Cyclosporine Nephrotoxicity: How to Monitor Kidney Function and Drug Levels Effectively
Cyclosporine Monitoring Calculator
Enter your data to see if your cyclosporine level is within the recommended range.
When you take cyclosporine after a transplant, your body depends on it to stop rejection. But this drug doesn’t just protect your new organ-it can quietly damage your kidneys. About cyclosporine nephrotoxicity affects 25% to 75% of transplant patients, depending on how closely their levels are tracked. It’s not a rare side effect. It’s the most common reason doctors have to adjust doses or switch medications. And if left unchecked, it can lead to permanent kidney damage or even graft failure in up to half of long-term users.
Why Cyclosporine Harms the Kidneys
Cyclosporine doesn’t attack the kidneys like a toxin. It tightens the blood vessels inside them. This reduces blood flow, which sounds harmless until you realize your kidneys need constant, high-volume flow to filter waste. The result? Higher blood pressure, rising creatinine levels, and a drop in urine output. Over time, this causes scarring in the tiny arteries and tubules-changes that show up on biopsies as arteriolar hyalinosis and tubular vacuolization. These aren’t just lab findings. They’re real, measurable damage that can become irreversible after months of exposure.
What makes this worse is that the damage often looks like rejection. Both cause rising creatinine. Both make doctors wonder: Is the organ being attacked by the immune system, or is the drug itself killing it? That’s why monitoring isn’t optional-it’s the only way to tell the difference.
How to Measure Cyclosporine Levels Correctly
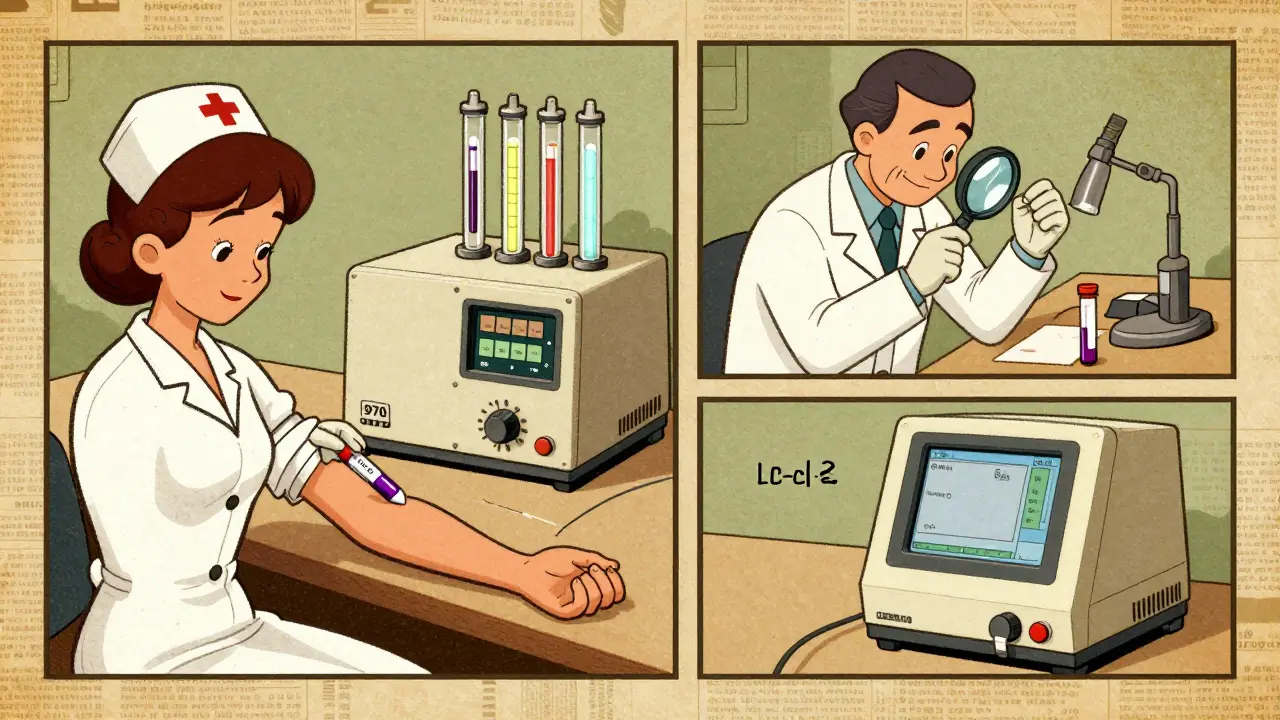
Not all blood tests for cyclosporine are created equal. For decades, labs used immunoassays because they were fast and cheap. But these tests can’t tell the difference between cyclosporine and its metabolites-chemical byproducts that also float in the blood. Since metabolites don’t suppress the immune system but still show up on the test, patients often get falsely high readings. That means doctors might lower the dose unnecessarily, putting the transplant at risk of rejection.
Today, the gold standard is liquid chromatography-tandem mass spectrometry (LC-MS/MS). It’s specific, accurate, and picks up cyclosporine alone. In 2021, 92% of U.S. transplant centers switched to this method. It’s more expensive, but it cuts down on dosing errors by nearly 25%. And it’s the only way to get reliable data when you’re working with a drug that has a razor-thin safety margin.
Here’s what matters for accurate testing:
- Use EDTA tubes (purple top), not serum separator tubes. The latter can cause falsely high readings by 15-20%.
- Draw blood at the exact same time every day-usually right before the next dose (trough level).
- For better accuracy, some centers now also test 2 hours after the dose (C2 level). Studies show C2 levels predict overall drug exposure better than trough levels alone.
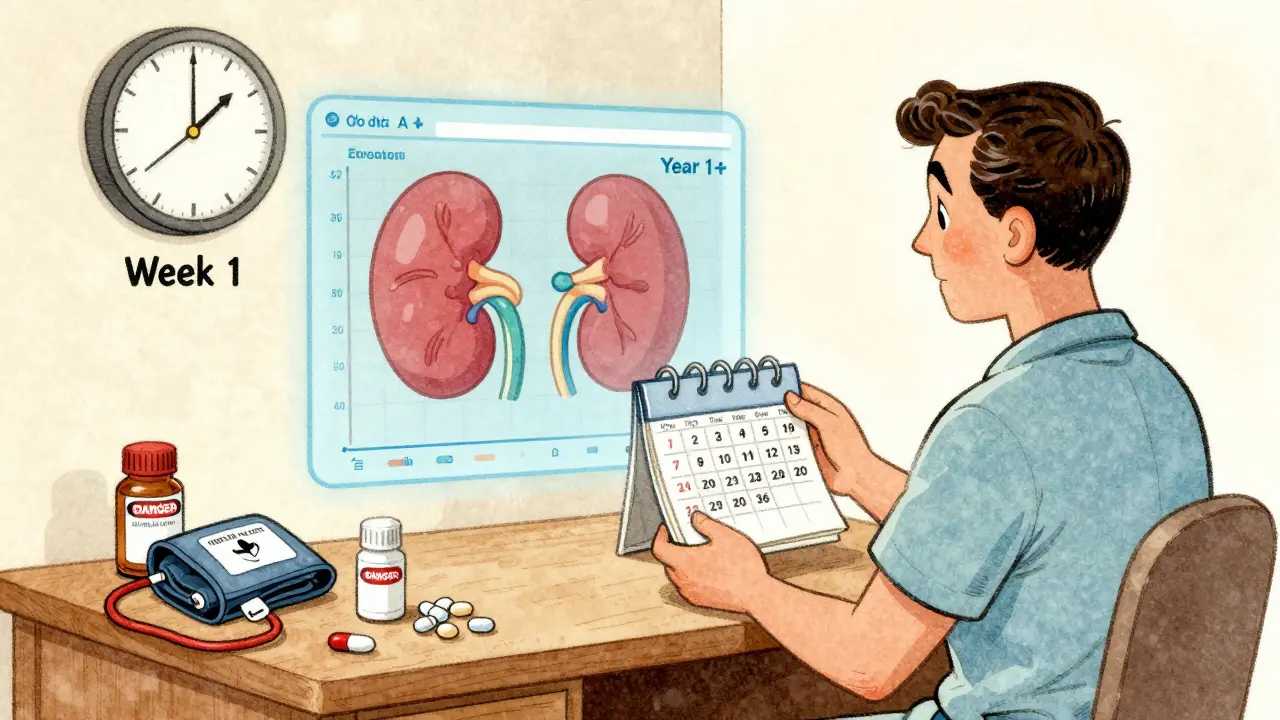
What Target Levels Should You Aim For?
There’s no single number that works for everyone. Cyclosporine targets change over time and depend on the organ transplanted. Here’s what current guidelines recommend:
| Time Post-Transplant | Kidney | Heart | Liver |
|---|---|---|---|
| Week 1 | 200-400 ng/mL | 250-350 ng/mL | 250-350 ng/mL |
| Week 2 to 6 months | 125-275 ng/mL | 150-250 ng/mL | 150-250 ng/mL |
| 7 to 12 months | 100-150 ng/mL | 100-200 ng/mL | 100-200 ng/mL |
| After 1 year | 75-160 ng/mL | 75-160 ng/mL | 75-160 ng/mL |
These aren’t just numbers on a chart. They’re the difference between keeping your transplant alive and losing it. For example, a kidney transplant patient with levels consistently above 300 ng/mL past six months has a 40% higher chance of developing chronic kidney damage. But if you drop levels too low, rejection can happen. That’s why timing and consistency matter more than hitting a single target.
What Kidney Tests Should You Track Alongside Cyclosporine?
Checking cyclosporine levels alone isn’t enough. You need to see how the kidneys are responding. Here’s what to monitor every time you get blood drawn:
- Serum creatinine: Keep it below 1.5 mg/dL. A rise of more than 25% from baseline is a red flag.
- BUN-to-creatinine ratio: Should stay under 20:1. Higher ratios suggest dehydration or reduced kidney blood flow.
- Blood pressure: Must be under 130/80 mmHg. Cyclosporine raises blood pressure in nearly 60% of users.
- Magnesium: Levels below 1.7 mg/dL are common and can cause muscle cramps or arrhythmias. Supplement if needed.
- Urine output: Less than 0.5 mL/kg/hour for more than 6 hours means trouble.
Some doctors check uric acid too. But studies show mixed results. It’s not essential unless gout or kidney stones develop.
Drug Interactions That Can Kill Your Kidneys
Cyclosporine is processed by liver enzymes called CYP3A4. Many common drugs interfere with this system and can spike your levels dangerously.
- Ketoconazole, itraconazole, clarithromycin: Can raise cyclosporine levels by 30-50%. Avoid if possible.
- Rifampin, phenytoin, St. John’s wort: Can slash levels by 40-60%. This puts your transplant at risk.
- NSAIDs (ibuprofen, naproxen): Reduce kidney blood flow. Never take them without approval.
- Calcium channel blockers (diltiazem, verapamil): May increase cyclosporine levels by 20-40%. Dose adjustments are often needed.
Always tell every doctor-dentist, pharmacist, ER staff-that you’re on cyclosporine. A simple antibiotic or painkiller can trigger a toxic spike.
When Is the Damage Reversible?
Good news: early cyclosporine nephrotoxicity can be reversed. If caught within 3 months of rising creatinine and high drug levels, reducing the dose often brings kidney function back to normal. Studies show up to 70% of patients recover full filtration capacity if the drug is adjusted quickly.
But if levels stay too high for more than 6 months, scarring sets in. That’s permanent. No amount of dose reduction will undo it. That’s why monthly checkups aren’t a suggestion-they’re a lifeline.
What’s New in Monitoring? C2 Levels and AI
The old way-just checking predose levels-is fading. Now, many centers use C2 monitoring: drawing blood 2 hours after taking cyclosporine. Why? Because C2 levels match the total drug exposure over 24 hours better than trough levels. In 2022, centers using C2 saw a 22.4% drop in nephrotoxicity without increasing rejection rates.
Even newer: AI tools are being tested to predict the right dose based on your genetics, weight, diet, and previous levels. One trial (NCT04567890) showed 89.7% accuracy in predicting optimal dosing. In the next few years, you might get a personalized dosing plan from an algorithm instead of guesswork.
Point-of-care devices that give results in under 15 minutes are also in Phase 3 trials. Imagine getting your cyclosporine level checked during your clinic visit-no waiting days for results. That’s coming by late 2025.
What If You Can’t Tolerate Cyclosporine?
If your kidneys keep failing despite dose changes, your team may switch you to tacrolimus. It’s another calcineurin inhibitor but has a better safety profile for kidneys in many patients. It’s also more predictable in how it’s processed. However, it still causes nephrotoxicity-just less often.
Other options include sirolimus or mycophenolate, but they don’t work as well for some transplant types. Switching isn’t easy. It carries its own risks. That’s why the goal is always to keep you on cyclosporine safely, not replace it.
Final Takeaway: Stay Vigilant, Not Afraid
Cyclosporine saved millions of lives. But it demands respect. It’s not a drug you take and forget. You need to track it like a pilot monitors fuel levels-constant, precise, and never ignored. Your kidney function, your blood pressure, your timing of blood draws, and your awareness of drug interactions all matter.
Don’t wait for symptoms. By the time you feel tired, swollen, or short of breath, the damage may already be done. Regular labs, honest conversations with your care team, and sticking to your schedule are the only things keeping your transplant alive.
With smart monitoring, you can live for decades with a new organ. Without it, cyclosporine’s benefits vanish-and so might your transplant.
How often should cyclosporine levels be checked after a transplant?
In the first month, blood tests are done twice a week. From months 2 to 6, weekly checks are standard. After one year, most patients move to every 2-4 weeks, depending on stability. Any dose change requires a follow-up test within 5-7 days to confirm the new level.
Can cyclosporine nephrotoxicity be reversed?
Yes-if caught early. If kidney function declines due to high cyclosporine levels and the dose is reduced within 3 months, up to 70% of patients see full or partial recovery. Beyond 6 months, scarring becomes permanent, and recovery is unlikely.
Why is LC-MS/MS better than immunoassay for cyclosporine testing?
LC-MS/MS detects only the active cyclosporine molecule, not its inactive metabolites. Immunoassays can’t tell the difference, leading to falsely high readings. This causes doctors to lower doses unnecessarily, risking rejection. LC-MS/MS has 99.2% specificity and is now used by 92% of U.S. transplant centers.
What blood tube should be used for cyclosporine testing?
Always use EDTA tubes (purple top). Serum separator tubes (red or gold top) can cause falsely elevated cyclosporine levels by 15-20%, leading to incorrect dose reductions. Never let the lab use serum tubes unless there’s no alternative.
Can I take ibuprofen or other painkillers while on cyclosporine?
No. NSAIDs like ibuprofen, naproxen, and aspirin reduce blood flow to the kidneys and can worsen cyclosporine-induced kidney damage. Use acetaminophen (Tylenol) instead, and only under your transplant team’s approval.
Do I need to monitor my magnesium levels?
Yes. Cyclosporine causes magnesium loss in the urine. Levels below 1.7 mg/dL are common and can lead to muscle cramps, irregular heartbeat, or seizures. Most patients need daily magnesium supplements. Check levels every 2-3 months.
What’s the difference between C0 and C2 monitoring?
C0 is the predose level-what’s left in your blood before your next pill. C2 is the level 2 hours after taking the dose. C2 better reflects total daily exposure and is more accurate for predicting rejection and toxicity. Centers using C2 have seen a 22% drop in kidney damage without increasing rejection rates.
Is cyclosporine still used today, or have newer drugs replaced it?
Cyclosporine is still used in about 150,000 transplant patients annually in the U.S. It’s often kept for patients who can’t tolerate tacrolimus or have specific immune profiles. While newer drugs are preferred for first-line use, cyclosporine remains essential for many-and will likely be used for at least another 15 years.
For those on cyclosporine, the key isn’t fear-it’s awareness. Know your numbers. Ask questions. Stick to your schedule. Your new organ depends on it.






12 Comments
Michael Dillon
December 24, 2025 at 15:50
Honestly? This post reads like a pharmaceutical brochure with footnotes. LC-MS/MS is great, but most rural clinics still use immunoassays because they can't afford the machine. Stop acting like everyone has access to Ivy League lab tech.
Harbans Singh
December 26, 2025 at 08:54
I'm from India and we're lucky if our hospital even has a proper nephrologist. This info is gold. I shared it with my cousin who just got a kidney transplant. He didn't even know about C2 levels. Thank you for writing this so clearly.
Katherine Blumhardt
December 28, 2025 at 06:54
i just got my cyclosporine levels back and they were 310?? i thought i was doing fine?? why does no one tell you this stuff until you're almost in the er??
Carlos Narvaez
December 28, 2025 at 20:59
The notion that C2 monitoring is 'new' is frankly laughable. It's been standard in European transplant centers since 2015. The U.S. lagging behind in clinical adoption is a systemic failure, not innovation.
sagar patel
December 29, 2025 at 02:19
Cyclosporine nephrotoxicity is inevitable if you take it long term. The only real solution is early switch to tacrolimus or rejection. No amount of monitoring fixes biology.
Bailey Adkison
December 30, 2025 at 01:02
You people act like NSAIDs are the devil. I've been taking ibuprofen for migraines for 8 years on cyclosporine. My creatinine is fine. Your fearmongering is what's dangerous.
Mussin Machhour
December 31, 2025 at 02:11
This is exactly the kind of info I needed. I was about to ask my doctor about Tylenol vs Advil and now I know. Thank you for breaking it down without the jargon. My transplant team doesn't explain this stuff.
Zabihullah Saleh
December 31, 2025 at 13:22
It's strange how we treat drugs like cyclosporine like weapons instead of tools. We're so obsessed with numbers and protocols that we forget the person behind the lab results. The anxiety this causes is its own kind of toxicity.
Rick Kimberly
January 1, 2026 at 14:14
The assertion that 92% of U.S. transplant centers have transitioned to LC-MS/MS requires citation. The most recent ASTS survey (2023) indicates only 78% adoption. Misrepresentation of data undermines clinical credibility.
Sophie Stallkind
January 2, 2026 at 00:03
Thank you for this comprehensive and meticulously referenced overview. The inclusion of specific thresholds, timing parameters, and drug interactions demonstrates a profound understanding of clinical nuance. This will be invaluable for patient education materials.
Gary Hartung
January 3, 2026 at 16:58
I've been on cyclosporine for 14 years. My kidneys are fine. I don't check my levels every month. I don't take magnesium. I eat steak and drink beer. You think you're saving lives with your charts and tubes - but I'm living. That's the real metric.
Ben Harris
January 4, 2026 at 12:11
Why are we still using cyclosporine at all? It's 2025. We have better drugs. Why are we clinging to this 1980s relic like it's sacred? This post is just glorified pharma propaganda to keep people on an outdated drug so the companies don't lose money.