Metabolic Surgery Outcomes: Real-World Weight Loss and Diabetes Remission Rates
When someone with type 2 diabetes and obesity hears the word surgery, their first thought isn’t usually relief-it’s fear. But for many, metabolic surgery isn’t about cutting away fat. It’s about resetting the body’s broken metabolism. And the data doesn’t lie: for people struggling with diabetes that won’t respond to pills or diet, this surgery can change everything.
What Metabolic Surgery Actually Does
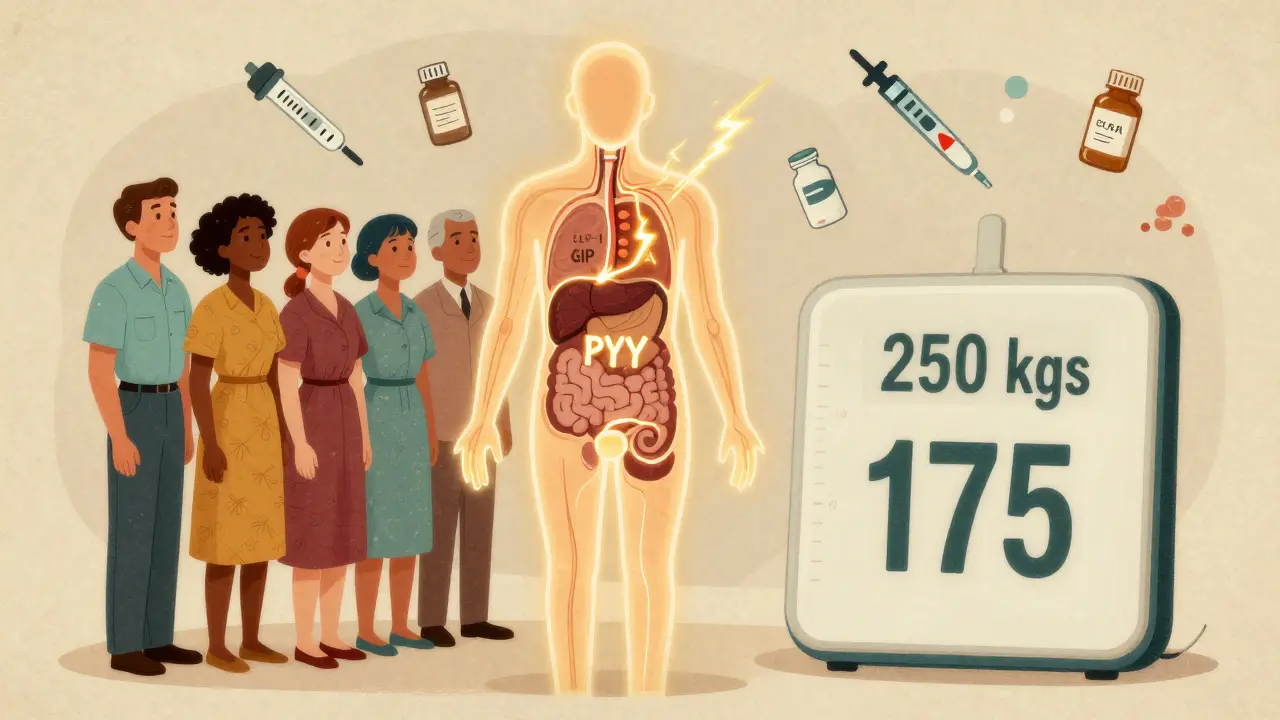
Metabolic surgery, often called bariatric surgery, isn’t just about shrinking your stomach. It’s a group of procedures that change how food moves through your digestive system. The most common types are gastric bypass, sleeve gastrectomy, and duodenal switch. Each one alters hormone signals, gut bacteria, and nutrient absorption-not just calorie intake. The big surprise? Diabetes often starts improving within days after surgery, long before you’ve lost much weight. That’s because these procedures trigger a cascade of hormonal changes. GLP-1, GIP, and PYY-hormones made in your intestines-start flooding your bloodstream. These hormones tell your pancreas to make more insulin, reduce liver sugar production, and make you feel full faster. It’s not just weight loss. It’s a metabolic reboot.How Much Weight Do People Actually Lose?
Numbers matter here. In a major 2024 study published in JAMA, patients who had gastric bypass lost an average of 19.9% of their total body weight over six years. Those who stuck with diet and medication? Just 8.3%. That’s more than double the loss. Across all types of metabolic surgery, patients typically lose 25-30% of their starting weight. For someone weighing 250 pounds, that’s 60-75 pounds gone. And it’s not just a short-term drop. Studies tracking patients for over 10 years show most keep off the majority of that weight. That’s something no pill or diet program has ever achieved at this scale.Diabetes Remission: The Real Win
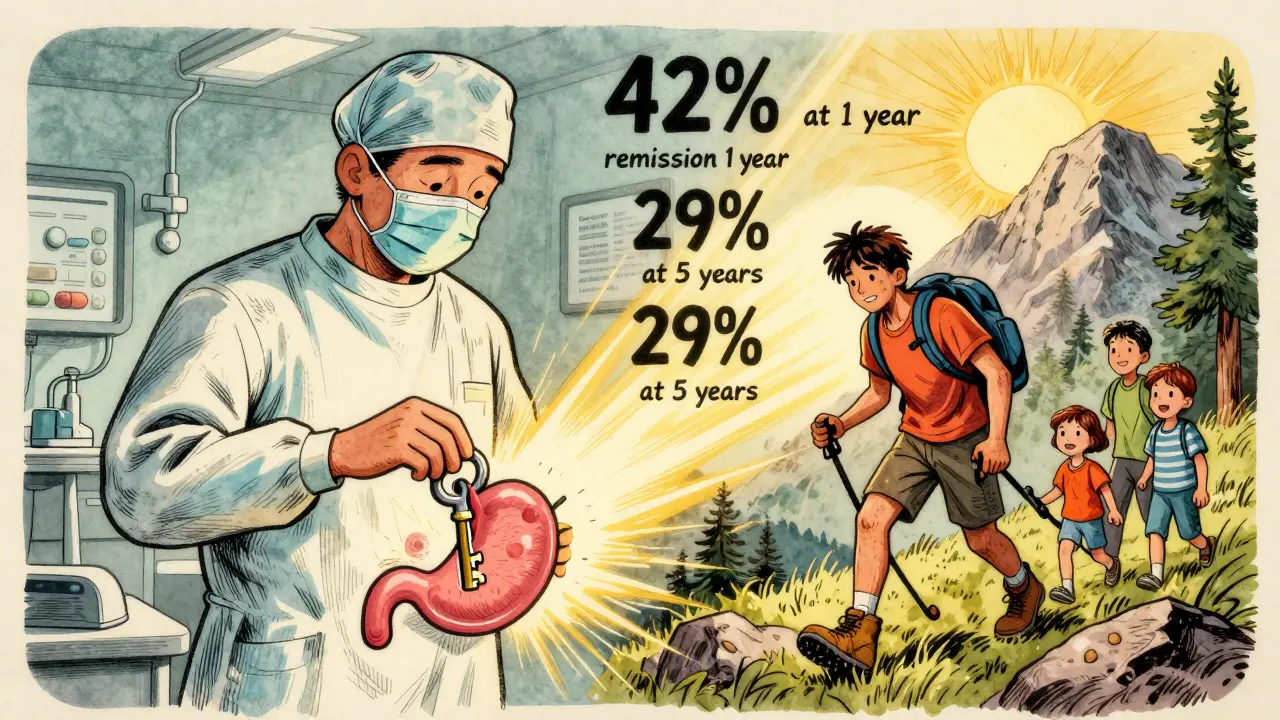
Weight loss is impressive. But for someone with type 2 diabetes, remission is the holy grail. Remission means your blood sugar stays normal without any diabetes meds-not just controlled, but gone. The Swedish Obese Subjects study, one of the longest-running trials ever, followed patients for 15 years. Of those who had surgery, 30.4% were in full diabetes remission. Only 6.5% of those treated with medication alone reached that point. That’s nearly five times higher. Gastric bypass leads the pack. One year after surgery, about 42% of patients no longer needed diabetes medication. At five years, that number was still at 29%. Sleeve gastrectomy, a less complex procedure, had 37% remission at one year and 23% at five. Even more striking: patients with a BMI under 35-considered only overweight, not obese-had a 93% remission rate after gastric bypass if they weren’t on insulin yet.Who Benefits the Most?
Not everyone responds the same. The best candidates have a few things in common:- They haven’t started insulin yet. Insulin users have lower remission rates-around 20-30%-because their pancreas is more damaged.
- They’ve had diabetes for less than 10 years. The longer you’ve had it, the harder it is to reverse.
- They’re younger, under 60. Age matters, but not as much as how long the disease has been active.
- They’re willing to stick with lifelong follow-up. Nutrition checks, blood tests, and supplements aren’t optional.
The Catch: It’s Not a Cure
Let’s be clear: metabolic surgery isn’t a magic bullet. Remission can fade. In the same Swedish study, remission dropped from 72% at two years to 36% at ten years. Why? Weight regain. Beta-cell exhaustion. Lifestyle drift. The body can slowly slip back into old patterns. But here’s the twist: even when full remission fades, most patients still do better than before surgery. Their blood sugar stays lower. They take fewer pills. Some stop insulin entirely. One study found that for every year of remission, the risk of kidney damage, nerve pain, and eye problems dropped by 19%. That’s not nothing. That’s decades of quality life.What About the Risks?
Surgery isn’t risk-free. The most common long-term issues are nutritional: iron and B12 deficiency leading to anemia, low calcium and vitamin D causing bone thinning, and occasional diarrhea or dumping syndrome. These aren’t rare. About 1 in 5 patients need ongoing supplements or IV treatments. Bone fractures are 30-50% more common in surgical patients over 10 years. That’s why follow-up care isn’t optional-it’s essential. You need regular blood tests, bone scans, and dietitian visits for life. And yes, there’s a learning curve for surgeons. Studies show outcomes improve dramatically after a team performs at least 100 procedures. If your surgeon has done fewer, ask why.Who Gets Access?
Despite strong evidence, less than 2% of eligible people in the U.S. get metabolic surgery each year. Why? Insurance. Most insurers only cover surgery if your BMI is 40 or higher, or 35 with another condition like diabetes. But research shows people with BMI 30-34.9 benefit too. The American Diabetes Association says surgery should be considered for these patients if their diabetes isn’t controlled. Yet many insurers still refuse. Even when approved, pre-approval can take months. You need proof you’ve tried diet, exercise, and medications for at least six months. You’ll need a psychological evaluation. It’s not easy-but it’s doable.The Bigger Picture: Surgery Isn’t the Only Option
Newer non-surgical tools are emerging. Intragastric balloons, endoscopic sleeve gastroplasty, and even the AspireAssist device (which drains part of your stomach after meals) offer middle-ground options. They’re less invasive but also less effective long-term. The DiRECT trial showed that a very low-calorie diet could lead to 46% diabetes remission at one year. But only 30% stayed in remission after two years. Surgery still wins on durability. The future? Trials like RESET are testing surgery in people with BMI as low as 27. That could open the door to millions more who currently don’t qualify.What Comes After Surgery?
You don’t walk out of the hospital cured. You walk out starting a new life. The first year is intense: protein intake matters. You can’t drink and eat at the same time. You’ll need vitamin B12 injections. Calcium and iron supplements are non-negotiable. Your doctor will monitor your blood every 3-6 months. But the rewards are real. People report more energy. Better sleep. Fewer doctor visits. The ability to walk without pain. To play with their kids without getting winded. To stop checking blood sugar five times a day. One patient, a 52-year-old teacher, lost 80 pounds after gastric bypass. Her A1C dropped from 9.2 to 5.4. She stopped all meds. She started hiking. She didn’t just lose weight. She got her life back.Final Thoughts: Is It Worth It?
Metabolic surgery isn’t for everyone. But for those with type 2 diabetes and obesity who’ve tried everything else, it’s the most powerful tool we have. It’s not about being ‘weak’ or ‘giving up.’ It’s about using science to fix a broken system. The body doesn’t respond to willpower alone. Sometimes, it needs a reset. The numbers don’t lie: better weight loss. Better blood sugar. Fewer complications. Longer life. And yes, even better sleep, more confidence, and more time with the people you love. It’s not easy. But for many, it’s the best shot they’ve ever had.Can metabolic surgery cure type 2 diabetes?
Metabolic surgery doesn’t guarantee a permanent cure, but it can lead to long-term remission-meaning normal blood sugar without medication. Studies show 30-40% of patients stay in remission for 10 years or more. Even when remission fades, most people still have better blood sugar control and need fewer drugs than before surgery.
Which surgery is best for diabetes remission?
Gastric bypass (RYGB) has the highest remission rates, especially in the first few years-up to 42% at one year and 29% at five. Biliopancreatic diversion with duodenal switch has even higher short-term remission (95%), but it carries greater nutritional risks. Sleeve gastrectomy is less complex and still effective, with about 37% remission at one year. The best choice depends on your BMI, health history, and willingness to manage long-term supplements.
Do I need to be severely obese to qualify?
Traditionally, yes-BMI 35 or higher with diabetes. But new guidelines from the American Diabetes Association and ongoing trials like RESET suggest surgery can benefit people with BMI as low as 30, especially if their diabetes is poorly controlled. Insurance often still denies coverage for these patients, but medical evidence supports it.
What if I’m already on insulin?
You can still benefit, but remission rates are lower-around 15-20% compared to 50%+ for those not on insulin. Insulin use often means your pancreas has lost much of its ability to produce insulin. Surgery can still improve blood sugar control and reduce your insulin dose, sometimes eliminating it entirely. But full remission is less likely.
What are the biggest long-term risks?
The biggest risks are nutritional: anemia from iron or B12 deficiency, low bone density leading to fractures, and gastrointestinal issues like dumping syndrome or chronic diarrhea. These aren’t rare-they affect up to 20% of patients. Lifelong blood tests, supplements, and follow-up care are mandatory. Skipping them can lead to serious health problems.
How long does recovery take?
Most people leave the hospital in 1-3 days. Return to light work takes 2-4 weeks. Heavy lifting and strenuous activity should wait 6-8 weeks. Blood sugar often improves within days. Weight loss is steady-1-2 pounds per week for the first year. Full adjustment to new eating habits takes 6-12 months.
Is metabolic surgery covered by insurance?
Most insurance plans cover surgery if your BMI is 40 or higher, or 35 with a condition like diabetes. Coverage for BMI 30-34.9 is inconsistent. You’ll need proof of failed medical therapy (6+ months of diet, exercise, and medications), psychological evaluation, and nutritional counseling. Denials are common, but appeals often succeed with strong medical documentation.
Can I gain the weight back after surgery?
Yes, about 15-20% of patients regain a significant amount of weight over 5-10 years. This is often linked to returning to high-calorie, high-sugar diets or skipping follow-up care. Weight regain doesn’t mean failure-it means you need to adjust your habits. Many patients still maintain better health than before surgery, even with some weight regain.






11 Comments
Rachel Liew
February 1, 2026 at 23:15
I know someone who had this surgery and it literally saved her life. She went from being bedridden to hiking mountains in a year. No magic, just science. And yeah, the supplements are a pain, but worth it.
Deep Rank
February 3, 2026 at 10:30
Look, I get why people are excited, but let’s be real-this isn’t a cure, it’s a band-aid with a side of lifelong vitamin hell. You think your body’s ‘resetting’? Nah. It’s just being forced into a new cage. And when you slip up? The guilt? Oh honey, it’s brutal. I’ve seen too many people crash after year 3 because they forgot how to eat. This isn’t empowerment-it’s a high-stakes gamble with your pancreas.
Naomi Walsh
February 4, 2026 at 07:09
It’s amusing how the article frames this as some revolutionary breakthrough. The hormonal cascade? GLP-1 agonists have been doing this for years-without cutting you open. The real issue isn’t the surgery-it’s that we’re still treating metabolic disease like a mechanical problem instead of a systemic one. Also, 30% remission? That’s barely better than placebo in the long run. The real win is the industry profit margin.
Bryan Coleman
February 4, 2026 at 10:24
Just chiming in as a nurse who’s seen this up close. The weight loss numbers are real, but the real MVP is the follow-up care. Patients who stick with dietitians and labs? They thrive. The ones who ghost their appointments? End up back in the ER with low iron and broken hips. It’s not the surgery that fails-it’s the system that drops the ball after the incision heals.
Naresh L
February 5, 2026 at 16:09
There’s something deeply poetic about using surgery to ‘reset’ a body that’s been betrayed by its own biology. We blame willpower, but the body doesn’t care about discipline-it responds to signals. This surgery doesn’t punish gluttony; it rewrites the language the gut speaks to the brain. Maybe we’re not broken. Maybe we’re just speaking the wrong dialect.
Sami Sahil
February 6, 2026 at 10:24
Y’all need to stop overthinking this. If you’re tired of being tired, of feeling like your body’s working against you-do the damn thing. Yeah, it’s scary. Yeah, you gotta take pills forever. But I lost 90 lbs and now I can chase my daughter without wheezing. That’s not a miracle. That’s just common sense with a scalpel.
franklin hillary
February 7, 2026 at 14:45
Let me be blunt-this isn’t surgery, it’s a biological hack. You’re not losing weight, you’re hacking your hormones like a programmer fixing a glitch. And yeah, the risks? Real. But so is dying from diabetic amputations at 45. If you’ve tried everything and your pancreas is crying, this is your reset button. No shame. No guilt. Just science. 💪🩺
Bob Cohen
February 7, 2026 at 18:20
Wow. So we’re now recommending major surgery because people can’t resist pizza? I mean, sure, it works. But is it really the answer? Or are we just outsourcing responsibility to a scalpel? Also, 2% of eligible people get it? That’s not a healthcare problem-that’s a capitalism problem. Insurance companies are playing Russian roulette with people’s kidneys.
Ishmael brown
February 9, 2026 at 01:11
So… you’re telling me cutting my stomach and taking vitamins for life is better than just… not eating donuts? 🤔💩
Nancy Nino
February 9, 2026 at 04:56
It is, of course, entirely predictable that the most effective intervention for metabolic disease remains inaccessible to the very populations most in need. The irony is not lost on those of us who have watched loved ones languish in the bureaucratic purgatory of insurance denials. One must wonder: if this were a pill, would it be so hard to obtain? Or is it the invasive nature of the procedure that renders it morally suspect in the eyes of those who profit from chronic disease?
Nidhi Rajpara
February 10, 2026 at 13:41
While the data presented is compelling, one must consider the longitudinal adherence rates to postoperative nutritional protocols. In India, where access to specialized dietitians and lab testing is limited outside urban centers, the long-term success of such interventions is statistically questionable. Moreover, the cultural emphasis on carbohydrate-rich diets may exacerbate nutrient deficiencies post-surgery, particularly in patients without adequate education or familial support systems. The clinical outcomes in Western cohorts may not be generalizable to low-resource settings without significant infrastructure investment.