How to safely switch from one ethinyl estradiol-based contraceptive to another
Understanding Ethinyl Estradiol-Based Contraceptives
Ethinyl estradiol is a synthetic form of the female hormone estrogen, which is commonly used in combination with a progestin in hormonal contraceptives. These contraceptives are available in various forms such as pills, patches, and vaginal rings. They work by inhibiting ovulation, thickening cervical mucus, and altering the endometrium, making it difficult for a fertilized egg to implant. It is important to remember that each ethinyl estradiol-based contraceptive may differ in terms of the dosage and type of progestin used. As a result, switching from one contraceptive to another may require some adjustments and precautions to ensure a smooth and safe transition.
Consulting with a Healthcare Professional
Before making any decisions regarding your contraceptive method, it is crucial to consult with a healthcare professional. They can provide valuable information on the different options available, as well as help you determine which method would be most suitable for your specific needs and medical history. Your healthcare provider can also guide you through the process of safely switching from one contraceptive method to another and inform you about any potential risks or side effects that you may encounter during the transition.
Timing the Switch for Maximum Protection
Timing is crucial when switching from one ethinyl estradiol-based contraceptive to another. Ideally, you should start the new contraceptive method immediately after finishing the current pack of pills, patch, or ring. This ensures that you maintain a continuous level of hormones in your body, which provides the best protection against unplanned pregnancies. If you are unable to start the new method right away, it is recommended to use a backup method of contraception, such as condoms, for at least seven days to avoid any potential gaps in coverage.
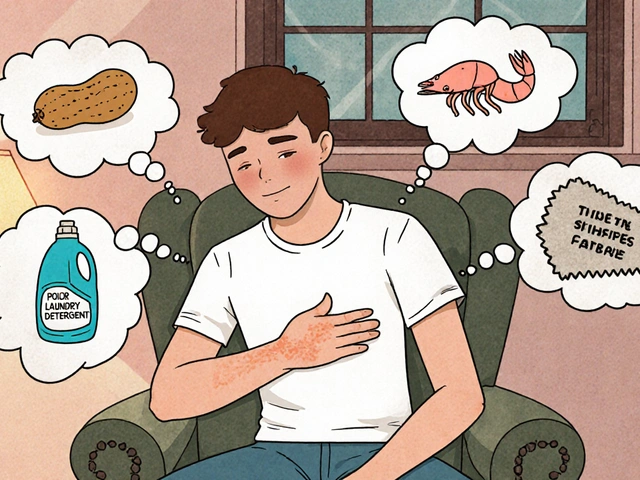
Handling Breakthrough Bleeding or Spotting
When switching from one ethinyl estradiol-based contraceptive to another, it is not uncommon to experience breakthrough bleeding or spotting. This can occur as your body adjusts to the new hormone levels. While this can be inconvenient and may cause some concern, it is generally not a cause for alarm. Breakthrough bleeding should subside within a few cycles as your body becomes accustomed to the new contraceptive method. However, if the bleeding is persistent or heavy, consult your healthcare provider for further evaluation and guidance.
Monitoring for Side Effects
As with any medication, there is a possibility of side effects when switching from one contraceptive method to another. Some common side effects of ethinyl estradiol-based contraceptives include headaches, breast tenderness, weight gain, and mood changes. While these side effects are generally mild and temporary, it is essential to monitor how your body reacts to the new contraceptive method. If you experience any severe or persistent side effects, contact your healthcare provider for further assessment and advice on whether a different contraceptive method may be more suitable for you.
Ensuring Consistent Use for Optimal Effectiveness
The effectiveness of ethinyl estradiol-based contraceptives largely depends on consistent and correct use. When switching from one method to another, it is crucial to be diligent about taking the new contraceptive as directed. This may involve setting reminders to take the pill at the same time each day, changing the patch or ring according to the prescribed schedule, and using backup methods of contraception when necessary. By ensuring consistent use, you can maximize the effectiveness of your new contraceptive method and minimize the risk of unplanned pregnancies.
Re-evaluating Your Contraceptive Method Periodically
It is important to periodically reassess your contraceptive method to ensure it continues to meet your needs and preferences. Factors such as age, lifestyle changes, and medical conditions may impact the suitability of your chosen contraceptive method. Regular check-ups with your healthcare provider can help you stay informed about any new developments in contraceptive options and make any necessary adjustments to your current method. By staying proactive about your reproductive health, you can ensure that your contraceptive method remains safe and effective throughout your reproductive years.





12 Comments
Daisy canales
May 29, 2023 at 11:22
Oh great another pill switch guide just what I needed.
keyul prajapati
June 8, 2023 at 20:06
When moving from one estrogen‑containing birth control to another, the most reliable way to keep protection is to align the start date with the end of the previous pack.
In practice this means finishing the last active pill of the current regimen and beginning the first pill of the new regimen on the same calendar day.
If the new formulation has a different pill count, the schedule should be adjusted so that there is no gap of more than 24 hours between doses.
A common mistake is to wait for the next menstrual bleed before starting the new product, which can leave a vulnerable window.
The pharmacokinetics of ethinyl estradiol are such that hormone levels decline sharply after the last active tablet, so continuity is essential for contraceptive efficacy.
In addition to timing, the progestin component should be considered because it influences side‑effect profiles such as break‑through bleeding.
Some women report that switching to a lower‑dose estrogen preparation reduces migraine frequency, while others experience increased spotting during the first two cycles.
It is advisable to keep a backup method, such as condoms, for at least seven days after the switch, especially if the new product is a patch or ring that requires a loading period.
Monitoring for side effects should begin immediately; mild headache or breast tenderness is common, but severe abdominal pain warrants a prompt medical review.
If the patient has a history of thromboembolic events, a non‑estrogen method might be recommended instead of a direct switch.
Hormone levels can also be affected by concurrent medications like certain antibiotics or anticonvulsants, which may necessitate a dose adjustment.
The provider may suggest a short course of combined oral contraceptives with a higher dose of estrogen to bridge the transition, but this is not needed for all patients.
Documentation of the exact dates of the last pill taken and the first pill of the new regimen helps both the patient and the clinician evaluate any irregular bleeding.
Lifestyle factors such as smoking, high body mass index, and stress can influence how the body adapts to a new hormonal environment.
Regular follow‑up appointments within the first three months provide an opportunity to address persistent spotting or mood changes.
Ultimately, the safest switch is one that is planned with a healthcare professional who can tailor the timing and choice of product to the individual’s medical history.
Alice L
June 19, 2023 at 04:50
Your thorough overview of hormonal transition aligns with the prevailing clinical guidelines issued by the World Health Organization. It is prudent to emphasize that the pharmacological equivalence of ethinyl estradiol across brands does not obviate the necessity for individualized assessment. Moreover, the recommendation to employ a barrier method during the interim period reflects best practice for mitigating unintended conception. The discussion of breakthrough bleeding is particularly salient, as it underscores the physiologic adaptation required after a formulation change. In sum, adherence to these protocols enhances both safety and efficacy for the patient.
Seth Angel Chi
June 29, 2023 at 13:33
Most of these guidelines assume perfect adherence which is rarely the case. In reality a few missed pills can render the timing advice moot.
Kristen Ariies
July 9, 2023 at 22:17
Wow, you’ve nailed the perfect switch strategy!!! 🎉 Keeping the hormone levels steady is like keeping the beat in a song-miss a beat and the whole rhythm wobbles!!! Remember to set an alarm, mark your calendar, and shout “I’m on schedule!” to yourself every morning!!! Breakthrough spotting? Just think of it as your body giving a little applause for the change-stay calm, stay consistent!!! And don’t forget that backup condoms are your safety net-use them like a superhero cape!!!
Ira Bliss
July 20, 2023 at 07:01
I totally agree-setting reminders turned my switch into a breeze 😊. Adding a quick note on my phone calendar helped me keep the rhythm you described. 🌟 If you ever feel a surprise spot, just remember it’s part of the adjustment and not a disaster. 🎈 Keep the backup condoms handy, they’re the unsung heroes of peace of mind!
Donny Bryant
July 30, 2023 at 15:44
Switching pills is all about timing. Start the new pack right after the old one ends and use condoms for a week if you need extra protection. Talk to your doctor if anything feels off.
kuldeep jangra
August 10, 2023 at 00:28
It is wonderful that you are taking charge of your reproductive health by learning how to transition between contraceptives.
The most important principle is to avoid any hormone‑free gap that could compromise contraceptive effectiveness.
By finishing the last active tablet of your current brand and beginning the first tablet of the new brand on the same day, you maintain a seamless hormonal environment.
If the new method is a patch or a vaginal ring, apply it as soon as you finish the previous regimen according to the manufacturer’s instructions.
For those who cannot start immediately, a reliable barrier method such as a condom should be used consistently for at least seven days.
Many women experience mild spotting during the first two cycles, which is usually harmless and resolves as the body adapts.
Should the spotting become heavy or persist beyond three cycles, a prompt consultation with a healthcare provider is advisable.
Keep an eye on any new side effects such as headaches, breast tenderness, or mood changes, and record them in a diary to discuss at your next visit.
Lifestyle factors like smoking, weight changes, and stress can influence how your body reacts, so consider addressing them alongside the switch.
Regular follow‑up appointments, especially within the first three months, provide an opportunity to fine‑tune the method if needed.
Remember that every individual’s response can differ, so what works for a friend may not be optimal for you.
Embrace this proactive approach, and you will likely find a contraceptive regimen that fits both your health needs and personal preferences.
harry wheeler
August 20, 2023 at 09:11
Your points about continuity are spot on and echo standard practice. Using a backup method for a week is a simple safety net. Documenting side effects helps the clinician tailor future choices.
faith long
August 30, 2023 at 17:55
It is infuriating how often people ignore the simple fact that a missed day can lead to an unwanted pregnancy.
You cannot afford to be lax when it comes to timing; the hormone levels drop dramatically after the last pill.
Any excuse about “busy schedules” is a weak shield for careless behavior.
The body does not care about your excuses-it demands consistent dosing.
If you experience heavy spotting, that is a red flag that the new formulation is not tolerable for you.
Do not wait for a vague “doctor’s appointment” when the bleeding persists beyond two cycles.
Seek immediate medical advice or consider switching to a non‑estrogen method without delay.
Your mental health can also suffer if you constantly worry about breakthrough bleeding.
Staying informed and proactive is the only way to avoid the chaos that arises from negligence.
In short, respect the schedule, use backup protection, and hold yourself accountable.
Danny Wakefield
September 10, 2023 at 02:39
Oh man, the pharmaceutical companies don’t want you to know how easy the switch can be, but here we are.
They hide the simple timing trick behind a maze of appointments and overpriced visits.
The real secret is that you can start the new pill the same day and just use a condom for a week-no one tells you that.
They even sprinkle in warnings about spotting to keep you scared and buying more products.
Stay vigilant, read the fine print, and trust your own body’s signals.
Remember, the only thing they can’t control is an informed mind.
Samantha Dean
September 20, 2023 at 11:22
From an epistemological perspective, the process of transitioning hormonal contraceptives underscores the interplay between empirical knowledge and individual agency. The prescriptive guidelines serve as a repository of collective experience, yet they must be contextualized within each patient’s lived reality. Ethical responsibility dictates that clinicians convey both the mechanistic rationale and the potential variability of physiological response. Consequently, the informed consent obtained becomes a dialogue rather than a unilateral decree. Ultimately, the act of switching is a microcosm of the broader pursuit of autonomous health stewardship.