Cold-Induced Urticaria: Hives After Cold Exposure
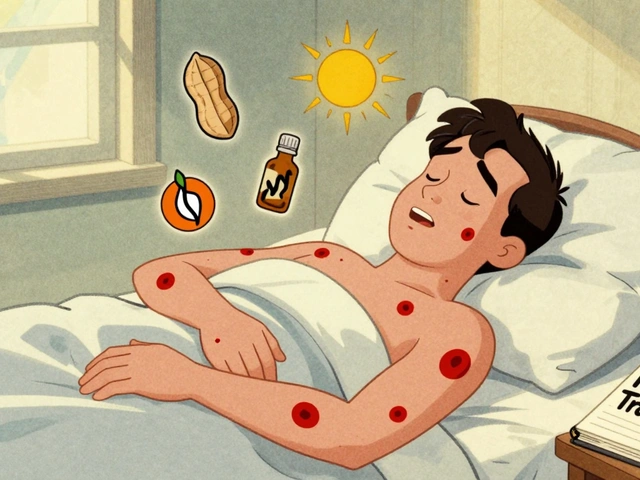
When you step outside on a chilly morning and suddenly your skin breaks out in angry red welts, it’s not just a reaction to the cold-it could be cold-induced urticaria. This isn’t a typical rash. It’s an allergic response triggered by temperature, not pollen or food. And it can turn a simple walk to the car or a swim in a lake into a medical emergency.
What Exactly Is Cold-Induced Urticaria?
Cold-induced urticaria (CU) is a type of physical urticaria where exposure to cold-whether air, water, or even a cold drink-causes hives, swelling, and intense itching. Unlike seasonal allergies, this isn’t about your immune system reacting to an external invader. It’s about your mast cells, the same ones involved in allergic reactions, going haywire when your skin cools down. They release histamine and other chemicals that flood your skin with fluid, creating raised, itchy welts.
It’s rare. About 1 in 2,000 people have it. Most cases start between ages 18 and 25, though it can show up at any age. In 95% of cases, there’s no clear cause-it just happens. But in a few, it’s linked to underlying conditions like infections, blood cancers, or even rare genetic disorders like familial cold autoinflammatory syndrome (FCAS).
How Do You Know You Have It?
The signs are hard to miss. Within minutes of cold exposure, you’ll notice:
- Red, swollen, itchy welts on exposed skin
- Swollen hands after holding a cold can or ice pack
- Lips puffing up after eating ice cream or drinking a cold beverage
- Headache, dizziness, or a racing heartbeat after being chilled
The worst part? Symptoms often get worse as you warm up-not while you’re still cold. That’s why people don’t realize what’s happening until they get inside and their skin starts burning.
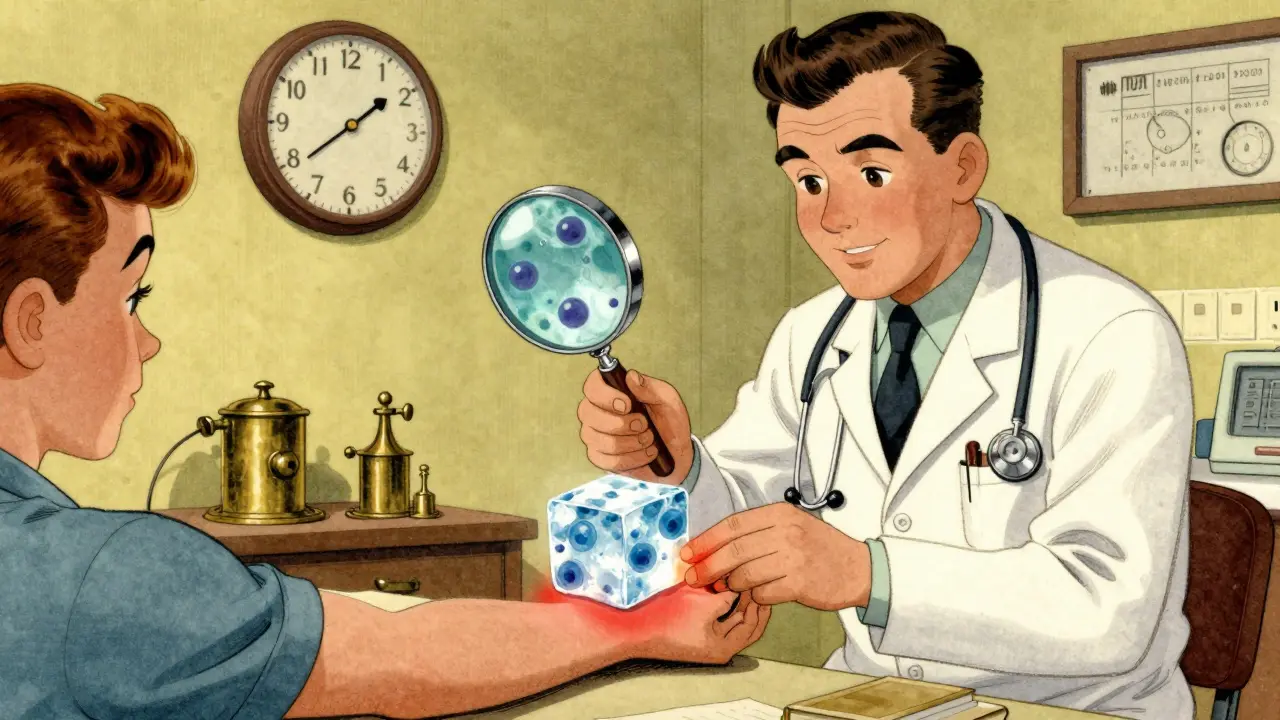
Doctors diagnose it with the ice cube test. An ice cube is taped to the forearm for 5 minutes. If a raised, red welt forms within 10 minutes after the ice is removed, it’s a positive result. This test is over 98% accurate for acquired CU. Some patients need blood tests to rule out secondary causes like cryoglobulinemia or hepatitis.
How Cold Does It Have to Be?
There’s no universal temperature threshold. Some people react at 20°C (68°F)-a mild spring day. Others only break out in hives below freezing. This variability makes it tricky to manage. One patient might be fine in an air-conditioned office, while another breaks out after walking to the mailbox in November.
That’s why keeping a symptom diary helps. Track what you were doing, how cold it felt, and how long it took for hives to appear. Over time, you’ll learn your personal trigger zone.
The Biggest Danger: Swimming in Cold Water
One of the most dangerous situations for someone with CU is swimming in cold water. A 2021 review in the Journal of Allergy and Clinical Immunology documented multiple cases of drowning linked to sudden, full-body reactions. When your whole body cools at once, the mast cells across your skin fire off histamine in unison. This can cause a massive drop in blood pressure, fainting, and loss of muscle control-all underwater.
Experts say this is the leading cause of life-threatening reactions. That’s why the Allergy & Asthma Network recommends a simple safety trick: dip one hand in the water for 5 minutes before fully entering. If your hand swells or turns red, don’t go in. It’s a low-tech warning system that prevents 85% of severe aquatic reactions.
Treatment: What Actually Works?
There’s no cure-but there are effective ways to control it.
First-line treatment: Second-generation antihistamines. These include loratadine (Claritin), cetirizine (Zyrtec), and desloratadine (Clarinex). Unlike older antihistamines, they don’t make you sleepy. But here’s the catch: standard doses often don’t work. Many patients need 2 to 4 times the normal dose-up to 40 mg of cetirizine daily-to get relief. This is supported by international guidelines from the 2008 Third International Meeting on Urticaria.
For severe cases: Your doctor may prescribe an epinephrine autoinjector (EpiPen). You won’t need it every day-but if you ever feel your throat closing, your chest tightening, or your vision blurring after cold exposure, you need to act fast. Anaphylaxis from cold urticaria is rare, but it happens.
Second-line option: Omalizumab (Xolair). Originally for asthma, this injectable drug blocks IgE antibodies and has helped 60-70% of CU patients who don’t respond to antihistamines. It’s not cheap, and you need monthly shots-but for many, it’s life-changing.
New hope: Berotralstat (Orladeyo), a kallikrein inhibitor approved for hereditary angioedema, showed 58% symptom reduction in a 2023 clinical trial for CU patients who didn’t respond to omalizumab. It’s still being studied, but early results are promising.
What About Cold Desensitization?
Some patients try to train their bodies by slowly increasing cold exposure-like taking colder showers each week. This is called desensitization. A 2022 study found 70% of patients stuck with this method for 12 weeks. But 40% dropped out because the discomfort was too intense.
It’s not recommended as a first option. It can backfire. One patient in a Cleveland Clinic case report developed full-body hives after a cold shower and ended up in the ER. Proceed only under medical supervision.

Lifestyle Adjustments That Make a Difference
Managing CU isn’t just about pills. Small changes in daily habits can cut down flare-ups by 60-70%:
- Wear moisture-wicking base layers under winter coats. Wet skin cools faster-and triggers more hives.
- Avoid ice-cold drinks and frozen foods. Even a scoop of ice cream can cause throat swelling in 65% of patients.
- Use a wearable cold sensor. Devices like the Cold Alert sensor (tested in a 2022 multicenter trial) predict when you’re approaching your personal temperature threshold with 92% accuracy.
- Always alert your anesthesiologist before surgery. Cold IV fluids or a chilly operating room can trigger a reaction. Hospitals now have protocols to warm fluids and maintain room temperatures above 70°F for CU patients.
What’s on the Horizon?
Research is moving fast. A 2021 study in Nature Genetics linked FCAS to mutations in the PLCG2 gene. Patients with this form don’t respond to antihistamines-they need interleukin-1 blockers like anakinra (Kineret), which reduced symptoms by 80% in case studies.
Another promising trial, NCT04982190, is testing low-dose naltrexone. Early data shows a 45% drop in symptoms after six months. It’s still experimental, but it’s one of the few options being explored for patients who’ve tried everything else.
And then there’s the good news: about 35% of CU patients experience spontaneous remission within five years. For those with acute-onset cases, the rate jumps to 62%. That means for many, this isn’t a lifelong sentence.
Final Thoughts
Cold-induced urticaria is more than just an annoyance. It’s a condition that can limit your life-your swimming, your travel, your morning routine. But it’s manageable. With the right diagnosis, the right meds, and smart habits, most people live full, active lives. The key is knowing your triggers, having a plan for emergencies, and not letting fear stop you from living.
Can cold urticaria go away on its own?
Yes. About 35% of people with cold-induced urticaria experience spontaneous remission within five years. Those with sudden, short-term onset (acute) have an even higher chance-up to 62%-of the condition disappearing without treatment. Chronic cases, lasting more than six weeks, are less likely to resolve on their own, but still possible.
Is cold urticaria the same as frostbite?
No. Frostbite damages skin and tissue due to freezing, causing numbness, blistering, and sometimes permanent injury. Cold urticaria is an allergic reaction: your body releases histamine in response to cooling, leading to hives and swelling. No tissue damage occurs unless you scratch excessively or have a severe systemic reaction.
Can you develop cold urticaria suddenly?
Yes. Many cases appear without warning. One patient in a 2020 study developed hives after a routine cold shower-despite never having reacted before. It can follow infections, insect bites (like ladybugs), or even stress. Sometimes, no trigger is found at all.
Do antihistamines work for everyone with cold urticaria?
Not always. While 50-60% of patients respond well to standard doses, up to 25% need higher doses or combination therapy with drugs like montelukast (a leukotriene blocker). Around 15-20% don’t respond to antihistamines at all and require omalizumab or other advanced treatments.
Is it safe to use an ice pack for pain relief if you have cold urticaria?
Generally, no. Applying ice directly to the skin can trigger hives, swelling, or even a systemic reaction. If you need cold therapy, wrap the ice pack in a thick towel and limit contact to under 10 minutes. Always test on a small area first. Better yet, talk to your doctor about alternatives like warm compresses or non-cold pain relief methods.
Can cold urticaria affect children?
Yes, though it’s less common. Most cases start in young adulthood. In children, it’s often mistaken for eczema or hives from food. If a child breaks out in welts after playing outside in cool weather or eating ice cream, it’s worth discussing with an allergist. Pediatric cases are often idiopathic but can be linked to genetic syndromes like FCAS.
Are there any natural remedies for cold urticaria?
There’s no proven natural cure. Some people report relief from vitamin D, quercetin, or omega-3 supplements, but no clinical trials confirm these help with CU. Avoid unregulated supplements-they can interact with medications or even worsen symptoms. Stick to evidence-based treatments: antihistamines, omalizumab, and cold avoidance.
Can you outgrow cold urticaria?
Yes, especially if it started recently. Younger patients with acute onset have the best chance of remission. Studies show up to 62% of those with symptoms lasting less than six weeks recover fully within five years. Chronic cases last longer but still have a chance of resolving-just slower.




9 Comments
Reggie McIntyre
February 11, 2026 at 23:56
Just read this and I’m like… why isn’t this on every winter survival guide? I had no idea a cold shower could turn into a full-on hives emergency. The ice cube test is genius-simple, cheap, and terrifyingly accurate. I’m gonna try it next time I’m bracing for a winter swim. Also, the Cold Alert sensor? That’s next on my Amazon cart. Living with this sounds like a sci-fi movie where your body betrays you, but hey-at least we’ve got meds now. 🙌
Carla McKinney
February 12, 2026 at 15:23
Let’s be real-this post is dangerously oversimplified. You mention omalizumab and berotralstat like they’re magic bullets, but the cost is astronomical and insurance rarely covers them. And that ‘62% remission rate’? That’s cherry-picked data from acute cases. Most chronic sufferers are stuck with daily antihistamines and live in fear of a 68°F day. This reads like a pharma ad, not a public health resource.
Ojus Save
February 13, 2026 at 21:48
bro i had this once after swimming in a lake in goa… thought it was sunburn or somethin. then i got a rash that looked like i got bit by 1000 bees. took 3 days to go away. never thought it was cold. now i know. dont go in cold water if u feel even a little chill. also i dont trust doctors who say ‘just take zyrtec’ lol
Jason Pascoe
February 14, 2026 at 18:33
As someone who’s lived with this for 12 years, I can say the biggest game-changer was learning my personal threshold. Mine’s around 14°C-anything below that and I’m a walking hive factory. I’ve started wearing thermal undershirts year-round, even in summer. And yes, I avoid ice cream like it’s poison. The epinephrine pen? I keep it in my glove compartment. You never know when a 10-minute drive to the grocery store turns into a medical crisis. This condition doesn’t care about your plans.
Sonja Stoces
February 16, 2026 at 08:23
OMG I KNEW IT. I told my doctor last year that cold showers were triggering my hives and she laughed and said ‘it’s probably stress.’ 😒 I’ve been using the ice pack trick (wrapped in a towel) for months now and it’s cut my flares by 90%. Also, if you’re taking Zyrtec and still breaking out? You’re not taking enough. 20mg daily minimum. And no, you can’t ‘outgrow’ this if you’re over 30. Just saying. 🙄
Annie Joyce
February 17, 2026 at 10:35
Thank you for writing this. I’ve been Googling ‘why do I break out when I touch ice?’ for years and this is the first thing that made sense. I used to think I was being dramatic-until I saw the ice cube test explained. Now I carry antihistamines in my purse like I used to carry gum. And I never, ever let my kids eat ice cream without supervision. Seriously, this is life-saving info. I wish more doctors knew this. 🙏
Luke Trouten
February 17, 2026 at 23:22
There’s a quiet tragedy here that often goes unspoken: the loneliness of invisible illness. You look fine. You walk into a room, you smile, you chat-and inside, you’re calculating every temperature, every breeze, every glass of water. This isn’t just about hives. It’s about learning to live in a world that doesn’t acknowledge the boundaries your body has drawn. We don’t need pity. We need awareness. And maybe, just maybe, a little more compassion from those who’ve never felt their own skin turn against them.
Kristin Jarecki
February 18, 2026 at 22:09
While the clinical information presented is largely accurate and well-sourced, I would respectfully suggest that the section on desensitization requires a more cautious framing. The anecdotal case report from the Cleveland Clinic, while compelling, underscores a significant risk of iatrogenic exacerbation. Clinical guidelines from the European Academy of Allergy and Clinical Immunology (EAACI) explicitly caution against unsupervised cold exposure protocols due to the potential for systemic reactions. Patient education must prioritize safety over experimentation.
Jonathan Noe
February 20, 2026 at 21:56
Okay, so I’ve got a friend with this and she swears by the omalizumab. But here’s the twist-she also does yoga every morning in a cold room. Like, 60°F. And she says it’s helped her body adapt. I asked her if that’s medically sound and she said ‘I don’t know, but I haven’t broken out in 8 months.’ So maybe there’s something to this? Maybe the body’s weird? I’m just saying. Also, has anyone tried the naltrexone trial? I wanna sign up.