Trimethoprim-Sulfamethoxazole and Warfarin: How This Antibiotic Can Raise Your INR and Increase Bleeding Risk
Warfarin-Bactrim INR Risk Estimator
How This Calculator Works
Based on clinical data, Bactrim can increase INR by 1.5-2.5 units in high-risk patients. This tool estimates your potential INR increase and recommends actions. Remember: INR over 4.0 requires medical attention.
Enter Your Information
Estimated Results
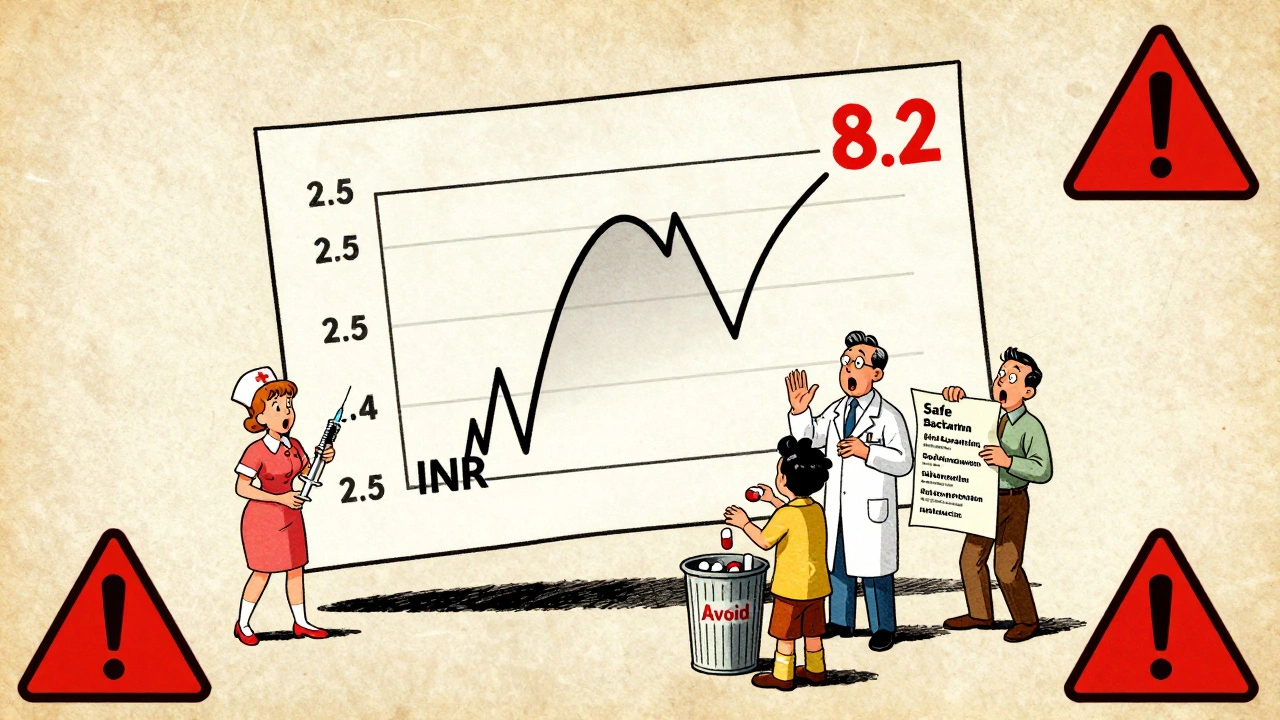
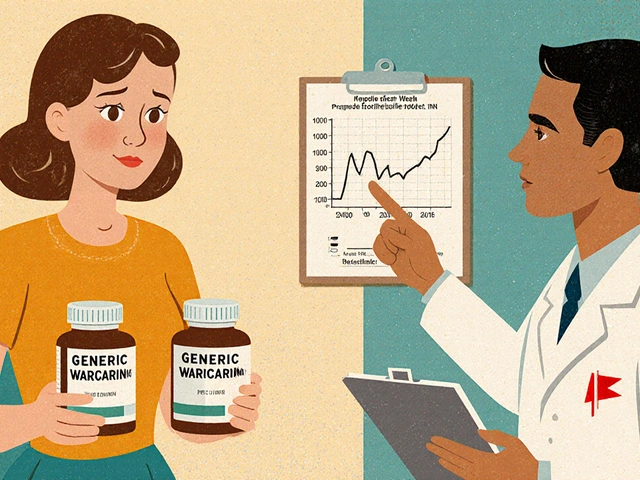
When you're on warfarin, even a simple antibiotic can turn dangerous. One of the most dangerous combinations you might not expect is trimethoprim-sulfamethoxazole (TMP-SMX), commonly sold as Bactrim or Septra, and warfarin. This isn’t just a theoretical risk - it’s a real, documented threat that sends people to the ER every year. If your INR suddenly spikes after starting this antibiotic, you could be at risk for serious, even life-threatening bleeding. And it doesn’t take much: just three days of Bactrim can push your INR from a safe 2.5 to a dangerous 6.0 or higher.
Why This Interaction Happens
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s a tightrope walk - too little, and you clot; too much, and you bleed. The drug is broken down in your liver by an enzyme called CYP2C9. Trimethoprim, one half of the TMP-SMX combo, is a moderate inhibitor of that same enzyme. When you take them together, your body can’t clear warfarin as fast. That means warfarin builds up in your blood, and your INR climbs. But that’s not all. Sulfamethoxazole, the other half, pushes warfarin off proteins in your blood. Warfarin normally sticks tightly to albumin - 97% to 99% of it. When sulfamethoxazole shows up, it kicks warfarin loose, flooding your bloodstream with free, active drug. Think of it like removing the brakes on a car. Suddenly, you’re going faster than you intended. There’s also a third factor: your gut bacteria. Some of them make vitamin K. TMP-SMX kills off those helpful bugs. Less vitamin K means your body has even less ability to counteract warfarin. It’s a triple hit: slower clearance, more free drug, and less vitamin K. No wonder INR jumps so fast.How Fast Does It Happen?
This isn’t a slow burn. Most patients see their INR rise within 36 to 72 hours after starting TMP-SMX. That’s why checking your INR before and after starting the antibiotic isn’t just good practice - it’s essential. A 2023 study in the Journal of Clinical Anticoagulation found that INR increased by an average of 1.8 units after starting Bactrim. Compare that to amoxicillin, which only raised INR by 0.4 units on average. That’s nearly five times the effect. One nurse practitioner in an anticoagulation forum reported multiple cases where elderly patients on warfarin had INRs jump from 2.5 to 6.0 after just two days of Bactrim for a urinary tract infection. In another case, a 78-year-old man with a mechanical heart valve saw his INR hit 8.2 after three days of TMP-SMX. He needed vitamin K and fresh frozen plasma to stabilize.Who’s at Highest Risk?
Not everyone reacts the same way. Some people take Bactrim and see no change in INR. Others crash into dangerous territory. Risk factors include:- Age over 75
- Heart failure, especially if it’s decompensated
- Liver disease
- Poor nutrition or low vitamin K intake
- Being male (studies show men are 9% more likely to have significant INR spikes)
What Do Experts Say?
The American Heart Association and the Institute for Safe Medication Practices both classify this interaction as high-alert. That means it’s one of the top 10 drug combinations that can cause serious harm if not managed properly. Dr. Gregory Makris, a leading anticoagulation expert, says bluntly: “TMP-SMX should be considered contraindicated in patients on warfarin unless absolutely necessary.” He recommends alternatives like nitrofurantoin for urinary tract infections - which have far less impact on INR. But not everyone agrees it’s always a hard stop. Dr. Jack Ansell, a hematologist, points out that some patients tolerate it fine. His advice? If you must use TMP-SMX, check INR within 48 hours. Don’t wait. Don’t assume. Test it.Real Numbers, Real Risks
The FDA’s Adverse Event Reporting System recorded 1,842 cases of INR elevation linked to TMP-SMX over five years. Nearly half of those cases led to hospitalization. And 68 people died from bleeding complications. A 2022 study in JAMA Internal Medicine found that nearly 1 in 5 warfarin patients were prescribed an interacting antibiotic within 30 days. TMP-SMX made up nearly 30% of those prescriptions - even though guidelines have warned about this for decades. Meanwhile, newer blood thinners like apixaban and rivaroxaban don’t interact with TMP-SMX the same way. But over 2.6 million Americans are still on warfarin - including 1.2 million with mechanical heart valves who can’t switch to newer drugs. That means this interaction isn’t going away anytime soon.What Should You Do?
If you’re on warfarin and your doctor suggests TMP-SMX, ask these questions:- Is there another antibiotic that won’t raise my INR? (Nitrofurantoin, doxycycline, or cephalexin are safer options for many infections.)
- If Bactrim is the only option, can we check my INR before and 48 hours after starting it?
- Should I reduce my warfarin dose ahead of time? (Some guidelines suggest cutting it by 20-30% in high-risk patients.)

What If Your INR Spikes?
If your INR goes above 4.0, don’t panic - but don’t ignore it either. Here’s what to do based on your INR level:- INR 4.0-5.0, no bleeding: Skip 1-2 doses of warfarin, then restart at a lower dose. Recheck INR in 2-3 days.
- INR 5.0-9.0, minor bleeding (bruising, nosebleeds): Take 1-2.5 mg of oral vitamin K. Recheck INR in 24 hours.
- INR over 9.0 or major bleeding (blood in urine, vomiting blood, severe headache): Go to the ER. You’ll likely need IV vitamin K (5-10 mg) and 4-factor prothrombin complex concentrate to reverse the effect fast.
How to Stay Safe
The National Blood Clot Alliance found that patients who got specific counseling about antibiotic-warfarin interactions had 37% fewer emergency visits for bleeding. That’s huge. Here’s what you can do:- Always tell every doctor and pharmacist you’re on warfarin - even for a simple sore throat.
- Keep a list of safe and unsafe antibiotics handy. Print it. Save it on your phone.
- Don’t take over-the-counter antibiotics or herbal supplements without checking with your anticoagulation clinic.
- Know your baseline INR. If you’re on a stable dose, know what your usual number is.
- Get your INR checked within 48 hours of starting any new antibiotic - even if you feel fine.
Bottom Line
Trimethoprim-sulfamethoxazole and warfarin don’t mix safely. The risk isn’t small. The consequences aren’t theoretical. This interaction has caused deaths. It’s preventable - but only if you act. Don’t assume your doctor knows. Don’t assume it’s safe because you’ve taken it before. Don’t wait for symptoms. Check your INR. Ask for alternatives. Be your own advocate. This isn’t about fear. It’s about control. You’re managing a powerful drug. You deserve to know what can break it - and how to fix it before it breaks you.Can I take Bactrim if I’m on warfarin?
Bactrim (trimethoprim-sulfamethoxazole) should be avoided if possible while on warfarin. It can cause your INR to spike dangerously within 2-3 days, increasing your risk of bleeding. Safer alternatives like nitrofurantoin or doxycycline are often available. If no other option exists, your INR must be checked within 48 hours of starting Bactrim, and your warfarin dose may need to be reduced.
How long does it take for INR to rise after taking Bactrim?
INR typically begins rising within 36 hours of starting Bactrim and peaks between 48 and 72 hours. That’s why checking your INR before and after starting the antibiotic is critical. Waiting longer than 72 hours puts you at higher risk for complications.
What antibiotics are safe with warfarin?
Antibiotics with minimal interaction risk include amoxicillin, cephalexin, doxycycline, and nitrofurantoin. Fluoroquinolones like ciprofloxacin carry moderate risk, and TMP-SMX is high-risk. Always confirm with your pharmacist or anticoagulation clinic before starting any new antibiotic - even over-the-counter ones.
What should I do if my INR goes above 5.0?
If your INR is above 5.0 and you have minor bleeding (like nosebleeds or bruising), take 1-2.5 mg of oral vitamin K and recheck your INR in 24 hours. If your INR is over 9.0 or you’re experiencing serious bleeding (blood in urine, vomiting blood, confusion), go to the emergency room immediately. You may need IV vitamin K and a clotting factor concentrate.
Can I take Bactrim if I’ve taken it before without problems?
Just because you took Bactrim before without an INR change doesn’t mean it’s safe this time. Your body changes - your liver function, diet, other medications, and even your gut bacteria can shift. A previous safe experience doesn’t guarantee safety now. Always check your INR before and after taking any antibiotic, even if you’ve used it before.



12 Comments
Sean McCarthy
December 2, 2025 at 03:53
Don't take Bactrim with warfarin. Period. I've seen three patients bleed out because someone thought it was fine. INR jumps fast. No warnings. No mercy.
soorya Raju
December 2, 2025 at 09:58
lol u think this is the only thing they hide from u? Big Pharma dont want u to know that vitamin K2 is the real cure but they sell u warfarin cuz its profitable. Also Bactrim is just a tool to make u dependent on blood transfusions. The government owns the labs. Check the patents. 🤔
Kshitij Shah
December 2, 2025 at 10:35
So let me get this straight - you’re telling me that in 2024, we’re still having this conversation because doctors don’t read the damn guidelines? I mean, this isn’t even a debate. It’s a textbook case. Why are we still losing people to this? 😒
Dennis Jesuyon Balogun
December 2, 2025 at 14:03
The pharmacokinetic synergy between TMP-SMX and warfarin is not merely additive - it’s multiplicative. The inhibition of CYP2C9, coupled with albumin displacement and gut microbiota depletion, creates a tripartite pharmacodynamic cascade that exponentially increases free warfarin concentration. This is not a drug interaction - it’s a biochemical ambush. We must implement mandatory electronic health record alerts for this combination. The current system is lethally negligent.
Grant Hurley
December 4, 2025 at 00:18
my grandma was on warfarin and got Bactrim for a UTI and her INR went nuts. she was fine after they gave her vitamin k but man, i didnt know this could happen so fast. always check with your doc. dont assume. i learned the hard way.
Lucinda Bresnehan
December 5, 2025 at 08:11
Just wanted to add - if you're on warfarin and your doc prescribes Bactrim, ask them if they’ve ever had a patient with an INR spike from it. If they say no, ask again. If they still say no, get a second opinion. I’ve seen too many nurses get yelled at for asking this. You’re not being difficult - you’re being smart.
Shannon Gabrielle
December 6, 2025 at 01:31
Of course the FDA says it’s dangerous. They only care when people die. Meanwhile, the same people who wrote this post are probably on Medicare and still take 10 pills a day. Wake up. The system is rigged. Trust no one.
Nnaemeka Kingsley
December 7, 2025 at 11:21
bro i had this happen to my uncle. he was 81, on warfarin for AFib, got Bactrim for a bladder infection. next thing you know, he’s in the hospital with blood in his pee. doc said he was lucky. now he only takes amoxicillin. i printed out a list of safe antibiotics and taped it to his fridge. simple stuff saves lives.
Linda Migdal
December 9, 2025 at 07:10
It’s not even about the science anymore. It’s about accountability. If your doctor prescribes TMP-SMX to a warfarin patient without checking INR first, they’re not just careless - they’re endangering lives. We need mandatory reporting for these incidents. No more excuses.
Tommy Walton
December 10, 2025 at 09:53
So… you’re saying we need to *rethink* the very architecture of pharmacovigilance? 🤯 The CYP2C9 pathway is a metaphysical trap. We’re all just quantum particles in a pharmaceutical lattice. Bactrim? Just a vector of existential risk. 🧠💊
James Steele
December 11, 2025 at 16:12
The clinical implications of this interaction are non-trivial. The pharmacodynamic synergy between sulfamethoxazole-induced protein displacement and trimethoprim-mediated hepatic inhibition constitutes a Class I drug-drug interaction per the Lexicomp classification system. Yet, we continue to see this prescribed in primary care without even a baseline INR. This is not negligence - it’s systemic incompetence.
Louise Girvan
December 13, 2025 at 07:41
They told me it was safe… I trusted them. My husband died because no one checked his INR after Bactrim. Now I’m the one screaming at every pharmacist. Don’t let this happen to your family. Ask. Demand. Fight. They don’t care until you make them care.