The Connection Between a Burning Sensation and Multiple Sclerosis
Understanding Multiple Sclerosis and Burning Sensations
As someone who has been personally affected by multiple sclerosis (MS), I know firsthand how difficult it can be to navigate the many symptoms and side effects that come with this life-altering disease. One such symptom that many people with MS experience is a burning sensation. In this article, I will explore the connection between a burning sensation and multiple sclerosis, digging deeper into the causes, symptoms, and potential treatment options for those who suffer from this debilitating condition.
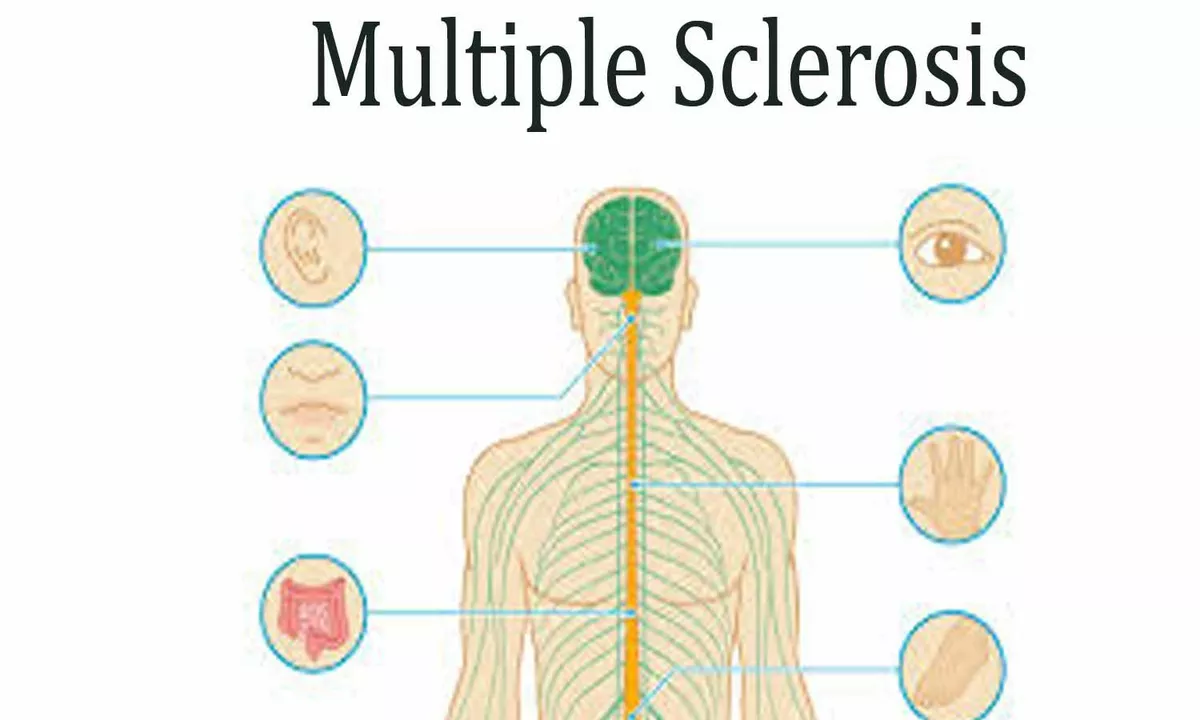
Exploring the Nervous System and MS
Before we can fully understand the connection between burning sensations and MS, we must first have a baseline understanding of the nervous system and how MS affects it. At its core, multiple sclerosis is an autoimmune disease that targets the central nervous system, which includes the brain and spinal cord. When the immune system attacks the protective layer around nerve fibers, known as myelin, it can cause a variety of symptoms, including burning sensations, numbness, and tingling.
The Science Behind Burning Sensations in MS
The burning sensation that many people with MS experience is known as dysesthesia. Dysesthesia is a type of altered sensation that can be painful, and it is caused by damage to the nerves in the central nervous system. When the nerves are damaged, they can send incorrect signals to the brain, which can manifest as a burning, itching, or tingling sensation. This can be extremely uncomfortable and can greatly affect a person's quality of life.
Identifying the Different Types of Burning Sensations
Not all burning sensations are created equal, and it's essential to know the different types that can occur in those with MS. There are two primary types of dysesthesia: thermal and mechanical. Thermal dysesthesia is characterized by a burning sensation that is triggered by changes in temperature, while mechanical dysesthesia is caused by touch or pressure. Both of these types of burning sensations can be incredibly disruptive to daily life, and it's crucial to identify which type you may be experiencing in order to seek appropriate treatment.
Managing and Treating Burning Sensations in MS
While there is currently no cure for multiple sclerosis, there are ways to manage and treat the various symptoms that come with the disease, including burning sensations. The first step in treating burning sensations in MS is to consult with a healthcare professional who can provide a proper diagnosis and recommend appropriate medications. Some potential treatment options include anticonvulsants, antidepressants, and pain-relief medications. In addition to medication, physical therapy and relaxation techniques can also help alleviate some of the discomfort associated with burning sensations in MS.
Alternative Therapies and Coping Strategies
In addition to traditional medical treatments, there are alternative therapies and coping strategies that may help alleviate burning sensations in those with MS. Some of these options include acupuncture, massage therapy, and mindfulness practices. While these methods may not work for everyone, they can provide additional relief for some people and can be a valuable part of a comprehensive treatment plan.
The Importance of a Support System
Living with multiple sclerosis and experiencing symptoms like burning sensations can be incredibly isolating and emotionally challenging. Building a strong support system is essential for maintaining mental and emotional well-being. Whether it's through friends, family, or a support group specifically for those with MS, connecting with others who understand your struggles can make a world of difference when it comes to managing your symptoms and maintaining a positive outlook.
Discussing Your Symptoms with Your Healthcare Team
It's crucial to keep an open dialogue with your healthcare team about the symptoms you're experiencing, including any burning sensations. This will allow them to better understand your specific needs and adjust your treatment plan accordingly. Be honest and thorough when discussing your symptoms, and don't be afraid to ask questions or seek clarification on any aspect of your care.
Staying Informed and Advocating for Your Health
As someone living with multiple sclerosis, it's essential to stay informed about the latest research and treatment options available. This will help you be an active participant in your healthcare journey and give you the tools you need to advocate for yourself and your well-being. Knowledge truly is power, and by staying up-to-date on the latest developments in MS research, you can help ensure that you receive the best possible care and support.
Conclusion
The connection between a burning sensation and multiple sclerosis is a complex and sometimes challenging aspect of living with this disease. By understanding the underlying causes, identifying the different types of burning sensations, and exploring various treatment options, you can better manage this symptom and improve your overall quality of life. Remember, you are not alone in this journey, and by connecting with others who understand your struggles, staying informed, and advocating for your health, you can face these challenges head-on and continue to live a fulfilling and meaningful life.




19 Comments
Puneet Kumar
May 13, 2023 at 19:46
Hey everyone, I wanted to add a bit of context to the discussion about burning sensations and MS. Dysesthesia, as mentioned, is a manifestation of central demyelination and neuroinflammation that can trigger thermal or mechanical pain pathways. In clinical practice we often see patients describing a “burning” quality that correlates with lesion location in the spinal cord or brainstem. Addressing this symptom usually involves a multimodal approach-pharmacologic agents like gabapentinoids, alongside physiotherapy and cognitive‑behavioral strategies. Remember, early intervention can improve quality of life, so keep the conversation going.
michael maynard
May 13, 2023 at 22:33
Look, the pharma giants don’t want you to know that most of these “miracle” meds are just a cash grab. They push gabapentin like it’s the holy grail while ignoring cheaper alternatives that actually work. And the “research” they cite is often funded by the same companies selling the drugs. It’s a sham that keeps us in the dark, feeding the industry’s profit machine.
Roger Bernat Escolà
May 13, 2023 at 23:56
Wow, that’s intense. I get the frustration, but burning sensations in MS are real and can be debilitating. Even if you’re skeptical, some patients do find relief with the prescribed meds, though outcomes vary widely.
Allison Metzner
May 14, 2023 at 01:20
It’s evident that the mainstream narrative is constructed by an elite consortium of neurologists and biotech lobbyists. Their discourse is deliberately obfuscating the true etiology of dysesthesia, steering us away from holistic modalities that could restore neuro‑immune balance.
william smith
May 14, 2023 at 02:43
For anyone looking for a quick start: talk to your neurologist about trialing a low‑dose gabapentin, monitor side effects, and pair it with daily stretching. That’s the most straightforward path.
Timothy Javins
May 14, 2023 at 04:06
Honestly, I think focusing on the burning sensation diverts attention from the bigger picture-MS progression itself. We should prioritize disease‑modifying therapies over symptomatic fixes.
Kay Yang
May 14, 2023 at 05:30
🤔 That’s a fair point, but symptom management is still crucial for day‑to‑day comfort. 😊
Rajesh Kumar Batham
May 14, 2023 at 06:53
From my experience, incorporating gentle yoga and mindfulness really helps calm the nerve firing that leads to that prickly, burning feeling. 🌿🧘♂️
Bill Gallagher
May 14, 2023 at 08:16
Indeed, the literature supports that integrative therapies can modulate neuroplasticity-particularly, yoga enhances parasympathetic tone, which reduces the frequency of ectopic discharges; mindfulness, on the other hand, recruits prefrontal cortical networks to re‑interpret nociceptive input, thereby diminishing the subjective intensity of dysesthesia; moreover, combining these approaches with proper pharmacologic titration yields a synergistic effect that is often overlooked in conventional treatment protocols; thus, a multidisciplinary regimen is not merely adjunctive but essential for comprehensive care.
Rajashree Varma
May 14, 2023 at 09:40
Stay hopeful, folks! Even with those burning sensations, many find that consistent self‑care and staying informed can turn the tide toward better days.
Anshuman Pandey
May 14, 2023 at 11:03
Think of each small improvement as a step on a ladder-climbing higher becomes easier when you believe in the ascent.
Thomas Malloy
May 14, 2023 at 12:26
That’s a solid tip.
Sushma Gowda
May 14, 2023 at 13:50
Remember, you’re not alone in this journey; lean on your support network and keep a symptom diary to track what works best for you.
Angie Wallace
May 14, 2023 at 15:13
Thanks for the reminder, really helpful.
Doris Montgomery
May 14, 2023 at 16:36
Honestly, this article feels like a rehash of the same old advice-nothing groundbreaking here.
Nick Gulliver
May 14, 2023 at 18:00
Well, some of us actually benefit from the basics; not everyone needs a revolutionary breakthrough to feel relief.
Sadie Viner
May 14, 2023 at 19:23
Dear community, I would like to formally acknowledge the complexity of dysesthetic pain in multiple sclerosis and suggest a structured protocol: first, confirm the diagnosis with quantitative sensory testing; second, initiate a low‑dose trial of a gabapentinoid while monitoring renal function; third, integrate a physiotherapy regimen focused on proprioceptive training; fourth, consider adjunctive low‑level laser therapy for localized burning; finally, schedule quarterly reviews to adjust the therapeutic plan. This systematic approach ensures both efficacy and safety.
Kristen Moss
May 14, 2023 at 20:46
Yo, the US healthcare system needs to stop over‑medicating folks and start letting them try natural stuff-power to the people!
Rachael Tanner
May 14, 2023 at 22:10
When we examine the phenomenon of burning sensations in multiple sclerosis, we must first appreciate the intricate pathophysiology of demyelination, which disrupts normal axonal conduction and leads to ectopic neuronal firing that patients describe as a “burn.” This aberrant signaling is not merely a peripheral inconvenience but a central nervous system mishap that reflects broader neuroinflammatory processes. Studies have shown that lesions located in the thalamic nuclei or spinal dorsal columns are particularly prone to generate dysesthetic pain, underscoring the importance of lesion mapping in clinical assessment. Pharmacologically, agents such as gabapentin and pregabalin act on the α2δ subunit of voltage‑gated calcium channels, dampening the hyperexcitability of damaged neurons. However, their efficacy is heterogeneous, and side‑effects like sedation or dizziness can compound the patient’s disability burden. Complementary interventions, including transcranial magnetic stimulation, have emerged as promising modalities that modulate cortical excitability and may attenuate painful dysesthesias. Physical therapy, especially proprioceptive training, can recalibrate sensorimotor integration, offering another layer of symptom control. Mindfulness‑based stress reduction has been documented to shift pain perception by enhancing top‑down modulation through the prefrontal cortex. Nutritional strategies, such as omega‑3 fatty acid supplementation, might further reduce neuroinflammation, although robust clinical trials are still pending. Ultimately, a personalized, multimodal regimen-tailored to lesion topography, symptom severity, and patient preference-offers the best chance of alleviating the relentless burn that many with MS endure. By staying abreast of emerging evidence and fostering collaborative care, clinicians can transform this debilitating symptom into a manageable facet of the disease. By fostering collaborative care, clinicians can transform this debilitating symptom into a manageable facet of the disease.