By weighing the points above, you can decide whether the classic Combivir combo still fits a patient’s needs or if a newer single‑tablet option offers a clearer path to viral suppression.



12 Comments
Gary Campbell
October 26, 2025 at 18:15
Listen, the pharma giants don’t want you to know that Combivir is basically a relic designed to keep the profit pipeline flowing while they push newer drugs that lock you into even higher prices. They market the single‑tablet regimens as "modern" but forget to mention the hidden fees in the fine print. Even the patent extensions on zidovine are a classic move to keep the old formulas alive just long enough to squeeze out every last dollar. Sure, the once‑daily pills sound convenient, but the real convenience is for the insurers, not the patients.
renee granados
October 27, 2025 at 14:00
What a load of nonsense. Combivir is cheap for a reason – it’s old and full of side effects. You’d rather be anemic than pay $300 a month for some fancy pill that does nothing but make you gain weight.
Barbara Ventura
October 28, 2025 at 12:13
Wow, this guide is packed with info, folks, really thorough, and I appreciate the breakdown of costs versus benefits, especially the side‑effect profiles, which can be a big deal for patients; the tables make it easy to compare, and the checklist at the end is super helpful, I’ll definitely keep it handy for my clinic.
laura balfour
October 29, 2025 at 10:26
Okay, let me break this down for ya - Combivir might be an old‑school option, but it’s not totaly worthless!!! It’s still used in pregnany cases where new drugs lack long‑term data… the evpuation of side‑effects is solid, but with the right monitoring you can manage those anemia issues. The cost factor is huge, especially for uninsured patients, so don’t dismiss it outright.
Ramesh Kumar
October 30, 2025 at 10:03
Let’s dive into the practical side of things. First, the cost advantage of generic Combivir cannot be overstated; at $30‑$45 per month it’s a viable option for patients without comprehensive insurance. Second, the dosing schedule of twice daily may seem burdensome, but for many patients it aligns with routine medication times, like morning and bedtime, which can actually improve adherence when paired with a reminder system.
Third, the side‑effect profile-anemia, neutropenia, and mitochondrial toxicity-requires regular monitoring. Baseline CBC and follow‑up at 4‑6 weeks are essential, and if hemoglobin drops more than 2 g/dL, a switch to a tenofovir‑based regimen should be considered.
Fourth, resistance patterns matter. Zidovudine resistance can emerge after about a year of therapy, especially if the viral load isn’t fully suppressed. This makes it less attractive for patients with prior treatment experience or known resistance mutations.
Fifth, pregnancy considerations are a real strength for Combivir. Zidovudine has a long history of safe use in pregnant women, reducing maternal‑to‑child transmission, which newer agents have yet to match in large cohort studies.
Sixth, renal and bone health: Unlike tenofovir disoproxil fumarate (TDF), Combivir doesn’t exert pressure on kidney function or bone mineral density, making it a safer choice for patients with chronic kidney disease or osteoporosis.
Seventh, drug‑drug interactions are minimal with zidovudine, simplifying regimens for patients on multiple medications, such as chemotherapy or antiepileptics.
Eighth, the flexibility to combine Combivir with various third agents (NNRTIs or INSTIs) provides clinicians with a customizable backbone that can be tailored to patient‑specific factors.
Ninth, the availability of generic versions ensures that even in low‑resource settings, patients can access effective therapy without financial ruin.
Tenth, adherence tools like pillboxes or smartphone alarms can mitigate the twice‑daily burden, turning a potential drawback into a manageable habit.
Eleventh, education is key: patients should understand the signs of anemia (fatigue, pallor) and be encouraged to report symptoms promptly.
Twelfth, regular viral load monitoring at weeks 4 and 12 helps confirm suppression and catch emerging resistance early.
Thirteenth, if a patient experiences intolerable side effects, clinicians should feel empowered to transition quickly to a single‑tablet regimen, which in 2025 offers comparable efficacy with better tolerability.
Fourteenth, always consider the individual’s lifestyle, comorbidities, and preferences before defaulting to the newest regimen; sometimes the older, cheaper option is the most appropriate.
Fifteenth, in summary, Combivir remains a cost‑effective, clinically useful option in specific scenarios-especially pregnancy, renal compromise, and limited insurance coverage-provided that vigilant monitoring and patient education are in place.
Barna Buxbaum
October 30, 2025 at 11:26
Great points on monitoring, Ramesh! I’d add that many clinics now use electronic health records to set automatic alerts for CBC checks, which really helps catch anemia early. Also, the newer INSTI‑based combos often have a smoother side‑effect curve, so if a patient is struggling with fatigue, a quick switch can make a big difference. Keep up the thorough work!
Alisha Cervone
October 30, 2025 at 12:50
Combivir is cheap.
asha aurell
October 30, 2025 at 14:13
Cheap but risky, especially with anemia.
Abbey Travis
October 30, 2025 at 15:36
Both of you raise valid concerns; the key is to match the regimen to the patient’s health status and financial situation, and ensure they’re fully informed about the monitoring requirements.
ahmed ali
October 30, 2025 at 17:00
Okay, so here’s the thing – everyone’s quick to throw around the word \"modern\" like it’s a badge of superiority, but let’s not forget that modern doesn’t always equal better for every single individual. For starters, the sheer convenience of a single‑tablet regimen is appealing, yes, but the price tag attached to those pills is astronomical, and that’s a reality many patients can’t afford. When you compare that to the $30‑$45 a month you can get for generic Combivir, the math is pretty clear. The price disparity isn’t just a number; it’s a barrier that can keep someone from staying in care altogether.
Next, the side‑effect profile – modern INSTI‑based combos certainly have fewer things like anemia, but they bring their own set of issues like weight gain, insomnia, and occasionally neuro‑psychiatric symptoms that can be just as debilitating if not managed properly. In contrast, anemic side effects from zidovudine are well‑documented and can be screened for early with routine CBCs. You know exactly what to look for and how to intervene.
Now, let’s talk about pregnancy. Zidodine – I mean zidovudine – has a long, solid track record for preventing mother‑to‑child transmission. The data on newer drugs in pregnancy isn’t as extensive, and for a lot of clinicians that uncertainty translates into caution. In settings where safer, proven options are needed, Combivir still has a foothold.
Renal considerations are another point – tenofovir disoproxil fumarate can be harsh on kidneys, and even tenofovir alafenamide isn’t completely free from renal concerns. Combivir, meanwhile, spares the kidneys. For patients with chronic kidney disease, that’s a huge plus.
Adherence is a common argument for once‑daily dosing, sure, but habit formation is personal. Some patients actually find a twice‑daily schedule easier to pair with meals or other medications, especially if they’re already used to it. Adding a reminder app or a pillbox can make that regimen just as reliable.
Finally, the resistance issue – yes, zidovudine resistance can emerge, but in treatment‑naïve patients with good viral suppression, the risk is mitigated, especially if you pair Combivir with a strong third drug like an INSTI. You get a decent barrier without the astronomical cost.
Bottom line: Don’t throw away the baby with the bathwater. Combivir is not the default option for every patient, but it remains a valuable tool in a clinician’s armamentarium, especially when cost, pregnancy, renal health, and known side‑effect management come into play. It’s about individualized care, not one‑size‑fits‑all hype.
Deanna Williamson
October 30, 2025 at 18:23
While Ahmed’s enthusiasm is noted, the reality remains that relying on older NRTI combos can expose patients to avoidable hematologic toxicity. A more balanced approach would prioritize newer agents when feasible, reserving Combivir for truly constrained scenarios.
Miracle Zona Ikhlas
October 30, 2025 at 19:46
Your point about balancing efficacy, safety, and cost is spot on. Let’s keep the conversation focused on patient‑centered decisions and ensure everyone has access to the best possible treatment plan.