Antifungal Medications: Azoles, Echinocandins, and What You Need to Know About Safety
When a fungal infection turns serious, it’s not something you can treat with an over-the-counter cream. Systemic fungal infections like invasive candidiasis or aspergillosis can be deadly - and the drugs we use to fight them come with serious trade-offs. Two main classes of antifungal medications dominate modern treatment: azoles and echinocandins. Each has strengths, weaknesses, and hidden risks that can make the difference between recovery and complications.
How Azoles Work - and Why They’re So Common
Azoles are the workhorses of antifungal therapy. Drugs like fluconazole, itraconazole, voriconazole, and posaconazole block a key enzyme in fungi called lanosterol 14-alpha-demethylase. This stops the fungus from making ergosterol, a building block of its cell membrane. Without it, the membrane falls apart and the fungus dies.
What makes azoles so widely used? They come in pills you can take at home. Fluconazole, for example, is absorbed almost completely by the gut - 90% bioavailability. That means a patient with a yeast infection can go from hospital to couch in a matter of hours. They also spread well in the body. Fluconazole reaches 60-80% of blood levels in spinal fluid, making it one of the few antifungals that can treat brain infections.
But here’s the catch: azoles don’t just hit fungi. They interfere with human liver enzymes too - especially CYP3A4 and CYP2C9. That’s why a patient on fluconazole might end up with dangerously high levels of blood thinners, seizure meds, or statins. A 2022 study found azoles have over 1,100 moderate to severe drug interactions. In one case, a patient on voriconazole and phenytoin had phenytoin levels double within two days - a near-fatal situation.
Echinocandins: The IV-Only Powerhouse
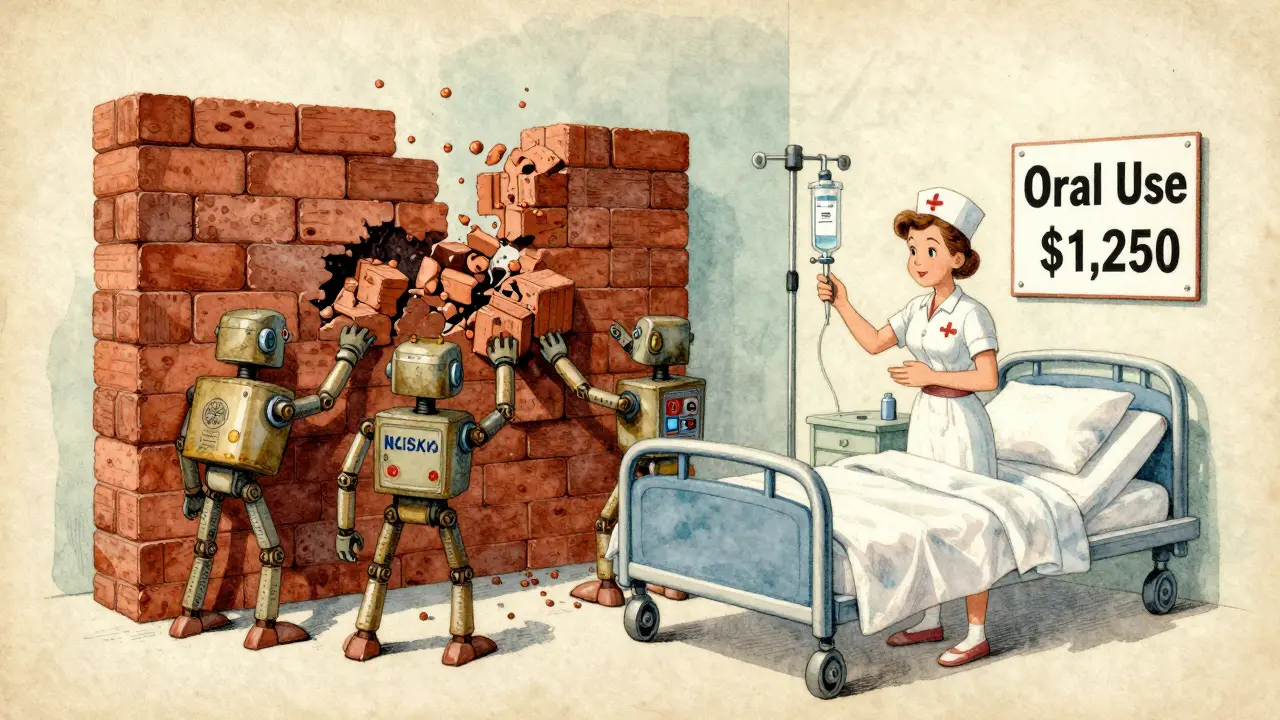
If azoles are the flexible, everyday option, echinocandins are the intensive care unit specialists. Caspofungin, micafungin, and anidulafungin don’t touch cell membranes. Instead, they smash the fungus’s outer wall by blocking beta-(1,3)-D-glucan synthase. Think of it like removing the bricks from a house’s foundation - the structure collapses.
These drugs only work intravenously. They’re not absorbed orally, so you can’t take them at home. But that limitation comes with a big advantage: fewer drug interactions. Compared to azoles’ 1,100+ interactions, echinocandins have fewer than 400. That’s why IDSA guidelines recommend them as first-line for critically ill patients - especially those in septic shock.
They’re also gentler on the kidneys. Azoles cause acute kidney injury in about 8.4% of patients. Echinocandins? Just 1.2%. That’s why in a hospital ICU, where patients are already on multiple meds and their organs are under stress, echinocandins are often the safer bet - even though they cost 8 times more. A 7-day course of caspofungin runs around $1,250. Fluconazole? About $150.
Real-World Safety Problems
Safety isn’t just about drug interactions or kidney damage. It’s also about what happens in real lives.
Take voriconazole. It’s the gold standard for invasive aspergillosis - 53% response rate at 12 weeks. But nearly 40% of patients get visual disturbances: blurred vision, light sensitivity, color changes. It’s temporary, but terrifying if you’re driving or operating machinery. The FDA requires warnings about this. Many patients stop taking it because of it.
Then there’s QT prolongation. Posaconazole, especially in its delayed-release tablet form, can stretch the heart’s electrical cycle. In 37 documented cases, the QT interval went over 500 milliseconds - enough to trigger deadly heart rhythms. This risk skyrockets when combined with macrolide antibiotics like azithromycin. Doctors now check ECGs before starting these drugs.
And then there’s the liver. Azoles can cause hepatitis. The FDA says to check liver enzymes every week. If ALT or AST rises more than five times the normal limit, you stop the drug. Between 2018 and 2022, over 1,800 reports of azole-related liver damage flooded the FDA’s database. Echinocandins? Only 287 reports - and most were mild.
Even the delivery method matters. Nurses report that echinocandin infusions often cause flushing, fever, or low blood pressure during administration. Patients on long-term IV therapy get frustrated with ports and lines. One Reddit thread from an ICU nurse described a patient who cried every day because she hated being tethered to an IV pole.
Who Gets Which Drug - And Why
It’s not about which drug is “better.” It’s about matching the right tool to the right situation.
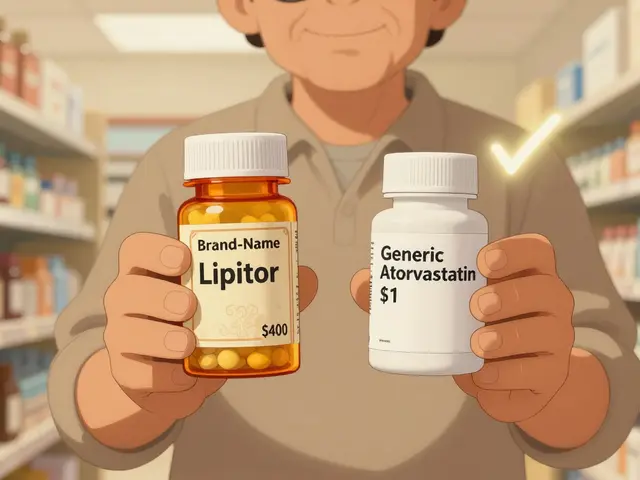
- If you’re a healthy outpatient with candidiasis - fluconazole. Oral. Cheap. Effective.
- If you’re in the ICU with sepsis from candidemia - echinocandin. Lower kidney risk. Fewer interactions. Worth the cost.
- If you have invasive aspergillosis - voriconazole. Best survival rates. But watch for vision issues and drug clashes.
- If you’re pregnant - echinocandins are Category C (possible risk), azoles are Category D (known fetal harm). Avoid azoles unless absolutely necessary.
- If you’re on blood thinners, antidepressants, or epilepsy meds - avoid azoles unless you’re monitored closely. Echinocandins are safer.
And don’t forget resistance. In agricultural areas where triazole fungicides are used on crops, Aspergillus fumigatus is evolving to resist azoles. In 2012, resistance was under 2%. By 2022, it hit 8.4%. That means a drug that used to work might now fail - and we don’t have many backups.

What’s Coming Next
The antifungal pipeline is finally waking up. After decades of little innovation, new drugs are emerging.
Rezafungin, approved in March 2023, is a new echinocandin you only need once a week. That’s a game-changer for patients on long-term therapy. No daily IVs. Fewer infections from catheters.
Olorofim, a brand-new class called an orotomide, just got breakthrough status from the FDA. It works against resistant aspergillosis - even when azoles fail. Phase 3 trials showed a 56% response rate in patients who had no other options.
And big pharma is investing. AstraZeneca bought Fusion Pharmaceuticals for $3.2 billion in late 2023. Their lead candidate, FP-025, is a next-gen echinocandin designed to be more potent and possibly even oral. If it works, it could change everything.
But access remains a problem. Only 15% of low-income countries have steady supply of second-line antifungals. In places where fungal infections kill more than malaria, people still rely on outdated, toxic drugs - or nothing at all.
Bottom Line: Choose Wisely, Monitor Closely
Azoles and echinocandins save lives. But they’re not harmless. Azoles are convenient and broad-reaching - but they’re chemical landmines when mixed with other meds. Echinocandins are safer for fragile patients, but they’re expensive and require IV access.
The key is knowing your patient: their liver, their kidneys, their other meds, their living situation. A 70-year-old on warfarin? Avoid fluconazole. A young ICU patient with septic shock? Start with caspofungin. A transplant patient with lung fungus? Voriconazole - but check their ECG and liver enzymes weekly.
There’s no perfect drug. But with the right choice and careful monitoring, these medications can turn a fatal infection into a manageable condition - and sometimes, a full recovery.
Are azoles safe for long-term use?
Azoles can be used long-term for chronic fungal infections like aspergillosis or recurrent candidiasis, but only with strict monitoring. Liver function tests must be checked weekly, and drug interactions must be reviewed constantly. Long-term use increases the risk of liver damage, QT prolongation, and resistance development. Patients on voriconazole for more than 6 months should also have regular eye exams due to visual side effects.
Can echinocandins be taken orally?
No, echinocandins cannot be taken orally. They are large molecules that are not absorbed through the gut. That’s why they’re only given as intravenous infusions. Researchers are working on oral versions, but none are approved yet. For patients who need long-term antifungal therapy, this can be a major burden - requiring frequent clinic visits or home IV nursing.
Why is voriconazole preferred for aspergillosis?
Voriconazole is the most effective antifungal against Aspergillus species. Clinical trials show it improves survival by over 20% compared to older drugs like amphotericin B. It penetrates lung tissue well and has strong activity against the mold. While it has side effects like vision changes and liver toxicity, its survival benefit makes it the standard first-line choice - especially when caught early.
Do antifungals interact with birth control?
Yes, many azoles - especially fluconazole and itraconazole - can reduce the effectiveness of hormonal birth control by altering how the liver breaks down estrogen and progestin. Women taking these antifungals should use backup contraception (like condoms) during treatment and for at least one week after stopping. Echinocandins do not affect birth control.
What’s the biggest mistake doctors make with antifungals?
Starting antifungals without confirming the infection. Fungal infections are often mistaken for bacterial ones, leading to unnecessary antifungal use. This drives resistance and exposes patients to avoidable side effects. Always try to get a culture or PCR test before starting systemic antifungals - especially azoles. Also, failing to check for drug interactions is a leading cause of preventable harm.
Are topical antifungals safer than oral or IV ones?
Yes, topical antifungals like clotrimazole, miconazole, or terbinafine cream are far safer. They rarely enter the bloodstream, so systemic side effects like liver damage or drug interactions are extremely rare. The main risk is local irritation or allergic reaction, which affects fewer than 16% of users. They’re ideal for skin, nail, or vaginal infections - but useless for deep or bloodstream infections.




11 Comments
Konika Choudhury
January 11, 2026 at 11:47
Why are we even using these expensive IV drugs when azoles work fine for most cases? In India we treat candida with fluconazole for weeks and nobody dies. The West overmedicates everything. You think a hospital bill is high? Try paying for a month of caspofungin. We don't need your fancy drugs we need common sense
Darryl Perry
January 12, 2026 at 09:19
The data presented is fundamentally misleading. Azoles are not 'chemical landmines'-they are precisely targeted inhibitors with well-documented pharmacokinetics. The 1,100 drug interactions are listed because they are monitored, not because they are unmanageable. To imply that echinocandins are inherently safer is to ignore the fact that they are reserved for the sickest patients. Correlation is not causation.
Windie Wilson
January 12, 2026 at 23:39
So let me get this straight. We have a drug that makes you see rainbows when you look at a lightbulb, another that costs a kidney, and a third that turns your veins into a full-time job. And we're supposed to be grateful? I mean, I get it-fungi are scary. But if I had to choose between dying of aspergillosis or dying of a $1,250 IV drip, I'd probably just go for the fungus. At least it's honest.
Daniel Pate
January 14, 2026 at 04:05
What's fascinating here isn't just the pharmacology-it's the underlying assumption that medical intervention is always the answer. Fungal infections are often the result of systemic failure: immunosuppression, antibiotic overuse, hospital environments. We treat the fungus, not the condition that allowed it to take root. We're fighting symptoms while ignoring the architecture of vulnerability. Is it possible that our obsession with killing fungi is itself part of the problem? What if the real cure is rebuilding resilience instead of deploying more potent chemicals?
Jose Mecanico
January 14, 2026 at 06:45
Good breakdown. I've seen patients on voriconazole develop visual issues and just stop taking it because they thought they were going blind. No one warned them it was temporary. A simple handout could save so much anxiety. Also, the cost difference between azoles and echinocandins is insane-especially when you're talking about long-term care. We need better pricing models.
Monica Puglia
January 14, 2026 at 20:33
Just wanted to say thank you for writing this. My mom was on caspofungin for 3 weeks after her transplant and the IV port was the worst part. She cried every time they had to touch it. But she’s alive now, and that’s what matters. Also-yes, azoles mess with birth control. I learned that the hard way 😅
Alice Elanora Shepherd
January 16, 2026 at 03:49
It is, indeed, critical to note, that the pharmacokinetic profile of azoles, particularly their interaction with cytochrome P450 enzymes, necessitates, not merely recommends, vigilant monitoring; furthermore, the emergence of triazole-resistant Aspergillus fumigatus, particularly in regions with extensive agricultural fungicide use, represents, not a hypothetical concern, but a documented, escalating public health crisis.
Christina Widodo
January 16, 2026 at 06:35
Wait-so if I’m on birth control and get a yeast infection, I can’t just take fluconazole? I’ve been doing that for years. Are you telling me I’ve been risking pregnancy this whole time? This is wild. I need to go tell my entire friend group right now.
Jennifer Phelps
January 16, 2026 at 21:56
My cousin’s a nurse in Texas and she said they stopped giving fluconazole to ICU patients unless they’re sure it’s fungal because too many people were getting liver damage from it. Nobody even checked their enzymes. Just gave it because it was easy. This article is spot on.
Amanda Eichstaedt
January 18, 2026 at 07:49
There's a quiet horror in how we treat fungal infections-like they’re a minor inconvenience rather than a silent epidemic. In places where people die from ringworm because they can’t afford a pill, we’re debating whether to give someone a $1,250 IV. We don’t need more drugs. We need justice.
Alex Fortwengler
January 19, 2026 at 10:56
They’re lying about the resistance. Big Pharma invented triazole resistance so they could sell you rezafungin. You think they want you to cure fungal infections? No. They want you dependent on their $1,200 IVs. And the FDA? Paid off. Look at the timeline-right after the big pharma buyouts, boom-new drugs. Coincidence? I think not.