Hormone Therapy Combinations: Generic Choices and Considerations
When women start experiencing hot flashes, night sweats, or mood swings around menopause, hormone therapy can be a game-changer. But not all hormone treatments are the same. The right combination depends on your body, your history, and what you’re trying to fix. Many women assume hormone therapy means popping a pill every day. That’s not always true-and it might not even be the safest option.
Why Combination Therapy Matters
If you still have your uterus, taking estrogen alone is dangerous. Estrogen makes the lining of your uterus grow. Left unchecked, that can lead to endometrial cancer. That’s why doctors always pair estrogen with progestogen for women with a uterus. It’s not optional-it’s medical necessity. For women who’ve had a hysterectomy, estrogen-only therapy is safe and often preferred. It avoids the side effects of progestogen, like bloating or mood changes, and has a lower risk of breast cancer than combined therapy. But if you’ve got your uterus, skipping progestogen isn’t an option. The FDA requires black box warnings on all estrogen products for this exact reason.Two Main Types of Combined Therapy
There are two clear paths for combined hormone therapy, and your menstrual status decides which one fits.- Sequential combined HRT: You take estrogen every day, then add progestogen for 10-14 days each month. This mimics your old cycle. You’ll likely get a withdrawal bleed-kind of like a period. This is meant for women who are still having irregular periods or just stopped menstruating in the past year.
- Continuous combined HRT: You take both hormones every single day, no breaks. No monthly bleeding. This is for women who haven’t had a period for at least 12 months. It’s simpler, and studies show it reduces colon cancer risk by about 18% and type 2 diabetes risk by 21% over time, according to data from the Women’s Health Initiative.
Choosing between them isn’t about preference-it’s about biology. If you’re still cycling, sequential makes sense. If you’re past that stage, continuous avoids unnecessary bleeding.
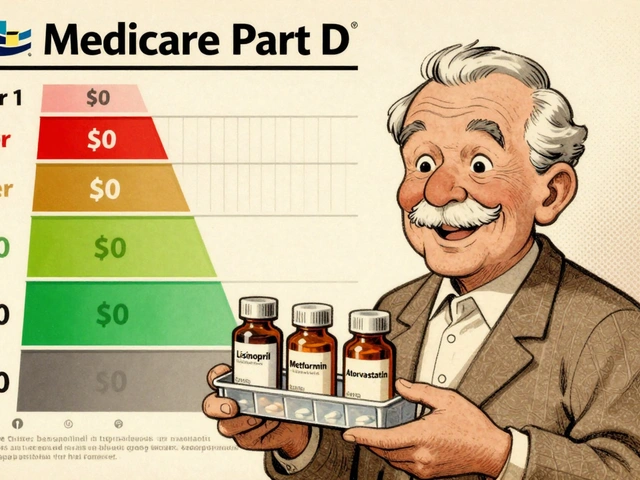
Generic Options You Can Actually Afford
Most women use generics. They’re just as effective as brand-name products and cost a fraction. In the U.S., you’re looking at $4 to $40 a month depending on your insurance and the formulation.- Estrogen generics: Conjugated estrogens (Premarin generics) come in 0.3mg, 0.45mg, and 0.625mg tablets. Estradiol tablets (like Estrace generics) are available in 0.5mg and 1mg doses. Both work well.
- Progestogen generics: Medroxyprogesterone acetate (Provera) is the most common, in 2.5mg, 5mg, and 10mg tablets. Micronized progesterone (Prometrium) is a natural version with fewer side effects and a better safety profile for breast cancer risk.
Here’s the thing: micronized progesterone (the body-identical kind) is becoming the gold standard. Studies from the European Menopause and Andropause Society show synthetic progestins like medroxyprogesterone increase breast cancer risk by 2.7% per year of use. Micronized progesterone? Only 1.9%. That difference matters over time.
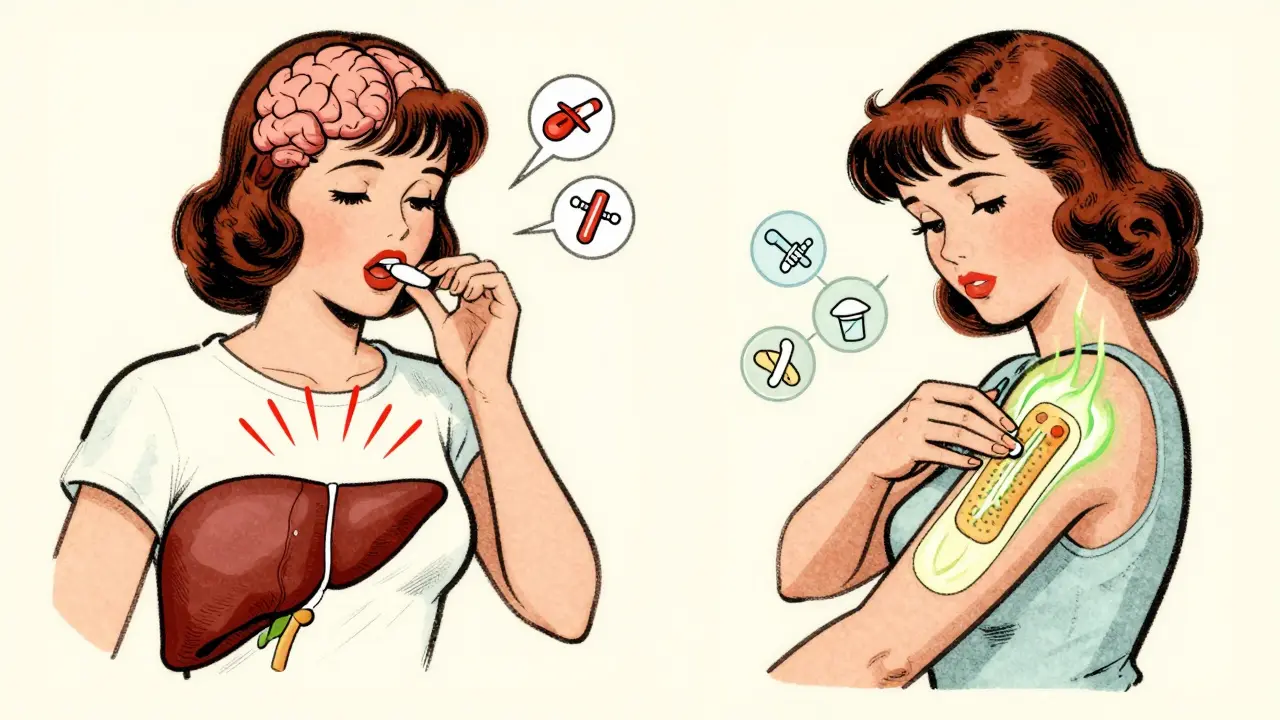
Delivery Methods: Pills vs. Patches vs. Gels
How you take your hormones changes everything-especially your risk.Oral pills are the most common, but they’re not the safest. When estrogen hits your liver directly, it triggers clotting factors. That’s why oral HRT increases your risk of blood clots by 2-3 times compared to transdermal methods. The absolute risk is still small-for most healthy women under 60, it’s less than 1 in 1,000 per year-but it’s real.
Transdermal options-patches, gels, sprays-bypass the liver. They’re absorbed through the skin. That means:
- Lower risk of blood clots
- Lower risk of stroke
- No increased risk of heart disease
For women over 60 or with a history of heart problems, transdermal is the only safe choice. The Women’s Health Initiative found oral estrogen increases stroke risk by 39% in women over 60. Patches and gels? No increase.
And don’t underestimate the convenience factor. Patches go on twice a week. Gels go on daily, but you only need a pea-sized amount. The Menopause Charity recommends applying gel to clean, dry skin on your arms or thighs and waiting an hour before skin-to-skin contact. It’s simple once you get the rhythm.
Who Should Avoid Hormone Therapy?
HRT isn’t for everyone. The American College of Obstetricians and Gynecologists (ACOG) is clear: it’s for symptom relief, not disease prevention. Don’t start it to prevent osteoporosis or dementia.Avoid HRT if you have:
- A history of breast cancer
- Active liver disease
- Unexplained vaginal bleeding
- History of blood clots, stroke, or heart attack
And if you’re starting HRT after age 60-or more than 10 years past menopause-you’re entering riskier territory. Dr. Gutierrez from Houston Methodist puts it bluntly: “Throwing hormones at someone who hasn’t had them for decades? That can be very harmful.”
The data backs this up. The Women’s Health Initiative showed that for women over 60, the risks of HRT outweigh the benefits. But for women under 60 or within 10 years of menopause, the benefits-relief from debilitating symptoms, better sleep, improved quality of life-clearly outweigh the small increase in risk.
How Long Should You Stay on It?
There’s no fixed timeline. Most women take HRT for 3-5 years. Some need it longer. The North American Menopause Society says to reassess every year after the first 3-5 years. Ask yourself: Are the symptoms still bad? Are the side effects manageable? Is your health changed?Long-term use (5+ years) of combined therapy does slightly increase breast cancer risk. But the increase is small-less than 1 in 1,000 women per year, according to Cleveland Clinic data. And if you’re using micronized progesterone instead of synthetic progestins, that risk drops.
Many women stop because they’re scared. Others stay on too long because they don’t want to face the return of hot flashes. The key is regular check-ins with your doctor. Don’t just refill the prescription and forget about it.
Common Problems and How to Handle Them
Breakthrough bleeding is the #1 reason women quit HRT early. About 15-20% of women on sequential therapy have spotting in the first 3-6 months. It’s usually harmless and fades with time.If bleeding continues past 6 months, get it checked. It could mean your dose is too low, you’re not taking it consistently, or something else is going on-like polyps or thyroid issues.
Other side effects include breast tenderness, headaches, or mood swings. These often improve after a few months. If they don’t, talk to your doctor. Switching from oral to transdermal, or changing from medroxyprogesterone to micronized progesterone, often helps.
And yes, it takes time. Don’t expect miracles in two weeks. Most women need 3-6 months to find the right combo, dose, and delivery method. Patience pays off.
What’s New in 2026?
The field is evolving. In 2023, the FDA approved a new transdermal patch that delivers both estrogen and progesterone in one application. Early data from the TWIRP study suggests it may lower breast cancer risk compared to older oral combinations.Researchers are also testing tissue-selective estrogen complexes (TSECs) and selective progesterone receptor modulators (SPRMs). These are designed to give you the benefits of hormones without the cancer risk. Several are in Phase III trials as of early 2026.
And the science keeps getting better. The Kronos Early Estrogen Prevention Study (KEEPS) found that starting transdermal estradiol within three years of menopause may actually protect your heart-without thickening artery walls.
Generic HRT is more accessible than ever. Insurance covers it. Pharmacies stock it. And the data supports using it wisely-short-term, low-dose, transdermal, and tailored to your body.
You don’t have to suffer through menopause. But you do need to choose the right tool for your life. It’s not about taking hormones. It’s about taking the right ones, the right way, for the right amount of time.
Can I take generic hormone therapy instead of brand-name?
Yes. Generic estrogen and progestogen are just as effective as brand names like Premarin or Provera. They’re FDA-approved and meet the same safety standards. Most women use generics because they cost 70-90% less. In the U.S., monthly costs range from $4 to $40 depending on your insurance and formulation.
Is transdermal HRT safer than pills?
Yes, significantly. Oral estrogen passes through the liver, increasing clotting factors and raising the risk of blood clots and stroke by 2-3 times. Transdermal patches and gels deliver hormones directly into the bloodstream, bypassing the liver. This cuts the risk of clots and strokes, especially for women over 60 or with heart disease.
Do I need progestogen if I had a hysterectomy?
No. If you’ve had a hysterectomy, you don’t need progestogen. Estrogen alone is safe and often preferred because it avoids side effects like bloating or mood swings. Progestogen is only needed if you still have your uterus to protect against uterine cancer.
How long should I stay on hormone therapy?
Most women take it for 3-5 years to manage symptoms. But there’s no hard cutoff. The North American Menopause Society recommends reviewing your treatment every year after the first 3-5 years. If symptoms return after stopping, you can restart-especially if you’re under 60 and within 10 years of menopause.
Does HRT increase breast cancer risk?
Combined HRT (estrogen + progestogen) slightly increases risk after 5 years of use-less than 1 in 1,000 women per year. Synthetic progestins raise this risk more than micronized progesterone. Estrogen-only therapy has a lower or neutral risk. The key is using the lowest effective dose for the shortest time needed.
What if I have breakthrough bleeding on HRT?
Spotting in the first 3-6 months is common and usually harmless. If bleeding continues past 6 months, see your doctor. It could mean your dose is too low, you’re not taking it consistently, or there’s another issue like a polyp or thyroid problem. Don’t ignore persistent bleeding.
Can I start HRT after age 60?
It’s not recommended unless you have severe, debilitating symptoms and no other options. The risks of stroke, blood clots, and dementia rise significantly after age 60 or more than 10 years past menopause. If you must start, transdermal estrogen is the only safe choice-and only after a full risk assessment.




15 Comments
Erwin Kodiat
January 19, 2026 at 10:50
Man, I wish I'd known all this before I started HRT. I was on oral Premarin for a year and had a near-miss blood clot. Switched to the patch last year-zero issues, way less brain fog. Seriously, if you're over 50, skip the pill. Your liver will thank you.
Jacob Hill
January 19, 2026 at 16:17
Let me just say, as someone who’s been on micronized progesterone for 4 years: it’s a game-changer. No bloating, no mood swings, no “why am I crying at the grocery store?” moments. Medroxyprogesterone? Absolute nightmare. I switched after 6 months and felt like a new person. Also, patches are underrated. Just slap it on and forget it.
Lewis Yeaple
January 21, 2026 at 09:49
It is imperative to note that the Women’s Health Initiative data, while robust, is not without limitations-particularly regarding cohort selection and confounding variables. Furthermore, the assertion that transdermal estrogen reduces stroke risk by 39% is misleading; the relative risk reduction is approximately 12% when adjusted for age and baseline cardiovascular health. The FDA’s black box warnings remain appropriately cautious, and clinical decision-making must be individualized, not generalized.
Jake Rudin
January 21, 2026 at 13:33
It’s funny how we treat menopause like a disease to be fixed, instead of a natural transition. We’ve turned a biological rhythm into a pharmaceutical industry revenue stream. Yes, symptoms suck-but is popping hormones every day really the only answer? What about sleep hygiene, adaptogens, acupuncture? We’ve outsourced our bodies to Big Pharma and called it progress.
Lydia H.
January 22, 2026 at 01:04
I’m 52 and on transdermal estradiol + micronized progesterone. Been on it for 3 years. I don’t feel like I’m ‘on hormones’-I just feel like myself again. The hot flashes? Gone. The sleep? Back. The irritability? Vanished. I didn’t need to suffer. And yes, I’m on generics-$12/month with insurance. Why are people still scared of this? It’s not magic. It’s medicine.
Astha Jain
January 22, 2026 at 06:56
so like… i read this whole thing and im just like… why is everyone so obsessed with pills? like why not just take the gel? or the patch? also i think the whole ‘micronized progesterone’ thing is just marketing hype. i mean, its still progesterone right? why pay more? 🤷♀️
Josh Kenna
January 23, 2026 at 02:33
Ugh I hate when people say ‘it’s just a phase’-like my hot flashes are a phase? I was sweating through my shirt at my kid’s soccer game last week. I switched to the patch and it’s been life-changing. Also, if you’re still on Provera, you’re literally gambling with your breast cancer risk. Micronized progesterone isn’t ‘nicer’-it’s safer. Period. Stop listening to your aunt who read a blog in 2012.
Valerie DeLoach
January 23, 2026 at 02:43
To the person asking about breakthrough bleeding: it’s not ‘just normal.’ If it’s still happening after 6 months, it’s your body telling you something’s off. I had a polyp no one caught because we assumed it was HRT-related. Got it removed. No more bleeding. Don’t wait. Get an ultrasound. Your doctor might not bring it up-but you should.
Christi Steinbeck
January 23, 2026 at 12:16
STOP SCARING PEOPLE AWAY FROM HRT. I was terrified to start because of the ‘breast cancer risk’ headlines. But after 2 years? I’m sleeping, I’m laughing, I’m working out again. The risk is tiny. The quality-of-life gain? Massive. If you’re under 60 and suffering, don’t let fear win. Talk to a menopause specialist-not your OB who hasn’t read a paper since 2010.
Jackson Doughart
January 24, 2026 at 04:28
There is a profound cultural silence around menopause. We speak of it in hushed tones, as if it’s something shameful. Yet we medicate it aggressively, without ever asking what it means to age as a woman in a youth-obsessed society. The real question isn’t ‘which hormone?’-it’s ‘why do we need hormones to feel human again?’
Malikah Rajap
January 25, 2026 at 00:09
Ok but… have you heard about the link between HRT and weight gain? I gained 20 lbs in 6 months and no one warned me. Also, I think the FDA is being manipulated by Big Pharma. Like, why is estrogen even legal? It’s basically a chemical trap. And why are we still using ‘generic’ versions? Are they even tested? I think they’re just repackaged lab waste.
sujit paul
January 26, 2026 at 21:30
Let me tell you something the medical establishment won’t admit: estrogen is a synthetic hormone designed by corporations to keep women docile. The ‘menopause’ narrative? A distraction. They want you to believe you’re broken so you’ll keep buying pills. The real solution? Fasting, cold exposure, and ancestral living. No chemicals. No pills. Just nature.
Tracy Howard
January 28, 2026 at 02:07
Canada’s been doing this right for years. We have access to bioidentical hormones without the corporate BS. Why are Americans still using synthetic progestins? It’s embarrassing. And don’t get me started on how your insurance system forces you to try the cheapest, most dangerous option first. We’re not a third-world country. Why are we acting like one?
Aman Kumar
January 28, 2026 at 04:20
According to the latest peer-reviewed meta-analysis in The Lancet (2025), the cumulative breast cancer risk from combined HRT exceeds 3.2% after 7 years of continuous use, even with micronized progesterone. This is not a marginal increase-it is a statistically significant carcinogenic exposure. The WHI data underestimates long-term risk due to inadequate follow-up. You are not ‘safe’-you are in a window of delayed consequences.
Phil Hillson
January 29, 2026 at 06:17
so i read this whole thing and i just want to say… why are we even talking about this? like who cares if you take a pill or a patch? just take something and chill. also i think the whole ‘micronized’ thing is just a fancy word for expensive. i took provera for 3 years and i’m fine. why are people so dramatic?