How to Read Medication Guides for Overdose Warnings and Antidotes
Every time you pick up a new prescription, you get a small paper insert-the medication guide. Most people glance at it, maybe skim the side effects, and toss it in the drawer. But if you’re taking medications that carry overdose risk-like opioids, benzodiazepines, or certain antidepressants-this guide could save your life. Knowing how to read it properly isn’t just helpful. It’s critical.
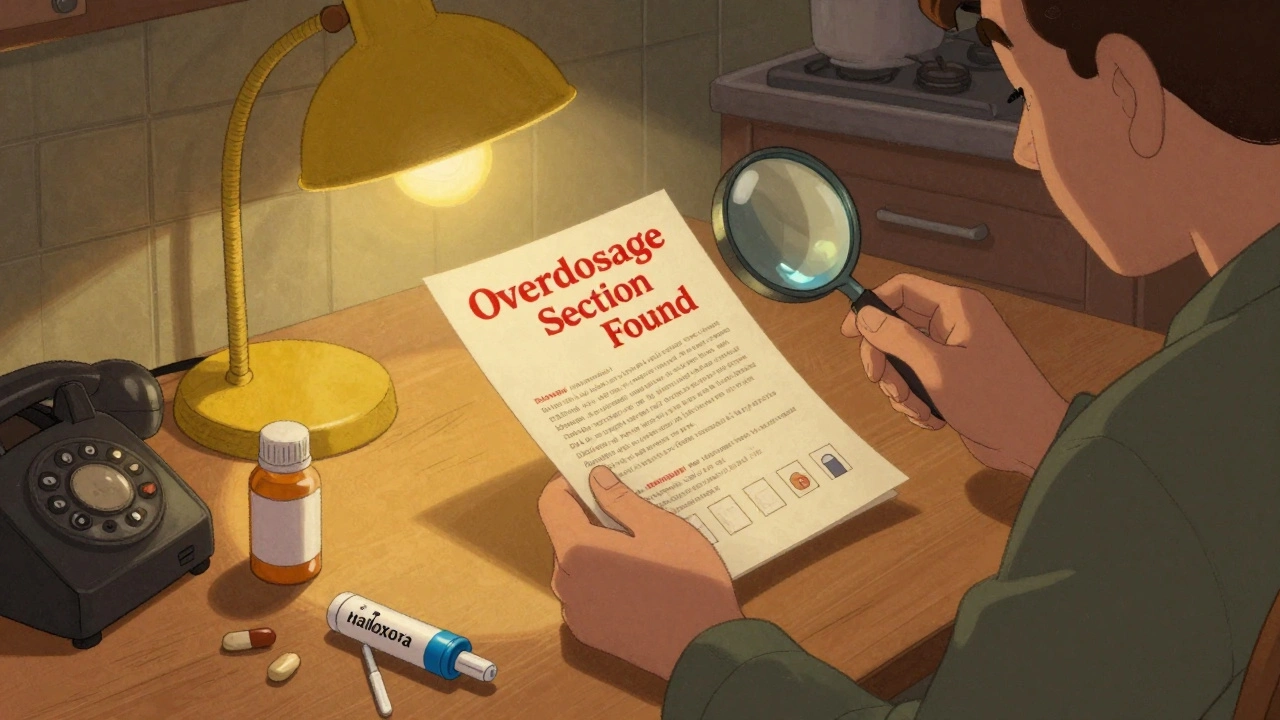
Where to Find the Overdose Section
The overdose information in your medication guide isn’t hidden. It’s required by the FDA to be clearly labeled. Look for the section titled Overdosage. It’s usually near the back, after Warnings and Precautions. This isn’t a vague warning like "take as directed." This section gives you exact details: how much is too much, what happens if you take too much, and what to do next.
For example, if you’re prescribed oxycodone, the Overdosage section will tell you that ingestion of 40 mg or greater of immediate-release oxycodone can be fatal in non-tolerant individuals. It won’t say "be careful." It’ll say exactly what the danger is. That’s the difference between a general warning and actionable data.
Understand the Boxed Warning
Before the Overdosage section, you’ll often see a black box with bold text. This is the FDA’s strongest warning-the Boxed Warning. If your medication has one, it means the risk is serious enough that the FDA requires it to be front and center. For opioid painkillers, this usually warns about respiratory depression, addiction, and overdose death.
Don’t skip this. The Boxed Warning tells you what the medication can do if misused. If it says "May cause fatal respiratory depression," that’s not a suggestion. It’s a fact. And if you’re taking more than one medication that depresses breathing-like sleeping pills, muscle relaxers, or alcohol-the risk multiplies. The Boxed Warning is your first red flag.
Find the Antidote Information
Not every medication has an antidote. But for opioids, benzodiazepines, and some other high-risk drugs, the Overdosage section will name the specific antidote. For opioids, it’s naloxone. For benzodiazepines, it’s flumazenil. These aren’t just names-they’re life-saving tools.
Look for phrases like: "Naloxone hydrochloride is a specific antidote for opioid overdose." Then check if it says how it’s given-intranasal, injectable, or auto-injector. Some guides even mention that naloxone may cause withdrawal symptoms like agitation or vomiting. That’s not a reason to avoid it. It’s a heads-up so you know what to expect after giving it.
Many pharmacies now offer naloxone without a prescription. If your medication guide mentions naloxone as an antidote, ask your pharmacist for a prescription or a free kit. Keep it in your purse, your car, or your medicine cabinet. It doesn’t expire quickly, and it’s safe to use even if you’re not sure an overdose is happening.

Know the Symptoms Listed
The Overdosage section will list symptoms of overdose. But don’t just read them. Memorize them. For opioids: slow or stopped breathing, extreme drowsiness, pinpoint pupils, cold/clammy skin, unresponsiveness. For benzodiazepines: confusion, slurred speech, loss of coordination, coma. For acetaminophen: nausea, vomiting, abdominal pain-then jaundice days later.
These symptoms don’t always come all at once. Overdose can start slowly. Someone might seem "just really sleepy" or "not themselves." If you’re taking a medication with overdose risk, tell someone close to you what these signs look like. Practice saying them out loud. When seconds count, you won’t have time to look up a list.
Check for Drug Interactions That Increase Risk
The Overdosage section doesn’t exist in a vacuum. It’s connected to the Warnings and Precautions section. Look for warnings about combining your medication with alcohol, other sedatives, or certain antidepressants. These interactions can turn a safe dose into a deadly one.
For example, mixing oxycodone with alprazolam (Xanax) increases overdose risk by up to 50%, according to CDC data. If your medication guide says "avoid concomitant use of CNS depressants," that includes alcohol, sleep aids, and anti-anxiety meds. Even over-the-counter cold medicines with diphenhydramine can be dangerous when combined with opioids.
Keep a list of everything you take-prescription, OTC, supplements. Bring it to every doctor visit. If your guide says "use with caution," don’t assume it’s safe. Ask your pharmacist: "Is this combination listed as dangerous in the Overdosage section?"

What If the Guide Doesn’t Mention an Antidote?
Not all drugs have a specific antidote. For antidepressants like SSRIs, there’s no direct reversal agent. For some pain meds, the antidote isn’t available outside a hospital. That doesn’t mean you’re safe. It means you need to be even more careful.
If your guide doesn’t name an antidote, focus on prevention: never take more than prescribed, never crush or snort pills, never mix with alcohol or other sedatives. Know the overdose signs. Have a plan. Call 911 immediately if you suspect an overdose-even if you’re unsure.
How to Use This Information in Real Life
Here’s what to do after reading your medication guide:
- Find the Overdosage section and read it out loud.
- Identify the antidote, if any, and ask your pharmacist for it.
- Write down the overdose symptoms and show them to a family member or roommate.
- Check the Warnings section for interactions you’re already using.
- Store the guide where you’ll see it-on your fridge, next to your pill organizer, taped to your bathroom mirror.
Don’t wait for an emergency to learn this. Practice now. If you’re caring for someone on high-risk medication, do this together. Make it part of your routine-like checking your smoke detector.
Why This Matters More Than Ever
In 2023, over 80,000 people in the U.S. died from drug overdoses. Many of those deaths involved prescription medications taken exactly as directed-but combined with other substances, or taken longer than recommended. The medication guide was there. But no one read it.
Reading it isn’t about being paranoid. It’s about being prepared. You wouldn’t drive a car without knowing where the brakes are. Don’t take a medication without knowing where the emergency stops are.
The FDA requires these guides for a reason. They’re not filler. They’re your safety manual. Treat them like one.
What should I do if I can’t find the Overdosage section in my medication guide?
If you can’t find an Overdosage section, the guide may be outdated or incomplete. Contact your pharmacist or the drug manufacturer directly. You can also look up the drug’s official prescribing information on the FDA website. Every FDA-approved medication must include this section-so if it’s missing, it’s an error that needs correction.
Can I rely on the label on the pill bottle instead of the medication guide?
No. The pill bottle label only tells you the name, dosage, and how often to take it. It doesn’t list overdose symptoms, antidotes, or drug interactions. The medication guide is the only document that contains full safety information. Always keep it.
Is naloxone safe to use even if I’m not sure someone is overdosing?
Yes. Naloxone only works on opioids. If someone isn’t overdosing on opioids, it won’t harm them. It won’t wake someone up if they’re just asleep. But if they’re overdosing, it can bring them back. It’s better to use it and be wrong than to wait and be too late.
Why do some medication guides say "call 911" and others say "administer naloxone first"?
Both are correct. Naloxone should be given immediately if available, but 911 must still be called. Naloxone wears off in 30 to 90 minutes, but opioids can stay in the system much longer. Someone can stop breathing again after the first dose. Emergency responders need to monitor them. So: give naloxone, then call 911. Don’t wait.
Do generic medications have the same overdose information as brand names?
Yes. Generic drugs contain the same active ingredient as brand names and are required by the FDA to have identical safety information, including overdose warnings and antidotes. The packaging may look different, but the guide’s content is legally required to match.




15 Comments
Steve Sullivan
December 8, 2025 at 20:24
I used to toss these guides in the drawer too... until my cousin OD'd on oxycodone and we didn't even know naloxone existed. Now I keep one in my glovebox. Life changes fast when you stop ignoring paperwork. 🙏
Simran Chettiar
December 9, 2025 at 22:58
It is truly remarkable how the human tendency to disregard critical information persists despite the overwhelming evidence of its importance, and one must consider the socio-cultural underpinnings of such negligence, especially in societies where medical literacy is not prioritized in public education systems, which leads to preventable tragedies that could be mitigated through simple, systematic engagement with pharmaceutical documentation.
Anna Roh
December 10, 2025 at 19:46
Meh. I just trust my doctor.
Richard Eite
December 12, 2025 at 05:55
America needs to stop being soft. If you can't read a damn insert, you deserve what you get. Naloxone isn't a babysitter
Katherine Chan
December 12, 2025 at 22:36
This is the kind of info that actually saves lives. I printed this out and taped it to my fridge next to my meds. My roommate now knows what to look for if I ever pass out. Small steps, big impact 💪
Philippa Barraclough
December 12, 2025 at 23:40
I find it curious that while the FDA mandates these guides, there is no standardized format across manufacturers. The placement of the Overdosage section varies significantly between brands, which may contribute to the confusion and oversight you describe. One might reasonably argue that a uniform structure would enhance comprehension and retention among the general public.
Tim Tinh
December 13, 2025 at 21:40
Just got my new script for gabapentin and read the guide for the first time. Turns out mixing it with alcohol can mess with your breathing. I had no idea. Told my buddy who drinks with me. He's gonna lay off now. Thanks for the nudge, this stuff matters.
Olivia Portier
December 14, 2025 at 12:16
I teach nursing students and I make them read these guides aloud in class. One girl cried because she realized her grandma died from a combo she didn't know was dangerous. We don't talk about this enough. Sharing this info isn't fear-mongering. It's love.
Tiffany Sowby
December 16, 2025 at 12:12
Why does the government even bother with these? People like me just want to feel better. If I have to read a novel every time I get a pill, I'll just stop taking them. It's not my job to be a pharmacist.
Asset Finance Komrade
December 16, 2025 at 13:37
The entire premise assumes Western medical authority is infallible. In many cultures, pharmacological reliance is seen as a symptom of systemic failure. Perhaps the real issue isn't that people don't read the guides, but that they distrust the system that gives them.
Jennifer Blandford
December 18, 2025 at 08:11
I used to think this was boring until my sister almost died from mixing her Zoloft with a cold med. She was fine, but I still have nightmares. Now I keep the guide on my phone as a screenshot. You never know when it'll be the thing that saves you. 🫂
Brianna Black
December 18, 2025 at 19:09
The Boxed Warning is not a suggestion. It is a death sentence waiting to be ignored. I have seen too many people treat these like fine print on a warranty. It is not. It is a declaration of danger. Treat it like the last warning before the abyss.
Shubham Mathur
December 20, 2025 at 09:09
I showed this to my dad hesitantly he's 72 and on 5 meds he said I never knew this stuff was in there I thought the bottle was enough now he carries his guide in his wallet
Stacy Tolbert
December 21, 2025 at 09:41
I read this and felt guilty. I didn't read my own guide for months. I'm scared to now. What if I find out I've been doing it wrong? What if it's too late?
Ronald Ezamaru
December 22, 2025 at 22:44
You're not alone. I felt the same way. But the guide isn't there to scare you. It's there to empower you. I read mine last week. Found out my muscle relaxer interacts with my tea. Changed my routine. No panic. Just awareness. That's all it takes.