Global Contraception Access & Affordability: Facts, Challenges, and Solutions
Contraception Affordability Calculator
Calculate Your Contraception Affordability
See how much a contraception method costs relative to your monthly income. Based on WHO standards, a method is considered affordable if it costs less than 2-5% of household income.
Affordability Results
$0.00
0.0%
Global Context:
- Low-income countries: Average cost is 2-5% of income
- High-income countries: Average cost is 1-3% of income
- Affordable threshold: Below 2.5% of income
When you hear the phrase Contraception is a set of methods that prevent pregnancy and allow individuals to plan if and when they have children, it sounds simple. In reality, getting the right method at a price you can afford is a daily struggle for millions of people worldwide. This article breaks down the biggest gaps, the numbers that matter, and what’s actually working to close the divide.
Why Contraception Matters Beyond Birth Control
Access to reliable contraception does more than stop an unwanted pregnancy. It improves maternal health, boosts girls’ school attendance, and lifts entire economies. The World Bank estimates that every $1 spent on modern contraceptives returns $4 in health and development savings. Countries with higher Family Planning coverage see lower infant mortality rates and higher female labor force participation.
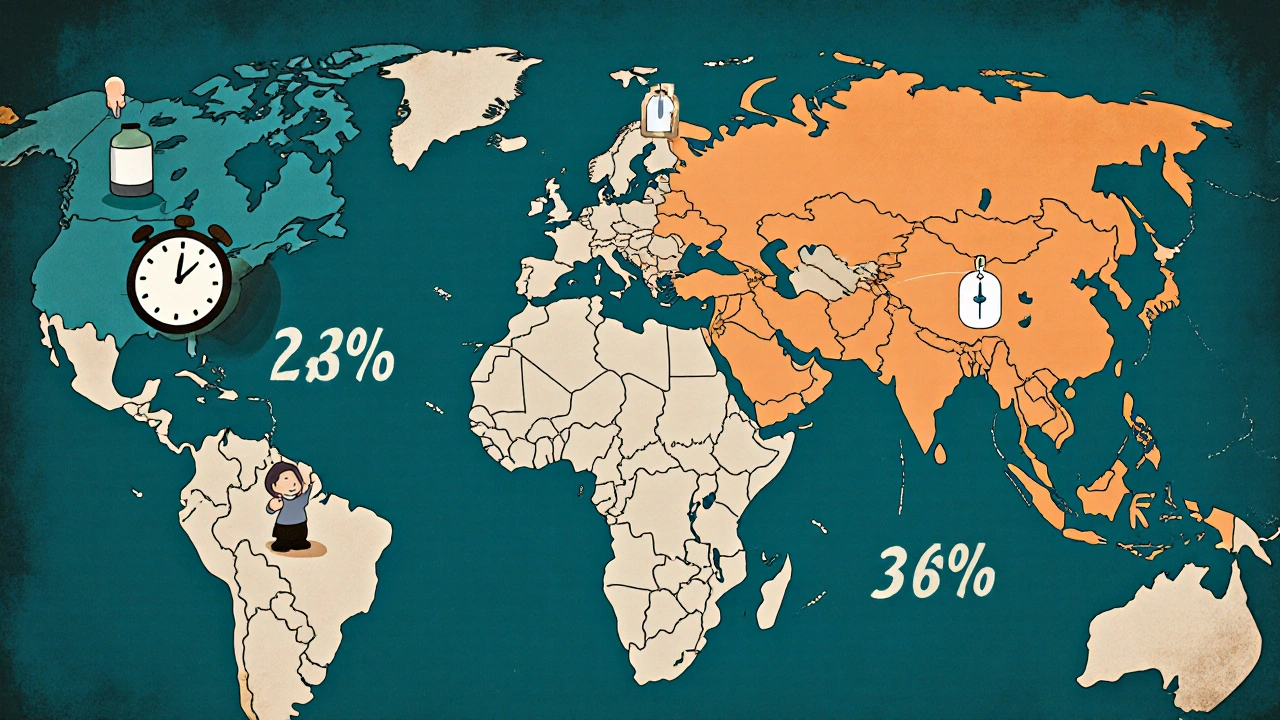
Global Snapshot: Who Has Access and Who Doesn’t?
According to the United Nations Population Fund (UNFPA) and the World Health Organization (WHO), about 63% of women of reproductive age use some form of modern contraception. Yet the picture splits sharply by income level:
- High‑income nations: 82% coverage, with most users opting for long‑acting reversible contraceptives (LARCs) or pills.
- Upper‑middle‑income nations: 66% coverage, but large gaps in rural areas.
- Low‑income nations: only 38% coverage, and many rely on less effective methods like condoms or traditional practices.
These numbers hide the fact that in sub‑Saharan Africa, less than a quarter of women can obtain their preferred method within a 2‑hour travel window.
Affordability: The Hidden Cost of Choice
Even when a method is physically available, price can block use. In many low‑and‑middle‑income countries, a month’s supply of oral contraceptives costs 2-5% of a household’s average monthly income. In the United States, uninsured women pay an average of $30-$50 per month for the pill, while Medicaid beneficiaries often get it for free.
Key affordability drivers include:
- Out‑of‑pocket fees: Direct payments at pharmacies or clinics.
- Insurance coverage gaps: Private plans may exclude certain methods, and public programs vary by state.
- Supply‑chain inefficiencies: Shipping delays inflate prices, especially for LARCs that require professional insertion.
Barriers Beyond Price
Money is only one piece of the puzzle. Cultural norms, restrictive policies, and weak health systems also limit access:
- Policy restrictions: Some countries require spousal consent or limit provision to physicians only.
- Cultural stigma: In many communities, using contraception is viewed as promoting promiscuity.
- Healthcare workforce shortages: Without trained providers, even cheap methods like the pill remain out of reach.
When you combine these factors, the odds of a woman obtaining her preferred method drop dramatically.
What’s Working? Proven Strategies to Boost Access and Affordability
Evidence from the Guttmacher Institute, UNFPA, and multiple ministries of health shows that a mix of policy, financing, and service delivery changes can move the needle.
| Intervention | Key Actions | Typical Cost Savings |
|---|---|---|
| Publicly funded LARC programs | Government covers device and insertion; task‑shifting to nurses | Up to 70% reduction in unintended pregnancies per 1,000 women |
| Managed‑by‑pharmacy emergency contraception kits | Over‑the‑counter availability, price caps | 30% lower out‑of‑pocket cost compared to clinic dispensation |
| Telehealth prescribing of oral contraceptives | Remote consultation, mailed prescriptions | Average $12 saved per patient per year |
| Conditional cash transfers for family planning | Small stipend for each documented LARC uptake | Improves uptake by 18% in targeted regions |
These approaches cut both direct costs and indirect barriers, like travel time or stigma.
Case Studies: Lessons from the Field
Rwanda’s community health worker model - By training CHWs to distribute pills and condoms, Rwanda lifted contraceptive prevalence from 27% in 2005 to 58% in 2022, while keeping user fees below $1 per month.
Sweden’s universal coverage - All residents receive free contraception through the national health system. Result: one of the lowest teen pregnancy rates in Europe (4 per 1,000 women).
U.S. Medicaid expansion - States that expanded Medicaid saw a 7% rise in LARC uptake and a 4% drop in uninsured pregnancies within three years.
India’s subsidized IUD program - Central subsidies lowered the price of copper IUDs to under $2, leading to a 12% increase in rural uptake.

Checklist for Policymakers and Advocates
- Identify the most used methods in your region and target price reductions on those.
- Remove legal barriers: allow pharmacists and nurses to provide a broader range of methods.
- Invest in supply‑chain transparency to prevent stock‑outs.
- Integrate contraception services with maternal‑child health visits.
- Use data dashboards (e.g., WHO’s contraceptive commodity tracker) to monitor coverage gaps.
Following this list can turn vague commitments into measurable progress.
Future Outlook: What to Watch in the Next Five Years
Three trends are poised to reshape global contraception access:
- Digital health platforms: Apps that order pills or schedule LARC insertions are expanding in low‑resource settings.
- Male‑focused methods: New hormonal gels and injectables could share the burden of access.
- Climate‑smart supply chains: Renewable‑energy‑powered cold storage aims to keep temperature‑sensitive methods viable in remote areas.
Keeping an eye on these developments helps stakeholders act before gaps widen.
Key Takeaway
Improving contraception access isn’t just about handing out pills-it’s about aligning policy, financing, and service delivery so that every person can choose a method that fits their life and budget. When countries invest in affordable, stigma‑free options, they unlock health, education, and economic gains for entire societies.
What is the difference between short‑acting and long‑acting contraceptives?
Short‑acting methods (like pills, patches, or condoms) require daily or per‑use action. Long‑acting reversible contraceptives (LARCs) such as IUDs and implants work for years after a single insertion, needing only occasional check‑ups.
How much does a typical birth‑control pill cost in low‑income countries?
Average prices range from $0.30 to $0.70 per month, often subsidized by NGOs or government programs. Out‑of‑pocket costs can still be a barrier for the poorest households.
Can teenagers access contraception without parental consent?
Laws vary worldwide. In many European countries, minors can obtain contraception confidentially. In contrast, several Asian and African nations require parental or spousal approval, limiting teen access.
What role do NGOs play in improving affordability?
Organizations like the Guttmacher Institute and UNFPA fund bulk purchases, negotiate price reductions, and run community education campaigns that lower both cost and stigma.
Is emergency contraception a reliable backup?
When taken within 72 hours of unprotected sex, emergency contraception reduces the chance of pregnancy by 75% to 89%, making it a crucial safety net where regular access is limited.




9 Comments
Ritik Chaurasia
October 22, 2025 at 12:46
India still watches the global numbers while millions of women trek hours to the nearest clinic for a single pill. The government’s budget talks often skip the real cost of a condom or an IUD for a rural family. When a month’s supply eats up 4% of a household income, you can bet they’ll cut corners elsewhere. It’s not just about money – cultural taboos still label contraception as taboo, driving women underground. We need bold policy swaps, task‑shifting to community health workers, and price caps that actually hit the shelves.
Mary Keenan
October 22, 2025 at 14:10
This reads like a glossy brochure.
Ben Collins
October 22, 2025 at 15:33
Wow, what a roller‑coaster of stats and solutions – buckle up, folks.
First off, the numbers are impressive, but they hide the daily grind of women who can’t even find a pharmacy that carries the right method. Second, the claim that $1 returns $4 is great advertising, yet it glosses over the bureaucratic bottlenecks that choke funding before it reaches a clinic. Third, the LARC programs sound like a miracle, but you still need trained hands, and many low‑income regions lack even a single qualified inserter.
Fourth, let’s talk about the cultural stigma that makes a teenager’s choice feel like a crime. Fifth, the supply‑chain jokes about “shipping delays” ignore the fact that temperature‑sensitive products often spoil before they hit remote villages.
Sixth, telehealth sounds futuristic, but without reliable internet it’s just a pipe dream for the very people who need it most. Seventh, cash transfers are a neat trick, yet they risk turning reproductive health into a transaction rather than a right.
Eighth, the case studies – Rwanda, Sweden, the U.S., India – each shine a light on different facets, but none solve the whole puzzle. Ninth, the digital health platforms might reorder pills, but who’s watching for data privacy breaches?
Tenth, male‑focused methods could balance the load, but they’re still in the research phase, so let’s not count on them as a silver bullet. Eleventh, climate‑smart supply chains sound eco‑friendly, but they add another layer of cost that low‑budget ministries can’t always afford.
Twelfth, the checklist is handy, but if policymakers treat it like a tick‑box exercise, we’ll see the same half‑measures. Thirteenth, the future outlook reads like a tech brochure; it’s hopeful, but hope isn’t a policy.
Fourteenth, let’s give a nod to NGOs – they’re the quiet engines pushing bulk purchases and education, though they’re often under‑funded themselves.
Finally, the core truth remains: we need coordinated policy, financing, and on‑the‑ground delivery that respects people’s choices, not just charts and tables. Until that happens, all the numbers in the world won’t change the fact that many still can’t get the method they need.
Denver Bright
October 22, 2025 at 16:23
Interesting points raised above, especially about telehealth and supply chains. It’s true that without reliable internet, many of those solutions stay theoretical. Still, incremental steps like training more nurses could bridge the gap sooner.
cariletta jones
October 22, 2025 at 18:20
Great overview! It’s encouraging to see real‑world examples where small policy tweaks made a huge difference. Keep spreading the optimism – every bit helps.
Kevin Hylant
October 22, 2025 at 19:43
The data is clear: price matters a lot. If a month’s pills cost a big part of a family’s budget, they’ll look for cheaper ways or skip birth control entirely. Simple subsidies can change that.
Holly Green
October 22, 2025 at 20:33
While subsidies help, we also need to tackle the stigma that stops people from even asking for help. A respectful, confidential service goes a long way.
Jonathan Harmeling
October 22, 2025 at 22:30
Reading through the strategies, I’m struck by how colorful the solutions can be – from cash incentives to digital apps. Yet the common thread is clear: empower local providers and cut the red tape.
Gary Marks
October 22, 2025 at 23:53
Honestly, the article feels like a parade of buzzwords without enough gritty detail. We need more than “task‑shifting” and “climate‑smart” – we need concrete budgets, real timelines, and accountability. Otherwise, the promises stay just that – promises. The relentless optimism is nice, but it can mask the brutal reality on the ground where women juggle work, childcare, and now a nonexistent supply chain. Let’s cut the fluff and focus on what actually moves the needle.