Postpartum Anxiety: Recognizing Symptoms, Screening Tools, and Effective Care Paths
One in five new mothers experiences postpartum anxiety - not just stress, not just tiredness, but a deep, persistent wave of fear that doesn’t fade with sleep or time. It’s not the baby blues. It’s not normal. And too often, it goes undiagnosed for weeks or even months because it’s mistaken for just being a "new mom." But when anxiety takes over - racing heart, sleepless nights even when the baby is sleeping, panic attacks, or intrusive thoughts about harm coming to your child - it’s time to recognize it for what it is: a treatable medical condition.
What Postpartum Anxiety Really Feels Like
Postpartum anxiety isn’t just worrying about whether you’re doing enough. It’s the kind of worry that makes your chest tighten, your hands shake, and your mind race even when everything seems fine. You might find yourself checking the baby’s breathing every five minutes, convinced something terrible is about to happen. Or you might feel overwhelming guilt that you’re not enjoying motherhood the way you "should." Physical symptoms are common and often misleading. Sixty-two percent of women report a racing heart. Nearly half experience nausea. About four in ten lose their appetite. These aren’t signs of a physical illness - they’re signs of anxiety. Panic attacks occur in 28 to 35% of cases, sometimes without warning. You might feel like you’re having a heart attack, but there’s no cardiac issue. It’s your nervous system stuck in overdrive. Unlike the baby blues - which affect 70 to 80% of new mothers and fade within two weeks - postpartum anxiety lasts longer than 14 days and often gets worse. It doesn’t improve with rest. It doesn’t go away when someone else takes the baby for an hour. It lingers, and it interferes with bonding, feeding, and even basic self-care.How It’s Different From Postpartum Depression
Many assume postpartum anxiety is just depression with extra worry. But they’re not the same. While depression is marked by sadness, numbness, and hopelessness, anxiety is defined by fear, dread, and hyper-vigilance. In clinical studies, 85% of women with postpartum anxiety report constant worry as their main symptom. In depression, 92% report persistent sadness. Intrusive thoughts - like imagining dropping the baby or something going wrong during a feed - appear in 68% of anxiety cases, compared to just 31% in depression-only cases. Physical symptoms are also more common in anxiety. Seventy-six percent of women with anxiety report physical signs like trembling, dizziness, or shortness of breath. In depression, that number drops to 43%. And while both can involve sleep problems, anxiety often means you can’t shut off your mind - even when the baby is asleep. The Edinburgh Postnatal Depression Scale (EPDS) helps sort this out. Women with no mental health issues score around 6.2. Those with anxiety alone average 9.8. Depression alone? Around 11.3. When both are present - which happens in nearly half of cases - scores jump to 14.7. But here’s the catch: the EPDS was designed for depression. It’s good at catching anxiety, but not perfect. That’s why newer versions now include a dedicated anxiety subscale, improving accuracy to 89%.Screening: What Works and What Doesn’t
Screening for postpartum anxiety isn’t optional anymore. The American College of Obstetricians and Gynecologists (ACOG) has recommended routine screening since 2018. Yet, as recently as 2015, only 12% of U.S. obstetric practices did it. By 2023, that number had jumped to 67% - progress, but still far from universal. The EPDS is still the most widely used tool. It’s quick, free, and easy to administer during postpartum checkups. But its specificity is only 68%. That means about one in three women flagged as anxious aren’t actually anxious - they’re just exhausted. For better accuracy, the Generalized Anxiety Disorder-7 (GAD-7) scale is gaining traction. It’s designed specifically for anxiety and has 89% sensitivity and 84% specificity for postpartum cases. It asks questions like: "Over the last two weeks, how often have you felt nervous, anxious, or on edge?" Responses range from "not at all" to "nearly every day." A score of 10 or higher signals likely anxiety. No blood test or brain scan can confirm it. Diagnosis is purely clinical - based on what you say, how you feel, and how long it’s lasted. That’s why it’s so easy to miss. Sixty-three percent of cases are initially dismissed as "normal stress." On average, women wait 11.3 weeks before getting proper help.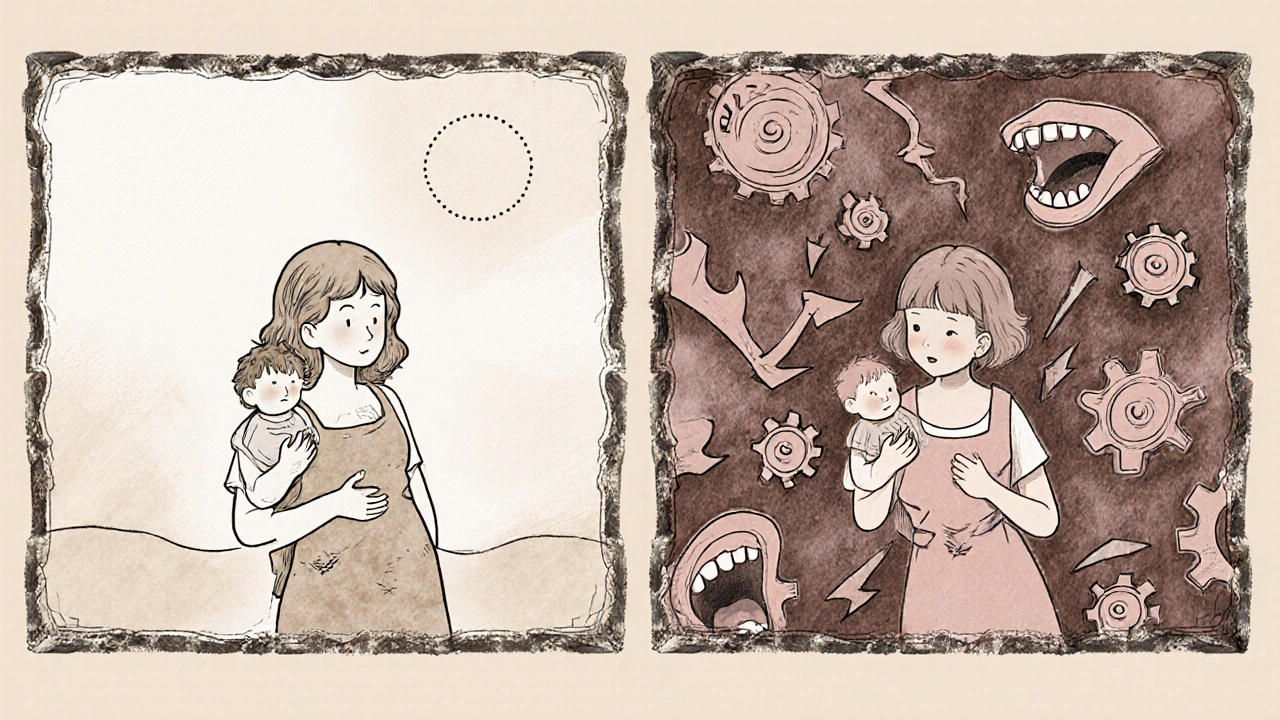
Risk Factors: Who’s Most Likely to Struggle
It’s not random. Certain factors dramatically increase the risk:- Having a prior anxiety disorder: 3.2 times higher risk
- Previous pregnancy loss: 2.7 times higher risk
- Infant medical complications after birth: 2.4 times higher risk
- History of postpartum depression: 3.8 times higher risk
Care Pathways: From Mild to Severe
Treatment isn’t one-size-fits-all. It’s tiered based on severity, measured mostly by EPDS scores:Mild Cases (EPDS 10-12)
For women with mild symptoms, therapy and lifestyle changes are the first step. Cognitive Behavioral Therapy (CBT) is the gold standard - it helps rewire anxious thought patterns. Even without medication, CBT reduces symptoms in 57% of postpartum women after 12 to 16 sessions. Lifestyle tweaks matter more than you think. A daily 30-minute walk outside reduces anxiety scores by 28% in eight weeks. Yoga has shown a 33% reduction in symptoms in clinical trials. These aren’t "nice-to-haves" - they’re part of the treatment plan.Moderate Cases (EPDS 13-14)
When symptoms interfere with daily life - you’re avoiding outings, skipping meals, or having panic attacks - CBT becomes essential. Group therapy with other new mothers helps too. Feeling isolated makes anxiety worse. Being in a room with others who get it? That’s powerful. Some providers now offer digital tools. The FDA-cleared app MoodMission uses CBT exercises to guide users through anxiety attacks. In a trial of 328 postpartum women, it cut anxiety symptoms by 53% in just 8 weeks.Severe Cases (EPDS 15 or higher)
When anxiety is debilitating - you can’t leave the house, you’re having daily panic attacks, or you’re terrified of being alone with your baby - medication is often needed. Selective Serotonin Reuptake Inhibitors (SSRIs) like sertraline are first-line treatment. They’re not FDA-approved specifically for postpartum anxiety, but decades of research show they’re safe and effective. Sertraline transfers only 0.3% of the maternal dose into breast milk. About 64% of women see improvement within eight weeks. The catch? SSRIs take 4 to 6 weeks to kick in. That’s why doctors pair them with mindfulness training during the waiting period. Daily mindfulness practice - even just 10 minutes of breathing exercises - reduces anxiety symptoms by 41% in two weeks.
What’s New and What’s Coming
The field is evolving fast. Brexanolone (Zulresso), approved for postpartum depression, is now being tested for anxiety. Phase III trials show a 72% response rate in just 60 hours - far faster than SSRIs. Insurance coverage has improved dramatically. In 2021, specific CPT billing codes (90834 and 90837) were introduced for postpartum anxiety. That pushed insurance reimbursement from 38% to 79% of cases. More providers are now willing to treat it because they can get paid. Still, only 15% of affected women get proper care. Rural areas are especially underserved - only 17% of rural hospitals offer specialized perinatal mental health programs. And the average delay in treatment? Six months.Where to Find Help
You don’t have to figure this out alone. Programs like The Women’s Place at Texas Children’s Pavilion for Women offer psychiatric care, medication management, and peer support groups. Hospitals with perinatal mental health units are growing - 43% of U.S. hospitals now have them. If you’re not sure where to start, ask your OB-GYN or midwife for a referral. Call your insurance company and ask: "Do you cover postpartum anxiety screening and therapy?" Many plans now do. And if you’re reading this and thinking, "That’s me," - you’re not broken. You’re not failing. You’re not alone. This is a medical condition, not a character flaw. And it can be treated.Is postpartum anxiety the same as baby blues?
No. Baby blues are mild mood swings, tearfulness, and fatigue that start within a few days after birth and fade by two weeks. Postpartum anxiety is more intense, lasts longer than two weeks, and includes physical symptoms like panic attacks, racing heart, and constant worry that interferes with daily life.
Can I take medication for postpartum anxiety while breastfeeding?
Yes. SSRIs like sertraline are considered safe during breastfeeding. Only about 0.3% of the maternal dose passes into breast milk, which is considered negligible. Many women successfully breastfeed while taking these medications. Always discuss options with your provider - they can help you choose the safest and most effective one for your situation.
How long does postpartum anxiety last?
Without treatment, it can last up to a year or longer. With proper care - therapy, medication, or both - most women see significant improvement within 8 to 12 weeks. Some feel better in just a few weeks with mindfulness and lifestyle changes. The key is not waiting to get help.
Can postpartum anxiety harm my baby?
Left untreated, yes. Chronic anxiety can affect bonding, reduce responsiveness to your baby’s cues, and increase stress hormones in your body - which can impact your baby’s emotional development. But when treated, mothers recover and form strong, healthy attachments. Early treatment protects both you and your child.
Why is postpartum anxiety underdiagnosed?
Because it’s often mistaken for normal stress. Many women feel guilty for not being "happy" enough after birth, so they hide their symptoms. Providers sometimes overlook anxiety because screening tools were designed for depression. And there’s still stigma - people think you should just "get over it." But this isn’t weakness. It’s biology.
What’s the best therapy for postpartum anxiety?
Cognitive Behavioral Therapy (CBT) is the most effective. It helps you identify and change anxious thought patterns. Group CBT is especially powerful because it reduces isolation. Mindfulness-based approaches and interpersonal therapy also work well, especially when combined with CBT.
Are there any natural remedies that help?
Yes - but they’re supplements, not substitutes. Daily walks, yoga, and mindfulness reduce symptoms significantly. Sleep, even in small chunks, helps. Omega-3 fatty acids and vitamin D may support mood, but they don’t replace therapy or medication for moderate to severe cases. Always talk to your doctor before starting supplements.
When should I call my doctor?
If you’ve felt overwhelmed, anxious, or panicked for more than two weeks - especially if it’s getting worse - call your provider. Don’t wait for your six-week checkup. If you’re having thoughts of harming yourself or your baby, seek help immediately. You’re not alone, and help is available.





14 Comments
Darragh McNulty
November 21, 2025 at 08:02
Just read this and cried in my coffee 😭 I thought I was failing as a mom... turns out my body was just screaming for help. Thank you for putting this out there. You’re not alone, sister. 🤍
Cooper Long
November 22, 2025 at 01:25
The clinical data presented here is methodologically sound and aligns with contemporary psychiatric guidelines. The distinction between anxiety and depression in the postpartum context is both clinically significant and statistically robust.
Sheldon Bazinga
November 22, 2025 at 02:57
lol so now we got anxiety because we had a baby? next theyll say its trauma if u spill formula. wake up sheeple. this is just the patriarchy turning moms into emotional wrecks so theyll take pills and shut up. #antidepressantsareforweaklings
Sandi Moon
November 23, 2025 at 16:24
Let us not ignore the elephant in the room: the pharmaceutical-industrial complex has weaponized postpartum vulnerability to sell SSRIs to vulnerable women. The GAD-7? A tool of systemic control. Who funded these trials? Who owns the patents? The silence on this is deafening.
Kartik Singhal
November 24, 2025 at 07:39
CBT? Really? In India we just say ‘beta, thoda relax karo’ and it works. Why overcomplicate? Also, why is everyone obsessed with Western metrics? EPDS? GAD-7? We have centuries of wisdom. 🤷♂️
Pravin Manani
November 25, 2025 at 05:23
From a neuroendocrinological perspective, the HPA axis dysregulation postpartum is a well-documented phenomenon. The cortisol surge, coupled with rapid progesterone withdrawal, creates a neurochemical cascade that precipitates anxiety phenotypes. CBT modulates prefrontal-limbic connectivity, while SSRIs enhance serotonergic tone - both are evidence-based interventions that mitigate maladaptive neuroplasticity.
Leo Tamisch
November 25, 2025 at 23:40
Wow. So we’re now diagnosing motherhood as a mental illness? 🤔 Next they’ll say crying over burnt toast is a trauma response. I mean… I get it. But is this just capitalism turning normal stress into a product? Also, emoji? Really? 🤦♂️
Daisy L
November 26, 2025 at 17:00
THIS. THIS. THIS. I had panic attacks every time I heard the baby cry at 3 a.m.-and my doctor told me to ‘just drink more water.’ I felt like a monster. Now I’m on sertraline, doing yoga, and actually smiling again. You are NOT broken. You are healing. 💪❤️
Anne Nylander
November 28, 2025 at 02:04
if you feel this way its not your fault!! you are doing amazing!! just breathe and ask for help!! i was there too and its okay to not be okay!! 🙌
Noah Fitzsimmons
November 29, 2025 at 08:34
Wait, so you’re telling me that after 4 hours of sleep and a screaming baby, you’re not supposed to feel like you’re going to die? That’s just… basic human biology. Why are we medicalizing tiredness now? I’ve got three kids and I’ve never seen a therapist. You’re weak.
Eliza Oakes
November 30, 2025 at 08:00
Oh please. ‘Postpartum anxiety’ is just a fancy term for ‘I didn’t get enough Instagram likes while holding my baby.’ Wake up. Everyone’s tired. Everyone’s scared. But we don’t need a 12-page diagnosis to cope. Maybe just… stop scrolling?
Clifford Temple
November 30, 2025 at 14:24
This is why America is collapsing. We’re turning motherhood into a trauma industry. Back in my day, women just sucked it up and fed the baby. Now we need apps, CPT codes, and SSRIs just to hold our kids. Pathetic.
Corra Hathaway
December 1, 2025 at 01:53
YOU ARE NOT ALONE. I had panic attacks in the grocery store at 2 a.m. buying diapers. I thought I was losing my mind. I cried in the cereal aisle. Then I found a group. Now I help others. You’re not broken. You’re becoming. 💛✨
Shawn Sakura
December 1, 2025 at 02:25
Thank you for this. I’ve been silent for 8 months. I thought I was just ‘not a good mom.’ Now I’m in CBT. I’m sleeping 5 hours. I’m holding my baby without shaking. It’s not perfect. But it’s better. And that’s enough.