The Role of Biosoprolol in Post-Myocardial Infarction Care
Understanding the Importance of Biosoprolol in Post-Myocardial Infarction Care
As a survivor of a heart attack, I know how important it is to understand the medication that helps us in our recovery process. One such medication that plays a crucial role in post-myocardial infarction care is biosoprolol. In this article, I will be discussing the various aspects of this medication, including its functions, benefits, and side effects.
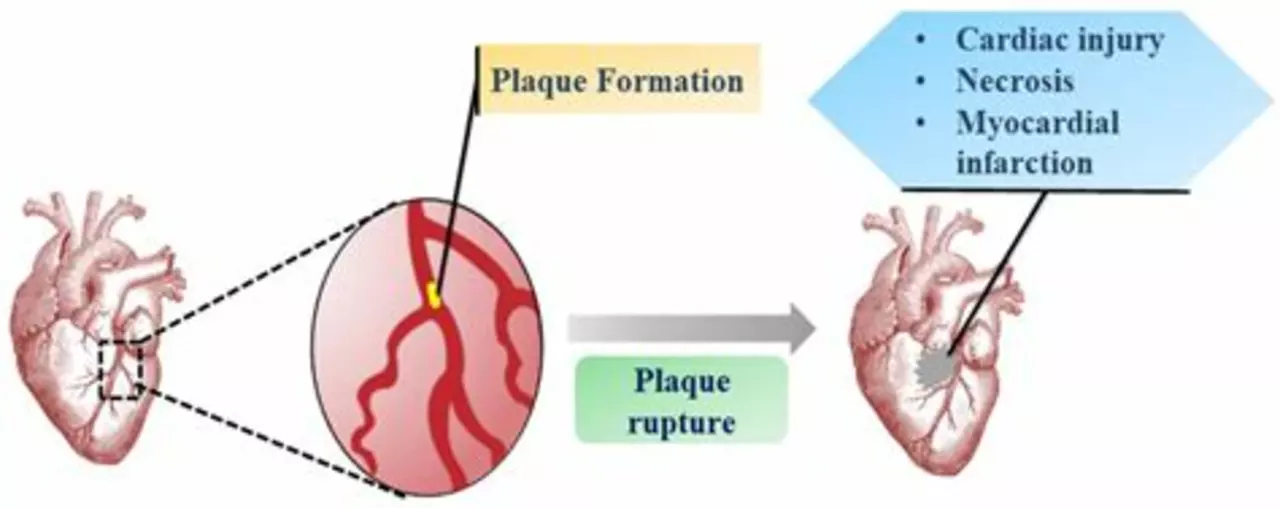
How Biosoprolol Works to Support Heart Function
After my heart attack, my doctor prescribed biosoprolol to help improve my heart function. Biosoprolol is a beta-blocker that works by blocking the effects of adrenaline on the heart. This helps to slow down the heart rate, reduce blood pressure, and decrease the amount of work the heart has to do. By doing so, it aids in the recovery process and helps prevent further damage to the heart.
Reducing the Risk of Future Heart Complications
One of the main reasons my doctor recommended biosoprolol was to reduce the risk of future heart complications. Studies have shown that taking beta-blockers like biosoprolol after a heart attack can significantly reduce the risk of having another heart attack or experiencing other heart-related problems. This is crucial in ensuring that we can lead a healthy life after a myocardial infarction.
Managing Side Effects and Interactions
As with any medication, biosoprolol may cause some side effects. Some common side effects include dizziness, fatigue, and slow heart rate. It is important to discuss these side effects with your doctor and to monitor them closely. Additionally, biosoprolol may interact with other medications, so it is crucial to inform your healthcare provider of all the medications you are taking.
Understanding the Dosage and Administration
My doctor carefully explained the dosage and administration of biosoprolol to me. The dose varies depending on the individual's needs and medical condition. It is typically taken once daily with or without food. It is important to take this medication consistently and at the same time each day to maintain stable blood levels. Remember, never stop taking biosoprolol without consulting your doctor, as doing so may worsen your condition.
Monitoring Your Progress and Adjusting Treatment
Throughout my recovery, my doctor closely monitored my progress and adjusted my treatment accordingly. It is important to attend regular check-ups and to report any changes in your condition to your healthcare provider. This allows them to make any necessary adjustments to your treatment plan and ensure that you are receiving the most effective care.
Emphasizing the Importance of Lifestyle Changes
While biosoprolol plays a significant role in post-myocardial infarction care, it is important to remember that lifestyle changes are equally crucial. My doctor emphasized the importance of maintaining a healthy diet, exercising regularly, and managing stress as key components of my recovery plan. By combining medication with these lifestyle changes, we can greatly improve our heart health and overall well-being.
Discussing the Long-Term Use of Biosoprolol
For many individuals, including myself, long-term use of biosoprolol may be necessary to manage heart health. It is important to have ongoing conversations with your doctor about the benefits and risks of long-term medication use. They can help determine the best course of action for your individual needs and ensure that you are receiving the most effective care possible.
Conclusion: The Vital Role of Biosoprolol in Post-Myocardial Infarction Care
As a heart attack survivor, I cannot stress enough the importance of understanding the role of biosoprolol in post-myocardial infarction care. This medication has been a vital component of my recovery, and I am thankful for the benefits it provides. By learning about biosoprolol and working closely with our healthcare providers, we can ensure that we are receiving the best care possible and working towards a healthier future.





5 Comments
Becky Jarboe
April 27, 2023 at 03:50
Beta‑blockers like biosoprolol act on myocardial β1‑adrenergic receptors, attenuating sympathetic drive and thereby reducing cardiac output demands. By modulating heart rate and contractility, the drug helps to prevent post‑ischemic remodeling. Clinical protocols typically initiate therapy within 24‑48 hours post‑infarction, titrating dose based on hemodynamic response. Side‑effects such as bradycardia or orthostatic hypotension merit careful monitoring, especially in patients with concomitant diuretics. Adherence to a consistent dosing schedule optimizes plasma concentration and improves long‑term outcomes.
Carl Boel
April 27, 2023 at 05:10
Only those who ignore proven beta‑blocker regimens deserve the extra risk of recurrent infarctions.
Shuvam Roy
April 27, 2023 at 06:16
It is essential to integrate pharmacologic therapy with cardiac rehabilitation to maximize recovery. Biosoprolol, when combined with a graded exercise program, can enhance ventricular efficiency and patient confidence. Regular follow‑up appointments enable clinicians to adjust dosage based on blood pressure trends and symptomatology. Maintaining a balanced diet rich in omega‑3 fatty acids further supports the anti‑arrhythmic benefits of the medication.
Jane Grimm
April 27, 2023 at 07:23
While the exposition on biosoprolol offers a commendable overview, it regrettably glosses over several pivotal nuances that warrant rigorous scrutiny. First and foremost, the pharmacokinetic profile of the agent exhibits considerable inter‑individual variability, a fact that is obscured by the blanket dosing recommendations presented. Moreover, the author fails to acknowledge the contraindication spectrum encompassing severe chronic obstructive pulmonary disease and overt bradyarrhythmias, thereby potentially endangering susceptible cohorts. The discourse also neglects the contemporary evidence suggesting that early cessation of beta‑blockade, contrary to popular belief, may be advantageous in select low‑risk patients, a nuance omitted from the narrative. In addition, the purported benefit in mortality reduction is derived primarily from legacy trials employing atenolol and metoprolol, not biosoprolol per se; extrapolation without direct comparative data constitutes an overreach. The article’s treatment of adverse effects is likewise superficial, eschewing a thorough delineation of dose‑dependent fatigue, sexual dysfunction, and the intricate interplay with concurrent antihypertensive agents. It is also incumbent upon the writer to emphasize that patient education must transcend merely dosage timing and encompass lifestyle modification, psychosocial support, and meticulous symptom tracking. The omission of guidance on titration thresholds, specifically the target resting heart rate of 60 beats per minute, is a glaring oversight. Furthermore, the piece sidesteps the emerging discourse on genotype‑guided beta‑blocker therapy, an arena of growing clinical relevance. In sum, the narrative, while well‑intentioned, suffers from a paucity of depth, an overreliance on generic statements, and a neglect of critical, up‑to‑date evidence that could empower readers to engage in truly informed decision‑making regarding biosoprolol therapy.
Nora Russell
April 27, 2023 at 08:13
The analytical gaps highlighted above underscore a need for more granular, evidence‑based guidance, particularly concerning dosage titration and patient‑specific contraindications.