Menopause and Hormone Therapy: What You Need to Know About Benefits and Risks
Hot flashes that wreck your sleep. Night sweats that soak your sheets. Mood swings that leave you feeling like you’re on an emotional rollercoaster. If you’re going through menopause, you know these aren’t just inconveniences-they’re life disruptors. For decades, hormone therapy was the go-to fix. Then came the scare. The Women’s Health Initiative study in 2002 told women to stop. But the story didn’t end there. Today, the science has evolved, and so have the guidelines. The truth? Menopause hormone therapy isn’t good or bad-it’s right or wrong depending on when, how, and for whom you use it.
What Menopause Hormone Therapy Actually Does
Menopause hormone therapy (MHT), sometimes called hormone replacement therapy (HRT), replaces the estrogen your body stops making after your ovaries shut down. For women with a uterus, it’s paired with progestogen to protect the lining of the uterus from overgrowth, which can lead to cancer. This isn’t about reversing aging. It’s about managing symptoms and protecting bone health. Estrogen therapy works better than anything else for hot flashes and night sweats. Studies show it cuts hot flashes by 75% compared to a placebo. That’s not a small improvement-it’s life-changing. One woman on Reddit shared, “I went from 15-20 hot flashes a day to 2-3 within 10 days on a low-dose patch.” That’s not an outlier. It’s the norm for women who start therapy early and use the right dose. It also helps with vaginal dryness, which affects over half of postmenopausal women. Low-dose vaginal estrogen creams or rings can restore comfort without affecting the rest of your body. And for bone health, MHT is one of the few treatments proven to slow bone loss. A woman who stayed on HRT for eight years told her support group, “My DEXA scan showed stable bone density. My sister, who skipped it, broke her hip at 62.”The Real Risks-Not the Myths
The fear around hormone therapy came from one big study-the Women’s Health Initiative (WHI)-that made headlines in 2002. It said HRT increased breast cancer and heart disease risk. But here’s what the headlines didn’t tell you: most of the women in that study were in their 60s and 70s, long past menopause. They weren’t starting therapy because of hot flashes. They were trying to prevent heart disease and dementia. That’s not what MHT is for. The real risk picture looks different when you look at timing. If you’re under 60 or within 10 years of your last period, the benefits of MHT for symptom relief outweigh the risks. The Endocrine Society, NAMS, and ACOG all agree on this. But if you’re 70 and starting estrogen for the first time? The risks climb-especially for stroke and blood clots. Breast cancer risk? It depends on the type. Estrogen-only therapy (for women without a uterus) adds about 9 extra cases per 10,000 women per year. Estrogen plus progestogen? About 29 extra cases per 10,000 women per year. That sounds scary, but compare it to smoking, which increases breast cancer risk by 30-50%. The risk from MHT is small and rises with longer use. Most women take it for 3-5 years, not 10. Blood clots are another concern. Oral estrogen increases the risk of venous thromboembolism (VTE)-a dangerous clot in the leg or lung-by about 2-3 times compared to not taking it. But transdermal estrogen (patches or gels) doesn’t carry that same risk. It bypasses the liver, so it doesn’t trigger the same clotting response. If you have a history of clots, high blood pressure, or migraines with aura, transdermal is the safer bet.Oral vs. Patch vs. Gel: Which Formulation Matters
Not all hormone therapies are created equal. The way you take it changes everything. Oral estrogen (pills like Premarin or generic estradiol) goes through your liver first. That’s why it raises your risk of clots, stroke, and gallbladder disease. But it’s cheap-$15 to $30 a month for generics. Many women start here because it’s easy. Transdermal options-patches, gels, sprays-deliver estrogen through your skin. That means less liver stress. Studies show transdermal estrogen lowers stroke risk by 30% compared to pills. It also carries a 50% lower risk of blood clots. The downside? Patches can fall off. Gels can rub off on clothes. And they cost more-$50 to $100 a month, even with insurance. Vaginal estrogen is a whole different ballgame. It’s used for dryness and discomfort during sex. It doesn’t enter your bloodstream in significant amounts, so it doesn’t affect your breast or uterus. You can use it long-term without worrying about systemic risks. Progestogen matters too. Micronized progesterone (brand name Prometrium) is the preferred choice over medroxyprogesterone acetate (Provera). Why? Provera is linked to higher breast cancer risk and more mood side effects. Progesterone is better tolerated and safer.
Who Should Avoid Hormone Therapy Altogether
MHT isn’t for everyone. If you’ve had:- Estrogen-sensitive breast cancer
- Active blood clots or a history of deep vein thrombosis or pulmonary embolism
- Undiagnosed abnormal vaginal bleeding
- History of stroke or heart attack
- Severe liver disease
What Works When Hormones Aren’t an Option
Not everyone can or wants to take hormones. That’s okay. There are alternatives, though they’re not as powerful. SSRIs like paroxetine (Brisdelle) are FDA-approved for hot flashes. They reduce symptoms by about 50-60%. Not as good as estrogen, but better than nothing. Gabapentin helps too-about 45% reduction-but it causes dizziness in a quarter of users. That’s a dealbreaker for some. Plant-based options like soy isoflavones or black cohosh? The evidence is weak. A Cochrane Review found they reduce hot flashes by only half a day compared to placebo. That’s barely noticeable. They’re not dangerous, but don’t expect miracles. Lifestyle changes help more than people think. Cooling your bedroom, wearing layers, cutting back on alcohol and caffeine, and doing regular aerobic exercise can cut hot flashes by 20-30%. One woman in Austin told me, “I started walking 30 minutes a day and cut out wine at night. My night sweats dropped by half. I didn’t need pills.”When to Start-and When to Stop
Timing is everything. The “window of opportunity” isn’t a myth-it’s science. Starting MHT within 10 years of your last period, or before age 60, gives you the best balance of benefit and safety. That’s when your blood vessels are still responsive to estrogen. After that, the risks creep up. A 2025 study of 120 million patient records found that women who started estrogen during perimenopause had 18% fewer heart events than those who waited until after menopause. That’s huge. As for stopping? There’s no hard deadline. Many women stay on it for 5-7 years until symptoms fade. Others need it longer for bone protection. The key is to reassess every year. Can you lower the dose? Can you switch from pills to a patch? Can you try going off for a few months to see if your hot flashes have calmed down?How to Get Started the Right Way
Don’t just pick up a prescription from your OB-GYN without a full discussion. Here’s what you need:- Track your symptoms for a month. Use a journal or app. How many hot flashes? How bad are the sleep disruptions?
- Get your blood pressure checked. High BP increases stroke risk with oral estrogen.
- Review your personal and family history. Any breast cancer? Blood clots? Liver disease?
- Ask about transdermal estrogen first. It’s safer for most women.
- Start low. Try 0.5 mg of oral estradiol or a 0.025 mg patch. You can always increase.
- Expect some spotting in the first 3-6 months. That’s normal as your uterus adjusts.
The Bigger Picture: Why This Matters Now
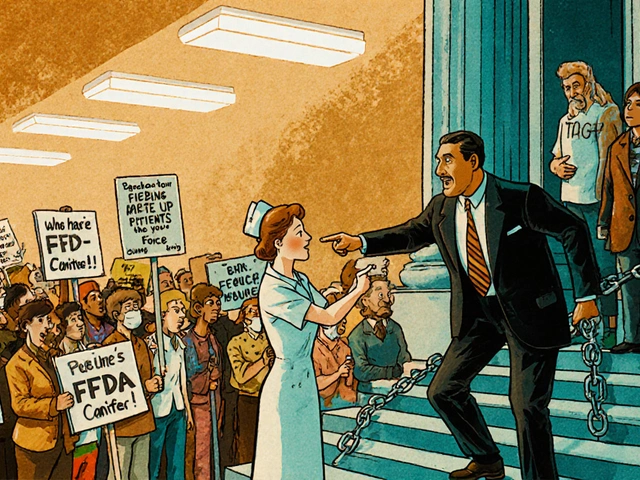
The market for hormone therapy is growing again. After a 70% drop post-2002, usage in the U.S. has climbed from 4% of menopausal women in 2013 to 15-20% today. Why? Because women are demanding better care. And science is finally catching up. New formulations like Duavee (a mix of estrogen and a bone-protecting drug) are making it easier to protect bones without raising breast cancer risk. Companies are starting to offer menopause support in the workplace-42% of Fortune 500 companies now do, according to a 2024 survey. The FDA just opened a public comment period in July 2025 to update guidelines based on new data. The message is clear: we’re moving away from blanket warnings and toward personalized care. Your age, your symptoms, your risk factors, your preferences-they all matter.Final Thoughts: It’s Not All or Nothing
Menopause isn’t a disease. But it’s not just “getting older” either. It’s a biological shift that can seriously impact your quality of life. Hormone therapy isn’t a cure-all. But for many women, it’s the most effective tool we have. The key is to stop seeing it as risky or safe. See it as a tool. Like a car. You wouldn’t drive a sports car in a snowstorm. You wouldn’t use a pickup truck to race on a track. You choose based on the conditions. If you’re under 60, have severe hot flashes, no history of cancer or clots, and want to feel like yourself again-MHT might be the right choice. Start low, go slow, use the safest delivery method, and recheck with your doctor every year. If you’re over 60, or you’re scared of breast cancer, or you just don’t want hormones-there are other ways. Lifestyle changes, non-hormonal meds, and support groups can help too. You don’t have to suffer. And you don’t have to take hormones. But you do need to know your options-and make a decision based on your body, your life, and your goals-not fear.Is hormone therapy safe for menopause?
For healthy women under 60 or within 10 years of menopause, hormone therapy is generally safe and effective for managing symptoms like hot flashes and night sweats. The risks-like blood clots and breast cancer-are small when using the lowest effective dose, especially with transdermal estrogen. But it’s not safe for women with a history of breast cancer, blood clots, stroke, or liver disease.
Does hormone therapy cause breast cancer?
Estrogen plus progestogen therapy slightly increases breast cancer risk-about 29 extra cases per 10,000 women per year. Estrogen-only therapy (for women without a uterus) adds only about 9 extra cases. The risk rises with longer use, but most women take it for 3-5 years. The absolute risk remains low compared to other factors like obesity or alcohol use.
What’s the safest form of hormone therapy?
Transdermal estrogen (patches or gels) is the safest option for women concerned about blood clots or stroke. It doesn’t pass through the liver, so it doesn’t increase clotting risk like oral pills do. Micronized progesterone is also safer than synthetic progestins like medroxyprogesterone acetate.
Can I take hormone therapy after age 60?
It’s not recommended for women starting hormone therapy after age 60 or more than 10 years past menopause. The risks of stroke, heart disease, and blood clots increase significantly with age. If you’re over 60 and still have severe symptoms, talk to your doctor about non-hormonal options or very low-dose transdermal therapy on a case-by-case basis.
How long should I stay on hormone therapy?
There’s no set time limit. Most women take it for 3-7 years until symptoms improve. Some need it longer for bone protection. The goal is to use the lowest dose for the shortest time needed. Reassess every year-can you lower the dose? Try going off for a few months? Your needs change over time.
Are there natural alternatives to hormone therapy?
Yes, but they’re less effective. SSRIs like paroxetine reduce hot flashes by about half. Gabapentin helps too, but causes dizziness. Lifestyle changes-cooling your room, avoiding caffeine, exercising-can cut symptoms by 20-30%. Plant-based options like soy or black cohosh have weak evidence and usually don’t work much better than placebo.






8 Comments
Alex Ronald
December 29, 2025 at 00:54
Just wanted to say this is one of the clearest breakdowns of MHT I’ve seen in years. The distinction between transdermal vs oral is critical, and most docs still push pills because they’re cheaper. I’ve had patients on patches for 8+ years with zero clots and stable bone density-no drama, just relief. If you’re under 60 and symptomatic, don’t let fear from 2002 stop you. Science moved on.
Sharleen Luciano
December 30, 2025 at 19:45
Let’s be honest-most women who take HRT are just chasing youth, not managing symptoms. The data shows a marginal benefit for hot flashes, but the long-term oncological risks are still underreported. And don’t get me started on the wellness influencers pushing ‘bio-identical’ hormones like they’re magic potions. If you’re not seeing a certified menopause specialist, you’re gambling with your health. This isn’t yoga and turmeric tea territory.
Aliza Efraimov
January 1, 2026 at 00:17
I was on oral estrogen for 4 years after my surgery at 48. Spotting for six months? Normal. Night sweats gone by week two? Life-changing. But I switched to a patch after my sister had a DVT on pills. My doctor didn’t even mention transdermal as an option until I asked. Why is this still not standard advice? Also-micronized progesterone saved my mental health. Provera made me weep uncontrollably for three weeks. Don’t let your provider push the cheap stuff. You deserve better.
Nisha Marwaha
January 2, 2026 at 21:57
From a global health equity perspective, the cost differential between transdermal and oral formulations represents a significant access barrier, particularly in low-resource settings. While transdermal estrogen demonstrates superior safety profiles in high-income cohorts, the majority of menopausal women globally rely on oral formulations due to systemic healthcare inequities. We must advocate for policy-level interventions to subsidize safer delivery mechanisms, not just individual patient education. The burden of risk stratification should not fall solely on the patient.
David Chase
January 3, 2026 at 20:57
STOP. JUST STOP. This article is a Big Pharma puppet show. Estrogen is a carcinogen. Period. They got away with lying about the WHI data and now they’re back peddling it like it’s ‘personalized medicine’? 😡 You think your ‘low dose’ patch is safe? You’re still flooding your system with synthetic hormones. And don’t even get me started on how they’re pushing this on women in their 50s like it’s a vitamin. 🇺🇸 WE’RE NOT LAB RATS FOR THE PHARMA INDUSTRY. #NoHRT #WomenRise
Paige Shipe
January 3, 2026 at 21:20
Actually, the data is very clear. The 2002 WHI study was flawed because it included women who were already old and unhealthy. But the FDA still uses it to scare women. I’ve read every single paper on this. The real risk of breast cancer from estrogen plus progestin is 0.29% per year. That’s less than the risk from drinking one glass of wine daily. And yet, doctors still act like you’re going to die if you take it. Pathetic.
Teresa Rodriguez leon
January 5, 2026 at 00:15
I started HRT at 51 because I was crying in the shower every day. I felt like a ghost in my own body. The first week on the patch? I slept through the night for the first time in two years. I didn’t cry. I didn’t rage. I just… breathed. I’m not ‘chasing youth.’ I’m reclaiming my sanity. And if you think that’s not worth it, you’ve never lived through it.
Tamar Dunlop
January 6, 2026 at 00:23
While the scientific consensus has indeed evolved, the cultural stigma surrounding menopause remains deeply entrenched, particularly within patriarchal healthcare frameworks. The normalization of suffering as an inevitable facet of aging continues to impede optimal patient care. It is imperative that medical education be restructured to prioritize menopausal health as a core competency-not an afterthought. Furthermore, workplace accommodations must be institutionalized, as the economic burden of untreated symptoms disproportionately impacts women’s professional longevity. This is not merely a medical issue; it is a human rights matter.