How to Keep a Symptom Diary for Suspected Drug Reactions
When you start a new medication, it’s normal to wonder: is this feeling caused by the drug, or is it something else? Dizziness after taking blood pressure pills? Nausea after a new antibiotic? A rash that shows up two days after starting a supplement? These aren’t just annoyances-they could be signs of a drug reaction. But without proof, doctors often dismiss them as stress, aging, or unrelated conditions. That’s where a symptom diary changes everything.
Why a Symptom Diary Matters
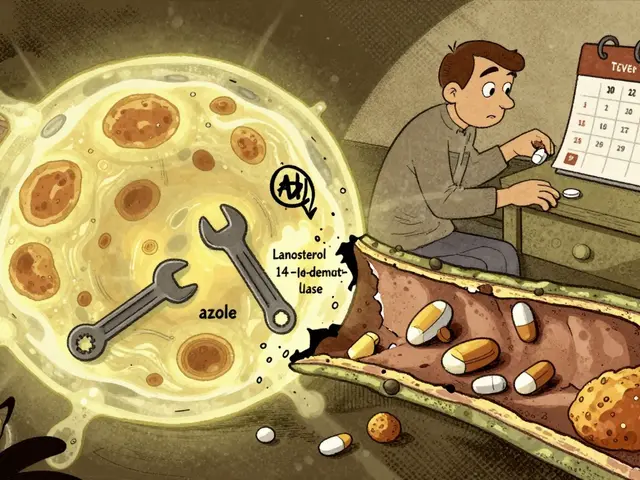
Most people rely on memory to explain how they feel after taking medicine. But memory is unreliable. A study from the National Institute on Aging found that after 48 hours, people forget up to 60% of symptom details. That’s why 62% of false drug reaction reports come from vague, delayed descriptions. A real symptom diary captures what happened, when, and how bad-before your brain tries to rewrite the story.It’s not just for emergencies. If you’re on multiple medications, supplements, or have chronic conditions like diabetes or arthritis, small changes in how you feel can add up. A diary helps you spot patterns. Maybe your headaches always hit 3 hours after taking your morning pill. Or your swelling flares after you eat lunch and take your diuretic. That’s not coincidence-that’s data.
Patients who kept detailed diaries before seeing specialists reduced unnecessary tests by 37%, according to La Roche-Posay’s clinical research. One Reddit user, u/MedTracker89, showed their neurologist a 14-day log linking levodopa doses to dizziness spikes. The doctor adjusted the dosage within 48 hours. That’s the power of clear, timed evidence.
What to Record: The 9 Essential Details
A useful symptom diary isn’t just a journal. It’s a structured record. The National Institute on Aging (NIA) and FDA require nine key data points for accurate analysis:- Date and time of medication intake-to the minute. Not "this morning." Not "around 8." Write: "March 12, 2025, 8:14 AM."
- Exact dosage and route-Was it 10 mg oral? 500 mg IV? Did you take half a pill? Write it down.
- All other medications and supplements-Even that fish oil, vitamin D, or herbal tea. Interactions matter.
- Symptom description-Be specific. "Headache" isn’t enough. Was it throbbing? On the right side? Did it feel like pressure behind the eyes?
- When the symptom started-Relative to the drug. "20 minutes after taking the pill" or "4 hours later."
- How long it lasted-Did it fade in 10 minutes? Last all day? Come and go?
- Environmental factors-Were you stressed? Hot? Sitting still? Exercising? Sleep-deprived? These affect how your body reacts.
- What you did to fix it-Did you lie down? Take ibuprofen? Drink water? Note it all.
- How it ended-Did it go away on its own? After medication? Did it leave any lingering effects?
For severity, use the Common Terminology Criteria for Adverse Events (CTCAE) scale. Grade 1 = mild, doesn’t interfere with daily life. Grade 2 = moderate, limits activity. Grade 3 = severe, needs medical help. Grade 4 = life-threatening. Grade 5 = death. You don’t need to be a doctor-just pick the best match.
Paper vs. Apps: Which Works Better?
You can use a notebook, a printable template, or a smartphone app. But here’s the truth: paper diaries get abandoned.Scripps Research found that 57% of people quit paper logs within 72 hours. Why? Too many boxes to fill. Too slow. Too easy to forget.
App-based diaries like Medisafe, CareClinic, and MyTherapy fix this. They:
- Auto-timestamp entries
- Send reminders to log symptoms
- Let you pick symptoms from preset lists (no typing needed)
- Generate charts showing when symptoms spike after taking a drug
- Export data as PDF to email to your doctor
Apps reduce abandonment to just 22%. And they’re FDA-compliant under 21 CFR Part 11 for use in clinical trials-meaning the data is trustworthy.
Still, some people prefer paper. If that’s you, get a pre-printed template with checkboxes for common symptoms: rash, nausea, dizziness, fatigue, swelling, confusion. Add a small space for notes. Keep it next to your pill organizer.
What Not to Document: Avoiding the Noise
Not every little change is a drug reaction. Some side effects are normal. Taking a new statin? Muscle soreness is common. Starting an SSRI? Nausea for the first week happens often.Dr. Michael Cohen from the Institute for Safe Medication Practices found that 41% of diaries were overloaded with expected side effects. This creates "noise"-and delays real help. A 2022 study showed these cluttered logs delayed intervention by over 3 days.
Focus on:
- Symptoms you’ve never had before
- Reactions that worsen over time
- Anything that stops you from doing normal things
- Symptoms that appear right after a new drug or dose change
Don’t log every tiny burp or mild headache unless it’s new, persistent, or severe. Be selective. Your doctor needs clarity, not a novel.
Visual Evidence: The Game-Changer for Skin Reactions
If you get a rash, hives, or skin discoloration after a drug, take a photo. Seriously.The European Medicines Agency found that adding photos to symptom diaries increased diagnostic accuracy for skin reactions by 78%. A description like "red spots on arms" is vague. A clear photo with a ruler or coin for scale? That’s diagnostic gold.
Even if you don’t think it’s serious, snap a picture. Skin reactions can escalate fast. And if you need to see a dermatologist, you’ll have proof. Don’t wait for it to get worse.
How to Make It Stick: Real Tips for Daily Use
Consistency is everything. Here’s how to make your diary part of your routine:- Sync with your phone-Set a daily alarm at the same time you take your meds. Use your phone’s health app to log meds and symptoms together.
- Keep your diary visible-Put your phone or notebook next to your pill box. Make it part of your morning or night ritual.
- Log within 15 minutes-For acute symptoms like swelling or trouble breathing, record immediately. Don’t wait.
- Review weekly-Every Sunday, look back. Are symptoms tied to specific drugs? Do they improve on weekends when you skip meds?
- Bring it to every appointment-Don’t wait for a crisis. Show your doctor your log during routine visits. It builds trust and opens the door to adjustments.
One trick: use your smartphone’s voice memo feature. Say: "March 12, 8:15 AM, took 25 mg lisinopril. Felt lightheaded 20 minutes later. Slight ringing in ears. Lying down helped after 15 minutes." Then transcribe it later. Less typing, more accuracy.

When to Seek Help: Red Flags in Your Diary
Your diary isn’t just for tracking-it’s a warning system. If you see these patterns, contact your doctor immediately:- Symptoms that start within minutes of taking a drug (possible anaphylaxis)
- Difficulty breathing, throat swelling, or wheezing
- High fever with rash
- Yellowing skin or eyes (liver issues)
- Severe abdominal pain or vomiting
- Unexplained bruising or bleeding
- Confusion, hallucinations, or seizures
These aren’t "maybe" reactions. They’re emergencies. Call 911 or go to the ER. Then, use your diary to tell them exactly what you took and when.
How Doctors Use Your Diary
Your diary doesn’t just help you-it helps your care team. Pharmacists use it to spot drug interactions. Neurologists use it to adjust dosages. Dermatologists use it to rule out allergies. The FDA now accepts patient-reported data directly in adverse event reports (since 2022), meaning your log could influence drug safety labels.In oncology, where drug reactions are common and dangerous, 92% of clinics require symptom diaries. In psychiatry, adoption is lower (48%) because cognitive issues make logging harder. But for everyone else? It’s becoming standard.
When you show your doctor a clean, timed log, they don’t just believe you-they trust you. And that leads to faster, smarter decisions.
What Happens Next: The Future of Symptom Tracking
The FDA is now testing systems that link your diary data directly to your electronic health record. If your app logs a spike in blood pressure after taking a new drug, the system could flag it automatically. Google Health’s Verily platform already predicts drug reactions with 89% accuracy using AI-though it’s not yet approved for clinical use.The NIH is funding a $4.7 million project to standardize symptom diaries across 150+ conditions by 2026. That means your log could soon work with any doctor, any hospital, anywhere in the U.S.
This isn’t science fiction. It’s the future of patient care-and you’re already part of it.
Do I need to log every single pill I take?
Yes-if it’s something you take regularly, even over-the-counter meds or supplements. Many drug reactions happen because of interactions. A common one is St. John’s Wort reducing the effect of birth control or antidepressants. Write down everything you consume, even if you think it’s harmless.
What if I forget to log a symptom?
Don’t guess. If you remember later, write "Recalled: March 10, 2025-felt dizzy after taking metformin, but didn’t log it at the time." Honesty matters more than perfection. Apps with reminders help prevent this.
Can I use my Apple Health or Google Fit app?
You can track meds and symptoms in them, but they’re not designed for detailed adverse event logging. Use a dedicated app like CareClinic or MyTherapy-they include the exact fields doctors need. You can still sync data from Apple Health to those apps for convenience.
How long should I keep the diary?
At least 2-4 weeks after starting a new drug or changing a dose. For chronic conditions or ongoing reactions, keep going. Some reactions only show up after months. Your doctor might ask for 30, 60, or even 90 days of data.
Will my doctor think I’m overreacting if I log every little thing?
No-if you’re selective. Focus on new, unusual, or worsening symptoms. Avoid logging expected side effects like mild nausea on day 2 of an antibiotic. Your doctor wants to see patterns, not noise. If you’re unsure, ask: "Is this something I’ve never felt before?" If yes, log it.





14 Comments
Deborah Jacobs
December 6, 2025 at 07:04
I started keeping a symptom diary after my weird dizziness with that new blood pressure med. At first I thought I was being dramatic, but after two weeks I saw the pattern-every time I took it with coffee, I felt like I was going to pass out. My doctor was skeptical until I showed her the log. Now I’m on a different dose and I haven’t felt off in months. It’s not just about tracking-it’s about reclaiming your body when no one else believes you.
Also, use the voice memo trick. I do it while brushing my teeth. Saves so much typing and feels way more natural.
Lucy Kavanagh
December 7, 2025 at 01:07
Did you know the FDA is secretly using these diaries to track people’s private health data and sell it to Big Pharma? They’ve been doing it since 2019. That’s why they pushed apps so hard-so they can auto-sync everything into their databases. I saw a whistleblower video on TruthFeed. They’re building a national health surveillance network under the guise of ‘patient empowerment.’
Don’t use any app. Write it on paper. Burn it after 30 days. Trust no one.
Stephanie Fiero
December 7, 2025 at 03:32
OMG YES THIS. I was so done with doctors telling me it was ‘just anxiety’ until I started logging. I forgot to log one day and my headache came back worse than ever-turns out it was the new fish oil. I’m not even kidding. I’ve been using CareClinic and it’s a lifesaver. I even set a reminder to log my period because my migraines sync with it. You’re not overreacting-you’re being smart.
Also, don’t listen to people who say ‘it’s not that bad.’ If it’s new, log it. Even if it’s just a weird burp. You never know.
Jennifer Patrician
December 8, 2025 at 03:32
Why are we letting corporations dictate how we track our own health? Apps like MyTherapy? Owned by a German conglomerate that’s tied to Bayer. They want you to log everything so they can tweak drug dosages in real time and profit off your suffering. And don’t get me started on the ‘FDA-compliant’ nonsense-that just means they passed a paperwork test, not that your data is safe.
Use a notebook. Handwrite it. Hide it. Burn it. If you’re not paranoid, you’re not paying attention.
Ali Bradshaw
December 8, 2025 at 05:29
This is actually really well put. I’ve been logging my meds for three years now since my autoimmune flares started. It’s not glamorous, but it’s saved me from three unnecessary hospital trips. I used to think I was just ‘being dramatic,’ but the data doesn’t lie.
My tip? Use a simple Google Sheet. Free, no ads, no tracking. I just jot it down on my phone when I remember. No fancy app needed. Consistency > perfection.
Annie Grajewski
December 8, 2025 at 09:01
Wow. So we’re supposed to be little data points for Big Pharma now? Cute. You know what’s *really* dangerous? Thinking that writing down your headache makes you an empowered patient. Meanwhile, your doctor’s still on a 7-minute visit and hasn’t read your diary because they’re too busy chasing KPIs.
Also, ‘CTCAE scale’? Sounds like something the military uses to classify how much pain you’re allowed to feel before they stop caring. Grade 1 = mild, doesn’t interfere with daily life. Translation: suck it up, Karen.
Rupa DasGupta
December 9, 2025 at 22:47
I tried this for a week and cried every night 😭 I felt so alone. My doctor laughed when I showed her my log. Said I was ‘overthinking.’ But I knew. I knew the rash was from the supplement. I just didn’t have the words. Now I use voice notes and cry while recording. It helps. Maybe I’m broken. Maybe I’m not. But at least I have proof.
Thank you for this. I’m not crazy. I’m just tired.
Marvin Gordon
December 10, 2025 at 20:05
One thing no one talks about: the emotional toll of keeping a diary. It’s not just logging symptoms-it’s reliving them every time you write them down. I used to feel like I was drowning in my own body.
But after 6 months, I started noticing things I couldn’t before-like how my fatigue spiked only when I took meds after 7 PM. That’s not coincidence. That’s insight. Don’t underestimate the power of small, consistent truths.
Michael Dioso
December 11, 2025 at 12:03
App? Paper? Who cares. The real issue is that doctors don’t want to hear it. They’re trained to dismiss patients, especially women, especially older ones. Your diary won’t change that. It’ll just give you more proof that you’re being gaslit.
Also, ‘FDA-compliant’? LOL. That’s just corporate jargon for ‘we paid the fee.’ Your data is not safe. Your doctor doesn’t care. Your log is just noise until you find the one who listens. Good luck with that.
Krishan Patel
December 11, 2025 at 21:18
It is imperative that individuals assume full responsibility for their physiological responses to pharmacological agents. To delegate diagnostic authority to pharmaceutical corporations or algorithmic platforms is to surrender autonomy. The symptom diary, when maintained with rigorous epistemological discipline, becomes an act of ontological resistance against institutional epistemic violence.
Furthermore, the use of voice memos is an abdication of linguistic precision. If you cannot articulate your experience in clear, grammatically correct prose, you have no right to expect your suffering to be taken seriously.
sean whitfield
December 13, 2025 at 03:54
They want you to log everything. That’s the point. So they can sell it. So they can predict you. So they can tell you what you’re feeling before you even feel it. You think this is about health? Nah. It’s about control. You’re not a patient. You’re a dataset.
Put down the phone. Go outside. Breathe. The pills will still be there tomorrow.
Mellissa Landrum
December 14, 2025 at 19:49
US government is using these logs to flag ‘high-risk’ citizens for future surveillance. I read it on a forum. They’re building a health-based social credit system. You think your diary is private? It’s synced to your Medicare ID. Your ‘mild headache’? That’s now a ‘potential neurological risk factor.’ Don’t be naive. They’re watching.
Mark Curry
December 16, 2025 at 08:10
I started this after my dad’s hospital stay. He didn’t know what meds he was on. No one could figure out why he was confused. We found a pill bottle in the drawer with no label. He’d been taking two different blood pressure pills at once. His log was a mess-but it was honest.
It saved his life. Not because it was perfect. Because it was real.
Just write it down. Even if it’s ugly.
an mo
December 17, 2025 at 09:21
Let’s deconstruct the underlying epistemic hegemony of the symptom diary paradigm. The entire framework assumes a Cartesian dichotomy between patient and provider, where subjective experience is quantified to conform to biomedical hegemony. The CTCAE scale? A tool of normalization. The app? A digital panopticon.
Meanwhile, structural determinants-poverty, food deserts, environmental toxins-are ignored. You’re being asked to fix a broken system by becoming a better data point. That’s not empowerment. That’s neoliberal co-optation.