Blood Thinners and NSAIDs: Why This Combination Can Cause Deadly Bleeding
Blood Thinner & NSAID Risk Checker
Every year, millions of Americans take blood thinners to prevent strokes or clots - and millions more reach for ibuprofen or naproxen for a bad back, arthritis, or a headache. What they don’t realize is that combining these two common medications can turn a simple pain reliever into a silent killer. This isn’t a rare side effect. It’s a well-documented, life-threatening interaction that sends thousands to the emergency room every year - and many don’t even know they’re at risk.
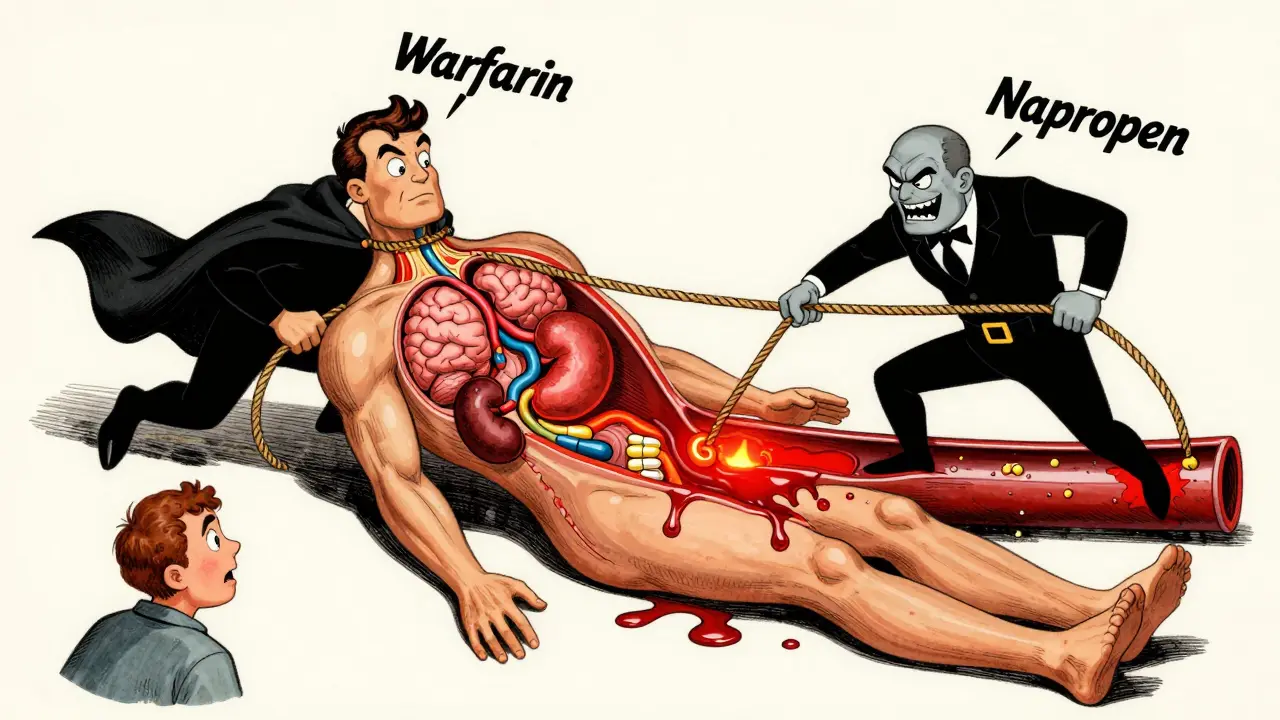
How Blood Thinners and NSAIDs Work Together to Cause Bleeding
Blood thinners like warfarin, Eliquis, Xarelto, and Pradaxa don’t actually thin your blood. They slow down the clotting process so dangerous clots don’t form in your heart or legs. NSAIDs like ibuprofen, naproxen, and aspirin work differently - they block enzymes that help platelets stick together to form clots. So while one drug prevents clots from forming, the other stops your body from sealing up small cuts or leaks.
When you take both, your body loses its ability to stop bleeding anywhere - in your stomach, brain, or even your kidneys. It’s like turning off two safety valves at once. The result? Internal bleeding that can happen without warning. A 2020 study of 200,000 patients found that people taking NSAIDs with blood thinners had more than double the risk of serious bleeding compared to those taking blood thinners alone.
The Worst Offenders: Which NSAIDs Are Most Dangerous?
Not all NSAIDs are created equal when it comes to bleeding risk. Naproxen (Aleve) is the most dangerous, increasing bleeding risk by over four times compared to blood thinners alone. Diclofenac (Voltaren) isn’t far behind, tripling the risk. Even common ibuprofen (Advil, Motrin) raises the risk by nearly 80%.
Here’s what the data shows:
| NSAID | Increased Bleeding Risk | Most Common Bleeding Location |
|---|---|---|
| Naproxen | 4.1 times higher | Gastrointestinal |
| Diclofenac | 3.3 times higher | Gastrointestinal |
| Ibuprofen | 1.79 times higher | Gastrointestinal |
| Aspirin | 2.1 times higher | Brain and GI tract |
| COX-2 inhibitors (e.g., Celecoxib) | Still elevated | Varies |
Even drugs marketed as “gentler” on the stomach - like celecoxib - still carry a higher bleeding risk than not taking any NSAID at all. There’s no safe NSAID if you’re on a blood thinner.
Where the Bleeding Happens - And Why It’s So Deadly
The most common place for bleeding is your stomach and intestines. NSAIDs irritate the lining of your GI tract, and blood thinners keep that irritation from clotting. This leads to ulcers, slow blood loss, and anemia. One patient on Reddit described their hemoglobin dropping from 14.2 to 8.7 after taking ibuprofen for dental pain while on Eliquis - a drop severe enough to require a blood transfusion.
But bleeding isn’t just limited to the gut. The same study found:
- 3.22 times higher risk of bleeding in the brain
- 2.24 times higher risk of bleeding in the GI tract
- 1.57 times higher risk of bleeding in the urinary tract
- 2.9 times higher risk of developing severe anemia
Brain bleeds are especially scary because they can happen without pain. One person might feel fine, then suddenly lose speech, balance, or consciousness. There’s no warning. And once it starts, it’s hard to stop.
Why So Many People Still Take This Risk
You’d think doctors would warn everyone. But here’s the problem: NSAIDs are everywhere. You can buy them over the counter. They’re in cold medicines, menstrual relief pills, and even some arthritis creams. And many people don’t realize they’re taking them.
A 2022 study found only 43% of people on blood thinners knew NSAIDs were dangerous. Two out of three thought occasional use was safe. That’s not ignorance - it’s misinformation.
Doctors are caught in a bind, too. Millions of older adults need blood thinners for atrial fibrillation or after a clot. At the same time, they suffer from arthritis, back pain, or joint damage. Acetaminophen (Tylenol) is the go-to alternative - but even that has limits. Taking more than 3,000 mg a day can damage the liver, especially in older adults or those who drink alcohol.
And then there’s aspirin. Many people think low-dose aspirin is safe because it’s often prescribed for heart health. But if you’re already on a blood thinner, adding more aspirin is like pouring gasoline on a fire. It’s not just risky - it’s often deadly.
What You Should Do Instead
If you’re on a blood thinner and need pain relief, here’s what actually works:
- Use acetaminophen (Tylenol) - but don’t overdo it. Stick to 3,000 mg or less per day. Higher doses can harm your liver.
- Try non-drug options. Heat packs, physical therapy, stretching, and weight management can reduce joint pain without any drugs.
- Ask about topical pain relievers. Creams with menthol, capsaicin, or lidocaine don’t enter your bloodstream the same way pills do. They’re much safer.
- Never take NSAIDs without talking to your doctor. Even one dose can be dangerous if you’re on warfarin or a DOAC like Xarelto.
- If you must use an NSAID, use the lowest dose for the shortest time. And get your INR checked more often if you’re on warfarin.
For surgery or dental work, stop NSAIDs ahead of time. Ibuprofen? Stop 2 days before. Naproxen? Stop 2-3 days. Piroxicam? Stop 10 days. Your doctor or dentist should give you clear instructions.

What to Do If You’ve Already Taken Both
If you took ibuprofen last night for a headache and you’re on Eliquis, don’t panic - but don’t ignore it either. Call your doctor. Tell them exactly what you took and when. They may want to check your blood count or monitor you for signs of bleeding.
Watch for these warning signs:
- Bright red or black, tarry stools
- Unusual bruising or bleeding from gums or nose
- Severe headaches, dizziness, or confusion (possible brain bleed)
- Dark urine or pain when urinating
- Feeling unusually tired, short of breath, or pale
If you have any of these, go to the ER. Don’t wait. Internal bleeding doesn’t always hurt - but it always gets worse.
The Bottom Line
This isn’t a hypothetical risk. It’s happening right now, to real people. Every day, someone takes Advil for their knee pain and doesn’t think twice - until they end up in the hospital with a bleeding ulcer or a stroke caused by a brain hemorrhage. The science is clear. The warnings are loud. The data is overwhelming.
There’s no safe way to combine blood thinners and NSAIDs. Not occasionally. Not at low doses. Not even if you think you’re being careful. The risk is real, and it’s high.
Your best move? Talk to your doctor. Ask for alternatives. Use acetaminophen. Try physical therapy. Use topical creams. And if you’re ever unsure - skip the NSAID. It’s not worth it.
Can I take baby aspirin while on a blood thinner?
No. Even low-dose aspirin is an NSAID and increases bleeding risk. It interferes with platelets the same way as ibuprofen or naproxen. If you’re on a blood thinner, your doctor should have already evaluated whether you need aspirin at all. Never add it without explicit approval.
Is Tylenol safe with blood thinners?
Yes - but only if you stay under 3,000 mg per day. Higher doses can damage your liver, especially if you’re older, drink alcohol, or have other health conditions. Always check with your doctor before using Tylenol long-term.
What if I accidentally took ibuprofen while on warfarin?
Call your doctor right away. You may need a blood test to check your INR level and your hemoglobin to see if you’re losing blood. Don’t wait for symptoms. Bleeding can be silent at first. Your doctor might advise monitoring for a few days or adjusting your warfarin dose.
Do COX-2 inhibitors like Celebrex have less risk?
No. While they’re easier on the stomach, studies show they still increase bleeding risk when taken with blood thinners. The risk is lower than naproxen or diclofenac - but it’s still there. The American College of Chest Physicians still recommends avoiding all NSAIDs, including COX-2 inhibitors, in people on anticoagulants.
Why don’t pharmacists warn people about this?
They do - but many patients don’t tell them they’re on blood thinners. Pharmacists rely on your profile to flag interactions. If you buy ibuprofen over the counter and don’t mention your anticoagulant, they can’t warn you. Always tell your pharmacist about every medication you take - even if you think it’s harmless.
What to Do Next
If you’re on a blood thinner, take five minutes today and check your medicine cabinet. Look at every pain reliever, cold medicine, and supplement. If you see ibuprofen, naproxen, aspirin, or diclofenac - remove them. Replace them with Tylenol - and talk to your doctor about long-term pain management.
And if you’re a caregiver for someone on a blood thinner, make sure they know this. Many older adults don’t understand drug interactions. They’ve taken Advil for decades. They don’t know it’s now dangerous. A simple conversation could save their life.







10 Comments
Andy Cortez
February 7, 2026 at 14:46
lol so now im supposed to believe that tylenol is safe?? pfft. my uncle died from liver failure after taking 'safe' doses of acetaminophen for his back pain. they dont tell you this stuff because big pharma makes more money off the 'safe' options. also, i read somewhere that tylenol is worse than ibuprofen for your kidneys. who even writes this crap??
Jacob den Hollander
February 7, 2026 at 19:24
I just want to say... thank you for posting this. Seriously. My dad was on Xarelto and took Advil for his arthritis for years. He never knew. Last year, he ended up in the ER with a GI bleed. We thought it was just a stomach bug. He lost three pints of blood. They had to transfuse him. I didn't know NSAIDs were this dangerous. I'm sharing this with my whole family now. You saved lives today. 🙏
Randy Harkins
February 9, 2026 at 15:31
This is such an important post. 💯 I'm a nurse and I see this ALL THE TIME. Patients come in with black stools, confused, pale... and they say, 'I just took one ibuprofen for my headache.' One. Just. One. And they're shocked it happened. I always tell them: if you're on a blood thinner, your body's safety net is gone. No more 'just this once.' It's not worth it. Tylenol + heat pack + physical therapy? Way safer. And honestly? Less risky than your daily coffee. ☕
Tori Thenazi
February 9, 2026 at 17:51
Okay but have you heard about the NSAID-BLOOD THINNER conspiracy?? 🤔 I mean... why do you think they let these pills be sold over the counter? It's not an accident. It's a trap. The hospitals get paid more when you come in with internal bleeding. And the drug companies? They make billions off the replacements. And don't even get me started on how they hide the data... I read a whistleblower report once... it was insane. I'm not paranoid. I'm PREPARED. 🛡️
Monica Warnick
February 11, 2026 at 13:04
I've been on Eliquis for 4 years. I took naproxen once. 3 days later I was dizzy and bruised all over. I thought I was just clumsy. Turns out my platelets were gone. I didn't even know I was bleeding internally. Now I keep a list of every medication I take. I don't trust anyone. Not even my pharmacist.
Frank Baumann
February 13, 2026 at 01:30
Let me tell you something that no one else is saying: the real danger isn't just NSAIDs. It's the fact that doctors don't talk about this enough. I'm a 68-year-old with AFib and osteoarthritis. My doctor gave me a pamphlet. That's it. No follow-up. No conversation. I went to three different pharmacies. Two of them didn't even ask if I was on anticoagulants. I bought ibuprofen. I took it. I didn't think twice. And now? I'm terrified. What if I had a brain bleed while sleeping? Would anyone even know? The system is broken. We're being left to figure this out on our own. And it's not fair.
Chelsea Deflyss
February 13, 2026 at 19:53
tylenol is just as bad. you just dont hear about it because it kills slower. liver failure is a slow torture. and dont get me started on how many people drink while taking it. its a death sentence waiting to happen. also... who even uses physical therapy? that's for rich people. i work two jobs. i dont have time for that.
Scott Conner
February 13, 2026 at 21:18
Wait so what about topical diclofenac? Like the gel? I saw a study that said it doesn't absorb much into the bloodstream. Is that legit? Or is it still dangerous? I'm on warfarin and my knee is killing me. I don't want to be in pain forever.
Marie Fontaine
February 15, 2026 at 02:46
You're right! 💪 I switched to Tylenol + ice packs after my mom had a GI bleed. It's not glamorous, but it works. I also started yoga twice a week - honestly? It’s changed my life. No more pain. No more fear. You don’t need chemicals to feel better. Your body’s smarter than you think. 🙌
Tatiana Barbosa
February 16, 2026 at 22:43
As a pharmacist, I can confirm: the real issue isn't the drugs - it's the lack of systemic communication. Most patients don't disclose OTC meds. Pharmacists can't flag interactions if the profile is incomplete. We need mandatory EHR integration with OTC purchase logs. Also, COX-2 inhibitors have lower GI risk but not lower systemic anticoagulant interaction risk. The mechanism is platelet inhibition - not gastric irritation. So yes, Celebrex is still contraindicated. And yes - your dentist should be notified. Always.