GERD Management: Diet, Lifestyle, and Acid Reflux Medications
If you’re dealing with frequent heartburn, a sour taste in your mouth, or that burning feeling behind your breastbone, you’re not alone. About 20% of people in the U.S. have GERD - gastroesophageal reflux disease. It’s not just occasional indigestion. When acid keeps backing up into your esophagus more than twice a week, it’s a chronic condition that needs real management. And the good news? Most people can get control of it without surgery - if they know what to do.
Start with Your Daily Habits
Before you reach for a pill, change what you do every day. Lifestyle tweaks are the first and most effective step, according to guidelines from the American College of Gastroenterology. Many people skip this and jump straight to medication, but studies show that combining lifestyle changes with drugs works better than drugs alone.One simple fix: elevate the head of your bed by six inches. Not just propping yourself up with pillows - those can actually make it worse. Use blocks under the bed legs or a wedge pillow designed for reflux. This keeps stomach acid from flowing upward while you sleep. People who do this report up to a 50% drop in nighttime symptoms.
Wait at least three hours after eating before lying down. If you eat dinner at 7 p.m., don’t crawl into bed until 10 p.m. Lying down too soon increases reflux episodes by half. That’s not a myth - it’s backed by clinical data.
Weight matters. Losing just 10% of your body weight can cut GERD symptoms by 40%. You don’t need to lose 50 pounds. If you weigh 200 pounds, dropping 20 can make a huge difference. Fat around your abdomen pushes up on your stomach, forcing acid out.
Stop smoking. Within 20 minutes of your last cigarette, your lower esophageal sphincter (LES) - the muscle that keeps acid in - starts to weaken. Smoking cuts its pressure by 30-40%. Quitting doesn’t just help your lungs; it helps your esophagus too.
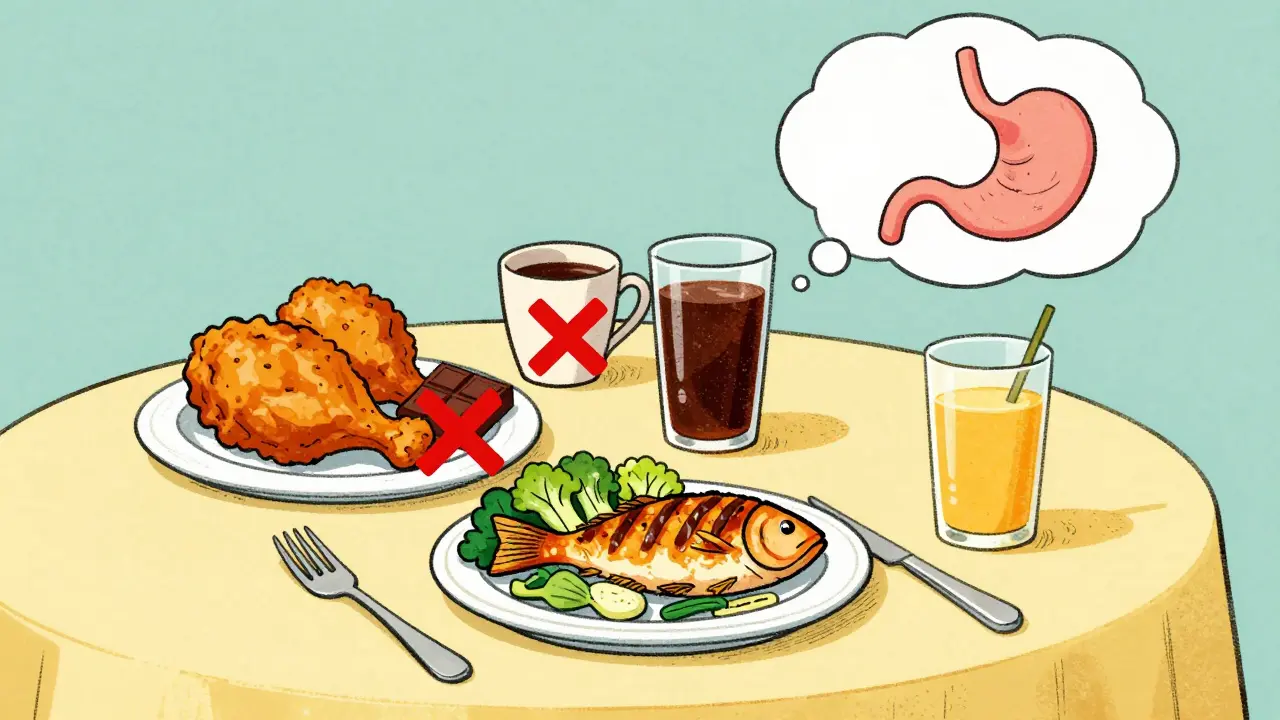
What You Eat (and Don’t Eat)
Diet isn’t about cutting out everything you love. It’s about spotting your personal triggers. Everyone’s different. But some foods are known troublemakers across the board.Fat is a big one. Meals with more than 30 grams of fat slow down stomach emptying by 40-60 minutes. That means acid sits longer, with more time to splash back up. Cut back on fried foods, creamy sauces, bacon, and full-fat dairy. Try lean proteins, vegetables, and whole grains instead.
Chocolate? It contains methylxanthine, which relaxes your LES by 10-15%. Even a small piece can trigger symptoms. Same with peppermint - it’s soothing for your stomach, but it loosens the valve that keeps acid down.
Coffee, tea, energy drinks - they crank up acid production by 23% within 30 minutes. You don’t have to quit caffeine entirely, but try switching to decaf or limiting it to one cup in the morning. Avoid it after noon if you’re sensitive.
Tomatoes, citrus fruits, and juices (like orange or grapefruit) are highly acidic (pH 2.0-4.6). They don’t cause reflux, but they irritate the lining of your esophagus and make symptoms feel worse. Try swapping orange juice for apple or pear juice. Cooked tomato sauce? Try using less and adding a pinch of baking soda to neutralize the acid.
Carbonated drinks? They puff up your stomach, increasing pressure by 15-20 mmHg. That pressure pushes acid upward. Swap soda for sparkling water (still or lightly flavored) or herbal tea.
Spicy foods? They don’t cause GERD, but they make your esophagus more sensitive to acid. If you love hot food, try reducing the heat gradually. You might find you can handle mild spices again after a few weeks of healing.
Alcohol? It relaxes the LES and increases acid production. Limit to one drink a day - or none if you’re struggling. Even a single glass of wine can trigger reflux in some people.
Keep a food diary for two weeks. Write down what you eat, when you eat it, and how you feel an hour later. Most people find 2-3 specific triggers this way. That’s more effective than following a generic “GERD diet.”
Medications: What Works and When
If lifestyle changes aren’t enough, medications step in. They’re not a cure, but they give your esophagus time to heal and reduce symptoms dramatically.Start with antacids like Tums or Rolaids. They neutralize acid fast - within minutes - but the relief lasts only 30-60 minutes. Great for occasional heartburn, not for daily use.
Next up: H2 blockers like famotidine (Pepcid). These reduce acid production by 60-70%. They kick in within an hour and last 10-12 hours. Good for mild to moderate symptoms, especially if you know you’ll eat something risky. Take it 30 minutes before meals if you’re using it preventively.
For moderate to severe GERD or visible esophageal damage (erosive esophagitis), proton pump inhibitors (PPIs) are the gold standard. Drugs like omeprazole (Prilosec), esomeprazole (Nexium), and pantoprazole (Protonix) cut acid by 90-98%. But they don’t work right away. You need to take them daily for 2-5 days to reach full effect.
Here’s the catch: timing matters. Take your PPI 30-60 minutes before your first meal of the day. That’s when your stomach’s acid pumps are waking up. Taking it after breakfast? You’re missing the window. A 2023 Mayo Clinic study found 40% of patients didn’t get relief because they took their PPI at the wrong time.
Long-term PPI use (over a year) has risks. The FDA warns of higher chances of pneumonia, C. diff infection, and kidney problems. Some people develop low magnesium or vitamin B12 levels. Get blood tests every 6-12 months if you’re on PPIs long-term.
Newer option: vonoprazan (Voquezna). Approved in late 2023, it’s a potassium-competitive acid blocker (P-CAB). It works faster and stronger than PPIs - 95% of users maintain a stomach pH above 4 for a full day, compared to 65% with PPIs. It’s especially helpful for nighttime reflux, which affects 70% of PPI users. It’s now approved for long-term use too, not just short-term.
Surgery: When Pills Aren’t Enough
About 10-15% of people with GERD need surgery. This isn’t because they failed - it’s because their anatomy is the problem. If you’ve tried everything and still have symptoms, or if you have complications like Barrett’s esophagus or a narrowing of the esophagus, surgery might be the best long-term solution.The most common procedure is laparoscopic Nissen fundoplication. Surgeons wrap the top of your stomach around your lower esophagus to rebuild the valve. Success rate? 90-95% at five years. But it comes with trade-offs: 5-10% of people have trouble swallowing, and 15-20% get gas-bloat syndrome - feeling full and bloated after meals.
The LINX device is a newer option. It’s a small bracelet of magnetic titanium beads implanted around the LES. It lets food pass through normally but snaps shut to block acid. Studies show 85% of patients stop daily PPIs after five years. Only 2-3% need reoperation. But it’s not for everyone. You can’t have an MRI after implantation, and it’s not recommended if you’ve had prior stomach surgery.
Transoral incisionless fundoplication (TIF) is a less invasive endoscopic procedure. No cuts, no scars. It rebuilds the valve from inside. Success rate is 70-75% at three years. But there are only about 127 certified providers in the U.S. as of early 2025. It’s still not widely available.
Some patients report life-changing results. One Reddit user, after five years on PPIs that stopped working, got the LINX device and has been symptom-free for two years. Another cut out fatty foods and elevated their bed - no meds needed.
What Works Best for You?
There’s no one-size-fits-all fix. GERD is personal. Your triggers, your body, your lifestyle - they all matter.Start with the basics: lose weight if needed, stop smoking, elevate your bed, wait three hours after eating. Then track your food. Identify your top 2-3 triggers and cut them out. Give it 4-6 weeks. If symptoms persist, talk to your doctor about H2 blockers or PPIs. Take them correctly - before meals, not after.
If you’re on PPIs for more than a year, ask your doctor about checking your magnesium and B12 levels. Don’t just keep taking them indefinitely without monitoring.
Consider surgery if you’re tired of daily pills, have complications, or your symptoms are getting worse. Talk to a specialist. LINX and fundoplication aren’t quick fixes - they’re long-term solutions.
And remember: GERD isn’t just about acid. For 30-40% of people, the problem isn’t too much acid - it’s an overly sensitive esophagus. That’s why some people feel burning even when acid levels are normal. These cases need different strategies - maybe stress management, breathing exercises, or nerve-targeted therapies.
Diaphragmatic breathing - slow, deep breaths into your belly for 15 minutes after meals - can reduce symptoms by 35%. It’s simple. Free. And only 30% of people stick with it. But if you can make it a habit, it helps.
What’s Next for GERD Treatment?
The market for GERD treatments is growing. PPIs still make up 65% of sales, but newer drugs like vonoprazan are gaining ground. The FDA approved it for long-term use in May 2024. Sales are rising fast.The LINX device got approval in Europe for people with higher BMI (up to 40) in July 2024. That opens it up to more patients. Obesity rates in the U.S. are expected to hit 47% by 2030 - meaning more GERD cases ahead.
Doctors are also moving toward personalized care. No more blanket prescriptions. Your treatment should match your symptoms, your test results, and your goals. Some people want to avoid surgery at all costs. Others want to be free of pills. Your doctor should help you choose - not push one option.
The American College of Gastroenterology is updating its guidelines in late 2025. Expect more emphasis on non-acid reflux, dietary individualization, and early surgical options for the right candidates.
GERD isn’t something you just live with. You can take control. Start small. Track your habits. Talk to your doctor. And don’t be afraid to ask: Is this the best option for me - or just the easiest one to prescribe?







10 Comments
Aurelie L.
January 27, 2026 at 10:11
I tried elevating my bed and it changed everything. No more midnight coughing fits. Just blocks under the legs. No pillows. Don’t overthink it.
Joanna Domżalska
January 29, 2026 at 08:32
So basically you’re saying if you’re fat and smoke and eat pizza you deserve heartburn? Wow. Groundbreaking. Maybe the real issue is capitalism pushing processed food and doctors pushing pills instead of asking why we’re all so stressed out.
Faisal Mohamed
January 31, 2026 at 06:32
Bro this is peak pathophysiology 🤯 The LES is a biomechanical marvel - when you disrupt its tonic pressure via methylxanthines or gastric distension, you’re essentially bypassing the gastroesophageal barrier. But here’s the kicker - neurogenic hypersensitivity in the esophagus is the real MVP. PPIs? They’re just band-aids on a leaking dam. Vonoprazan? Now we’re talking pharmacodynamic superiority. 🧠🔥
Josh josh
February 2, 2026 at 01:51
just stopped eating late and now i dont need my pills anymore lol who knew right? also quit smoking like 2 months ago and my chest stopped feeling like a fire pit. thanks for the reminder guys
bella nash
February 3, 2026 at 14:28
It is of paramount importance to note that the temporal relationship between meal ingestion and recumbency must be rigorously maintained. Failure to observe this temporal constraint may result in the exacerbation of gastroesophageal reflux events, as evidenced by multiple randomized controlled trials.
SWAPNIL SIDAM
February 4, 2026 at 09:20
My uncle had GERD for 15 years. He tried everything. Then one day he just started breathing deep after meals. Like 10 breaths. No magic. Just calm. Now he eats spicy food and sleeps flat. No pills. God is good.
Geoff Miskinis
February 5, 2026 at 09:52
Let’s be honest - most of these ‘lifestyle changes’ are just advice for people who have the luxury of time, money, and emotional bandwidth. What about the single parent working two jobs who eats dinner at 9 p.m. because that’s when the kids are finally asleep? This article reads like a TED Talk for the comfortably sedentary.
Sally Dalton
February 5, 2026 at 20:46
i love this so much!! i started doing the diaphragmatic breathing thing and honestly it feels like my body finally relaxed for the first time in years?? also swapped soda for sparkling water and my nights are way better. thank you for writing this like a real human 😊
Betty Bomber
February 6, 2026 at 19:19
honestly the only thing that worked for me was just not eating pizza after midnight. no joke. no other changes. just stopped doing that one thing. weird right?
Mohammed Rizvi
February 8, 2026 at 02:12
You people are overcomplicating this like it’s rocket science. You eat junk, you lie down, you get burned. Simple. No magic. No $800 devices. Just stop being lazy and stop lying down after tacos. Your esophagus ain’t a circus act.