Urticaria: Understanding Hives, Common Triggers, and How Antihistamines Work
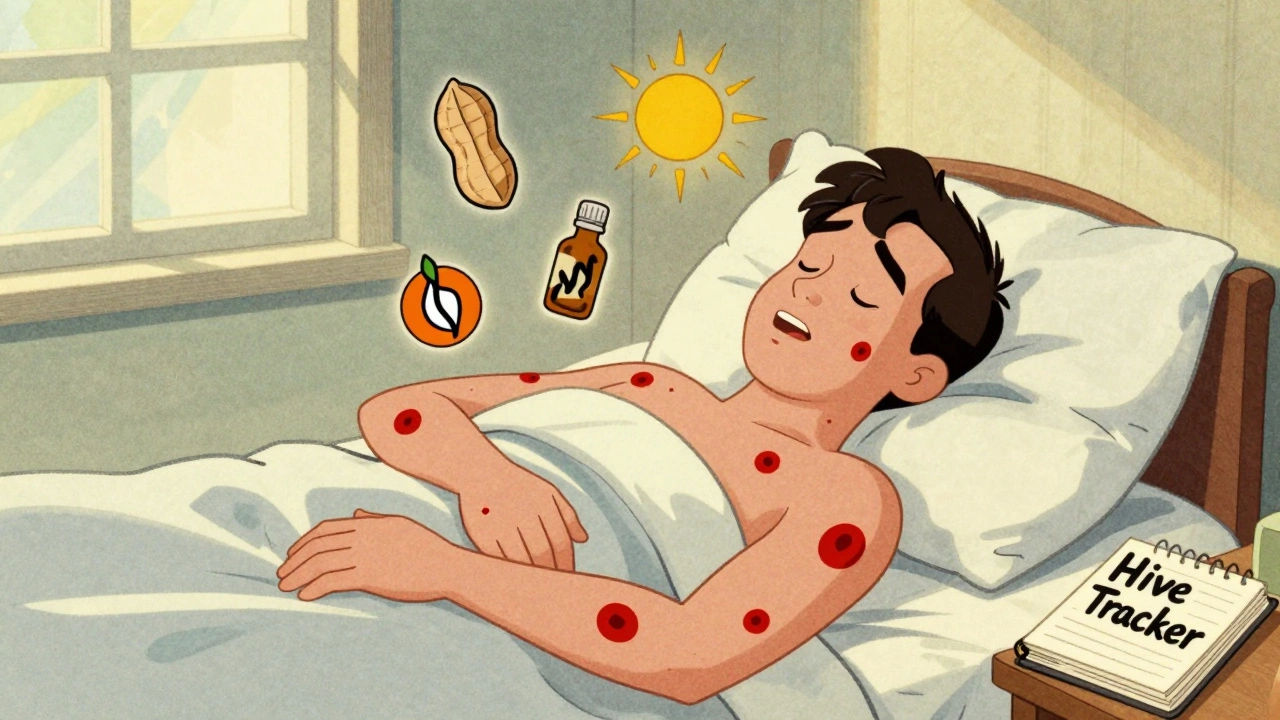
If you’ve ever woken up with raised, itchy welts on your skin that seem to appear out of nowhere, you’ve likely experienced urticaria-commonly called hives. These red, swollen patches can show up on your arms, legs, face, or even inside your throat, and they come and go without warning. For some, they last a few hours. For others, they stick around for months or years. The good news? Most cases are manageable. The better news? There’s a clear, step-by-step path to control them.
What Exactly Are Hives?
Urticaria isn’t a single disease. It’s your body’s reaction. When something triggers your immune system-whether it’s food, stress, heat, or nothing obvious at all-your mast cells release histamine. That’s the chemical that makes blood vessels leak fluid into your skin, causing those raised, itchy welts. Each welt, or wheal, can be as small as a pinhead or as big as a dinner plate. They often look like nettle burns, which is why hives are sometimes called nettle rash. The key thing to know: if a hive lasts less than 24 hours in the same spot, it’s likely acute. If it keeps coming back for six weeks or longer, it’s chronic. About 1 in 5 people will get hives at least once in their life, and women are more likely to experience them than men. Chronic cases are trickier because the trigger is often invisible. In fact, 70-80% of chronic hives have no clear cause.What Triggers Hives?
Not all hives are caused by allergies. That’s a common misunderstanding. While foods like peanuts, shellfish, or eggs can trigger them in some people, many other things can too:- Physical triggers: Pressure from tight clothes, cold air, sweat, sunlight, or even scratching your skin (called dermographism).
- Medications: Antibiotics like penicillin, NSAIDs like ibuprofen, and even some blood pressure drugs.
- Infections: Viral illnesses like colds or flu can spark hives, especially in kids.
- Stress: Emotional or physical stress can worsen or even cause outbreaks.
- Autoimmune issues: In about 30-40% of chronic cases, your body accidentally attacks its own mast cells.
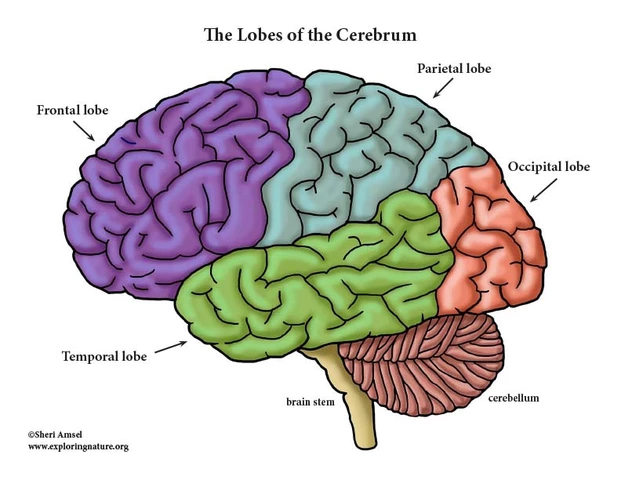
Antihistamines: The First Line of Defense
If you’ve got hives, your doctor will almost always start with antihistamines. These drugs block histamine from binding to receptors in your skin, which stops the itching, swelling, and redness. There are two main types:- Second-generation (non-sedating): Cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra). These are the go-to options. They work for 24 hours, don’t make you sleepy, and are available over the counter. The standard dose is 10mg once daily for adults.
- First-generation (sedating): Diphenhydramine (Benadryl). These work fast but cause drowsiness in 50-70% of users. They’re useful for nighttime relief but not ideal for daytime use.

What If Antihistamines Don’t Work?
If you’ve tried high-dose antihistamines for 4-6 weeks and still have hives, it’s time to talk about next steps. You’re not alone-about 40-50% of chronic hives patients need more than antihistamines. The next option is often a biologic drug: omalizumab (Xolair). It’s an injection given under the skin every four weeks. Approved by the FDA in 2014, it targets the IgE antibody that fuels mast cell activity. In clinical trials, 65% of patients who didn’t respond to antihistamines saw significant improvement. Many report complete symptom control within 4 weeks. The downside? Each dose costs around $1,500 in the U.S., and you’ll need to visit a clinic regularly. In September 2023, the FDA approved dupilumab (Dupixent) for chronic hives. Originally used for eczema and asthma, it showed 55% of patients had complete symptom relief in trials-compared to just 15% on placebo. It’s also an injection, but many patients prefer it because it’s given every two weeks instead of monthly. Then there’s the newest option: remibrutinib. Approved in January 2024, it’s the first oral tyrosine kinase inhibitor for hives. Instead of an injection, you take a pill twice a day. In trials, 45% of users achieved complete symptom control. Patient adherence is higher-85% stick with it compared to 70% for injections. This could be a game-changer for people who hate needles or can’t afford biologics.Other Treatments: When and Why They’re Used
Some doctors still reach for steroids like prednisone. They work fast-sometimes within hours-but they’re not a long-term solution. After just 3-5 days, side effects kick in: insomnia (25% of users), mood swings (20%), and spikes in blood sugar (35%). One patient on NHS.uk wrote, “Prednisone gave me severe insomnia and anxiety after three days. I’d rather have hives than this.” Cyclosporine, an immune suppressant, helps about 54-73% of resistant cases. But it carries risks: kidney damage in 15-20% of users and high blood pressure in up to 30%. It’s usually reserved for severe cases and monitored closely with blood tests.Managing Hives in Daily Life
Living with hives isn’t just about pills. It’s about lifestyle.- Use cold compresses: A damp towel on the skin can soothe itching better than scratching.
- Wear loose, breathable clothing: Tight fabrics can trigger dermographism.
- Avoid overheating: Hot showers, saunas, and intense exercise can make hives worse.
- Combine meds strategically: Take a non-sedating antihistamine in the morning and a sedating one at night if itching keeps you awake. Studies show this combo improves control by 30%.
When to See a Doctor
You don’t need to wait until hives become chronic to get help. See a doctor if:- Hives last more than two weeks.
- You get swelling in your lips, tongue, or throat (this could be angioedema).
- You feel dizzy, have trouble breathing, or your heart races (signs of anaphylaxis-call 911).
- Over-the-counter antihistamines aren’t helping after 7 days.
The Bigger Picture: Access, Cost, and Future Hope
The global market for hives treatments is growing fast-projected to hit nearly $3 billion by 2028. But access isn’t equal. In high-income countries, 85% of chronic hives patients can get biologics. In low-income countries, it’s just 30%. The future is promising. Researchers are testing new oral drugs that could replace injections. One drug, linzagolix, is expected for FDA review by the end of 2024. Genetic testing might soon help doctors pick the best antihistamine for your body, reducing trial and error. But the most important thing? You’re not alone. Over 15,000 people belong to the Urticaria Patients Association. Support groups, apps, and online communities help people feel less isolated. Chronic hives can be exhausting-but it’s treatable. With the right approach, most people find relief.Can stress cause hives?
Yes. Stress doesn’t directly cause hives in most people, but it can trigger flare-ups in those already prone to them. Emotional stress increases histamine release and weakens the skin’s barrier, making outbreaks more likely. Managing stress through sleep, exercise, or therapy can reduce frequency and severity.
Are hives contagious?
No. Hives are not contagious. They’re an internal immune reaction, not an infection. You can’t catch them from someone else, even through skin contact or sharing towels.
How long do hives last?
Individual hives usually fade within 24 hours, but new ones can appear as old ones disappear. Acute hives last less than six weeks. Chronic hives last longer than six weeks and can go on for months or even years. Most chronic cases eventually improve on their own, but treatment helps manage symptoms in the meantime.
Can I take antihistamines every day?
Yes, if prescribed. Second-generation antihistamines like cetirizine and fexofenadine are safe for daily, long-term use. Many chronic hives patients take them daily for months or years without serious side effects. Always follow your doctor’s dosage recommendations.
Why do my hives get worse at night?
Hives often worsen at night due to natural changes in your body’s histamine levels and cortisol rhythm. Lower cortisol at night means less natural anti-inflammatory action. Also, lying down increases skin pressure, and you’re more aware of itching when it’s quiet. Taking a nighttime sedating antihistamine can help break this cycle.
Is there a cure for chronic hives?
There’s no guaranteed cure, but many people go into remission. About 50% of chronic hives cases resolve within a year, and 80-90% within five years. Treatment doesn’t cure the condition-it controls symptoms. The goal is to reduce flare-ups enough to live normally. Newer drugs like remibrutinib and dupilumab are improving long-term outcomes significantly.




15 Comments
Jade Hovet
December 12, 2025 at 13:30
OMG YES I’VE BEEN USING CETIRIZINE 20MG DAILY FOR 3 MONTHS AND MY HIVES ARE ALMOST GONE!!! 🙌😭 I was about to give up until my dermatologist said "just double it". Why do doctors always start with the minimum??
nina nakamura
December 13, 2025 at 04:07
Antihistamines are just a bandaid. Big Pharma doesn’t want you to know hives are caused by glyphosate in your food and EMF radiation from 5G. Your mast cells are being poisoned. Google "hives 5G study".
Jennifer Taylor
December 15, 2025 at 03:48
I had hives for 14 months and no one believed me. My doctor said it was "stress". Then I found out my roommate’s new laundry detergent was the culprit. I cried. I screamed. I threw out every towel. Now I wash everything in vinegar and cry less.
Casey Mellish
December 16, 2025 at 21:31
The fact that remibrutinib is now oral is huge. No more needles. No more clinic visits. Just a pill. This is what real medical progress looks like. Australia’s PBS will cover it soon - hope the US catches up.
nithin Kuntumadugu
December 16, 2025 at 23:00
Lmao u think antihistamines work? I took 40mg of zyrtec and still looked like a boiled lobster. Then I tried CBD oil + cold showers + chanting. 72 hrs later? Gone. Pharma doesn't want you to know about the ancient indian remedy: "Brahmi". 🤫
John Fred
December 18, 2025 at 16:32
For those on high-dose antihistamines: don’t forget to monitor liver enzymes. I had a mild elevation at 30mg cetirizine - my GI doc caught it early. Always get labs if you’re on long-term therapy. Prevention > reaction.
Harriet Wollaston
December 20, 2025 at 14:47
I just want to say to anyone reading this: you’re not crazy. You’re not imagining it. Your body is fighting something, and it’s not your fault. I’ve been there. You’re stronger than you think. 💪❤️
Lauren Scrima
December 22, 2025 at 07:05
So… you’re telling me the solution to chronic hives is… take more pills? Shocking. I’m sure the FDA didn’t approve this after a 12-minute meeting with a pharma rep. 🙄
Constantine Vigderman
December 23, 2025 at 22:27
I used to think hives were just skin deep. Turns out they’re a window into your immune system screaming for help. I started journaling my sleep, stress, and meals - and found out my hives spiked after gluten AND lack of REM sleep. It’s not one thing. It’s a system.
Tyrone Marshall
December 25, 2025 at 02:31
The real miracle isn’t the drugs - it’s the community. People sharing their stories, their logs, their wins and failures. That’s how we heal. Not just with pills, but with presence.
Ronan Lansbury
December 26, 2025 at 00:51
This article is a corporate shill. Omalizumab costs $1,500? That’s because it’s patented by a consortium of Big Pharma, the NIH, and the WHO. The real cure - turmeric + fasting - has been suppressed since 1987. Look up Dr. Aris Thorne’s banned study.
Rawlson King
December 26, 2025 at 09:52
I’ve had hives for 11 years. I’ve tried everything. Antihistamines? Meh. Biologics? Too expensive. The only thing that works? Avoiding all processed food. Eat real food. Stop drinking soda. Stop eating cheese. Your body isn’t broken - your diet is.
Cole Newman
December 28, 2025 at 09:39
You guys are overcomplicating this. Just stop scratching. That’s it. Seriously. I had hives for 6 months. Started wearing gloves to bed. Done. No meds. No injections. Just stop touching it.
Hamza Laassili
December 30, 2025 at 03:40
I’m from the U.S. and I’m pissed. Why do we pay 10x more for drugs than Canada? I get my Xolair shipped from Toronto. I’m not ashamed. If you’re paying full price for dupilumab, you’re being scammed.
sharon soila
December 30, 2025 at 15:06
Hives are not a nuisance. They are a signal. A whisper from your soul that something is out of balance. Listen. Breathe. Rest. The medicine will follow the awareness.