QT Prolongation and Sudden Cardiac Death from Medications: Key Risk Factors You Need to Know
QT Medication Risk Checker
This tool helps you understand your risk of QT prolongation based on medications you're taking and key health factors. Remember, this is not medical advice - always consult your doctor.
Every year, hundreds of people in the U.S. die suddenly from a heart rhythm gone wrong-not because of a heart attack, but because of a medication they were taking. The culprit? A hidden electrical delay in the heart called QT prolongation. It doesn’t cause symptoms. It doesn’t show up on routine blood tests. It only shows up on an ECG-and even then, it’s often missed. Yet when it goes unchecked, it can trigger Torsades de Pointes, a chaotic heart rhythm that leads to sudden cardiac death. This isn’t rare. It’s preventable-if you know what to look for.
What QT Prolongation Really Means
The QT interval on an ECG measures how long it takes the heart’s lower chambers (ventricles) to recharge between beats. When that interval stretches too long, the heart’s electrical system becomes unstable. That’s QT prolongation. It’s not a disease. It’s a warning sign. And it’s triggered by more than 100 common medications-from antibiotics to antidepressants to anti-nausea drugs. The key number to watch is the corrected QT interval, or QTc. For men, anything over 450 milliseconds is prolonged. For women, it’s 470 milliseconds. But here’s what most people don’t realize: a QTc over 500 ms, or a jump of more than 60 ms from baseline, puts you in high-risk territory. That’s when the chance of Torsades de Pointes spikes. And once that rhythm starts, it can turn fatal in seconds.The Medications That Pose the Highest Risk
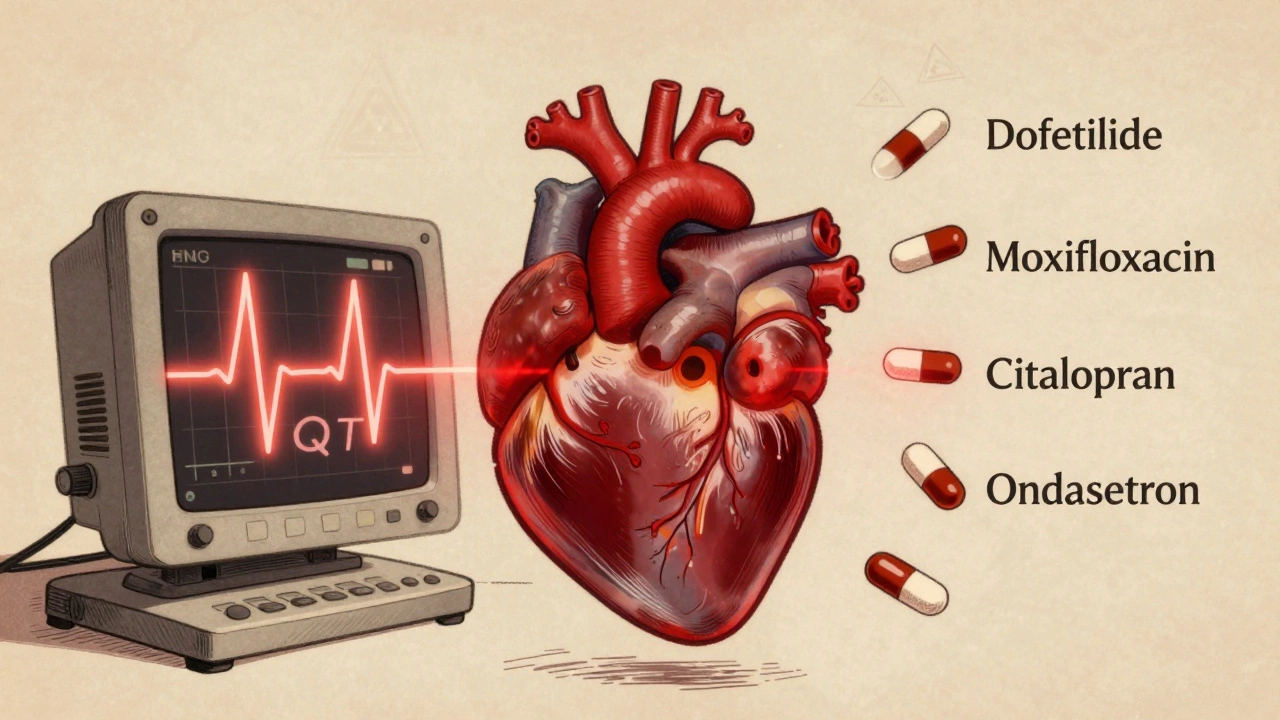
Not all QT-prolonging drugs are created equal. Some are low-risk. Others are ticking time bombs, especially when combined. Class III antiarrhythmics like dofetilide and sotalol are the most dangerous. Dofetilide alone causes Torsades in about 3.3% of patients-even when used exactly as prescribed. That’s why it’s only prescribed in hospitals with cardiac monitoring. Antibiotics like moxifloxacin (a fluoroquinolone) can push QTc up by 6 to 15 milliseconds. Compare that to ciprofloxacin, which barely moves the needle. Erythromycin? It doubles the risk of sudden death. And if you’re taking it with a CYP3A4 inhibitor like clarithromycin or grapefruit juice? The risk jumps fivefold. Antidepressants are another major concern. Citalopram at 40 mg daily increases QTc by an average of 8.5 ms. Escitalopram, its close cousin, only adds 4.2 ms. That’s why guidelines now cap citalopram at 20 mg for most adults. Antipsychotics like ziprasidone and haloperidol also carry significant risk-especially in older patients with heart disease. Even common drugs like ondansetron (for nausea) and certain antifungals can be risky. The problem isn’t just the drug itself. It’s the combo.Who’s Most at Risk?
You can’t predict who will have a bad reaction just by looking at their age or health. But some factors make it far more likely. First: existing heart disease. If you have heart failure, a prior heart attack, or thickened heart muscle, your risk of drug-induced arrhythmia goes up 10 to 100 times. That’s not a small increase. That’s a game-changer. Second: low potassium or magnesium. Hypokalemia (potassium under 4.0 mEq/L) is one of the most treatable risk factors. Correcting it cuts QT prolongation risk by 62%. Same with magnesium-many hospitals now give it routinely before high-risk infusions. Third: slow heart rate. Some drugs, like sotalol, work worse when your heart is beating slowly. That’s called reverse use dependence. It means the risk spikes at night, during sleep, or in people with heart block. That’s why QT prolongation often leads to death during rest-not activity. Fourth: multiple drugs. The average person over 65 takes nearly eight medications. About one in three of them are on a QT-prolonging drug. When you stack three or four of them together, the effect isn’t additive-it’s exponential. Fifth: genetics. Some people have inherited mutations in heart ion channels that make them extra sensitive. These aren’t tested for routinely. But if you’ve had unexplained fainting or a family history of sudden death before age 50, you should be evaluated.
Why ECGs Don’t Always Help
You might think: “Just get an ECG before taking the drug.” It sounds simple. But it’s not that easy. Automated ECG machines often misread the QT interval. Manual readings can differ by up to 40 milliseconds. That’s enough to miss a dangerous prolongation-or falsely flag someone who’s fine. And here’s the bigger problem: a normal QTc doesn’t mean safety. The real danger comes from uneven repolarization across the heart muscle-a pattern the standard 12-lead ECG can’t detect. That’s why some people die with a perfectly normal QT interval. Worse, many clinics now have automated QTc alerts in their electronic health records. But studies show 78% of these alerts are false positives. Doctors get so used to ignoring them, they start tuning out. That’s alarm fatigue-and it’s deadly.What Doctors Are Doing About It
The good news? Systems are improving. The FDA’s CiPA initiative, launched in 2013, replaced outdated lab tests with more accurate models that simulate how drugs affect human heart cells. It’s now used by 92% of major drug companies. New drugs are being screened for T-wave shape changes, not just QTc length. That’s a big step forward. Hospitals like Mayo Clinic added automated QTc alerts to their prescribing systems in 2015. Result? A 37% drop in high-risk medication orders. The University of Michigan’s QT Clinician Toolkit gives doctors a simple checklist: check potassium, check for drug interactions, check baseline QTc, check for heart disease. Simple. Fast. Effective. And now, AI is stepping in. Verily Life Sciences’ QTguard system uses machine learning to analyze ECG patterns and reduce false alarms by over half. It’s not perfect-but it’s helping.What You Can Do
If you’re on any prescription medication, ask these three questions:- Is this drug on the list of QT-prolonging medications? (Check azcert.org-it’s free and updated weekly.)
- Am I taking more than one drug that affects the QT interval? (Even over-the-counter meds like antihistamines can add up.)
- Have I had blood work to check my potassium and magnesium levels recently?
The Bigger Picture
Here’s the uncomfortable truth: QT prolongation isn’t just about bad drugs. It’s about how we prescribe. We’ve spent decades focusing on QTc as a simple number. But the science now shows it’s not the length-it’s the pattern. Not the drug alone-it’s the combo. Not the patient’s age-it’s their genetics, their electrolytes, their heart structure. The FDA has flagged 142 medications with QT warnings. Drug withdrawals due to QT risks cost the industry $18 billion a year. But the real cost? The lives lost because we treated this like a checkbox, not a crisis. The solution isn’t avoiding all QT-prolonging drugs. It’s using them smarter. With better tools. With better data. With better conversations between patients and providers. You don’t need to fear your medication. But you do need to understand the risks-and ask the right questions before you take that first pill.Can a normal QTc still mean I’m at risk for sudden cardiac death?
Yes. A normal QTc doesn’t guarantee safety. The real danger comes from uneven electrical recovery across different parts of the heart muscle-a pattern called spatial dispersion of repolarization. Standard 12-lead ECGs can’t detect this. That’s why some people experience sudden cardiac death even with a normal QT interval. Newer methods, like analyzing T-wave morphology, are being adopted to catch these hidden risks.
Which medications are the most dangerous for QT prolongation?
The highest-risk drugs include dofetilide and sotalol (antiarrhythmics), moxifloxacin (antibiotic), ziprasidone and haloperidol (antipsychotics), and citalopram at doses above 20 mg/day. Erythromycin also carries high risk, especially when taken with CYP3A4 inhibitors like clarithromycin or grapefruit juice. Even common drugs like ondansetron can contribute when combined with other QT-prolonging agents.
How do electrolyte imbalances increase QT prolongation risk?
Low potassium (hypokalemia) and low magnesium directly interfere with the heart’s ability to repolarize properly. Studies show correcting potassium levels above 4.0 mEq/L reduces QT prolongation risk by 62%. Magnesium supplementation is often given intravenously before high-risk procedures because it stabilizes heart cell membranes. These are simple, low-cost fixes that can prevent life-threatening arrhythmias.
Why are older adults at higher risk for drug-induced QT prolongation?
Older adults typically take more medications-on average, 7.8 per person over 65. About 34% of them are on at least one QT-prolonging drug. Their kidneys and liver process drugs slower, leading to higher blood levels. They’re also more likely to have low potassium, heart disease, or bradycardia-all of which amplify risk. Many are on multiple drugs that interact through the CYP3A4 enzyme system, creating dangerous combinations.
Should I get an ECG before starting a new medication?
If you’re over 65, have heart disease, are taking multiple medications, or have a history of fainting or family history of sudden death, yes. A baseline ECG helps establish your normal QTc and detect hidden issues. For younger, healthy people on a single low-risk drug, routine ECGs aren’t usually needed. But if you’re unsure, ask your doctor. It’s a 10-minute test that could save your life.
Are there any new technologies helping to prevent QT-related deaths?
Yes. The FDA’s CiPA initiative uses advanced computer models to predict drug effects on heart cells, replacing outdated tests. AI tools like QTguard by Verily Life Sciences analyze ECG patterns to reduce false alarms by 53%. The International Council for Harmonisation now requires new drugs to be tested for T-wave shape changes-not just QTc length. These changes are making drug safety screening far more accurate and personalized.





15 Comments
Chris Park
December 6, 2025 at 04:05
The FDA’s CiPA initiative? More like a PR stunt to keep Big Pharma off the hook. They’re still using the same flawed models-just with fancier algorithms. If you think AI can fix what corporate greed broke, you’re the real delusion. I’ve seen ECGs altered in EHRs to clear high-risk meds. This isn’t medicine. It’s a profit-driven slaughterhouse.
And don’t get me started on ‘baseline ECGs.’ Hospitals charge $800 for that. Meanwhile, the same system that flags your QTc ignores your $12,000 insulin co-pay. You think they care if you live? They care if you bill.
They’ll bury 142 drugs under ‘warnings’ while letting the real killers-like metformin-induced lactic acidosis-fly under the radar. Double standards. Always double standards.
Inna Borovik
December 6, 2025 at 08:34
Let’s be clear: QT prolongation isn’t a mystery-it’s a systemic failure of pharmacovigilance. The data has been available for decades. The problem isn’t lack of knowledge-it’s lack of enforcement.
Every time a drug gets approved with a QT warning, it’s a calculated risk. The company knows the death rate. They’ve modeled it. They’ve priced it. And they’ve decided the profit margin outweighs the liability.
When you see a 3.3% Torsades rate on dofetilide and still allow it outside monitored units? That’s not negligence. That’s complicity. The FDA doesn’t regulate safety-they regulate public perception.
And yes, potassium matters. But why is it left to the patient to ask for it? Why isn’t it mandatory pre-screening? Because convenience trumps care. Always.
Jackie Petersen
December 6, 2025 at 22:16
So let me get this straight-we’re terrified of a 60ms QT jump but okay with 200mg of acetaminophen daily? Or 1000mg of ibuprofen? Or 12 cups of coffee? Where’s the outrage there?
And why are we blaming drugs when the real culprit is the American healthcare system? You get one 15-minute visit. Your doctor’s on a 3-minute timer. They don’t have time to check your electrolytes, your meds, your family history, or your ECG. They just check the box and move on.
Also, who the hell is Verily? Google’s health division? That’s the company that lost 100k patient records? Now they’re our savior? Please. This is all theater. We’re being sold snake oil with a blockchain logo.
Annie Gardiner
December 7, 2025 at 02:09
I think we’ve all been conditioned to fear the invisible. The body’s electricity-this beautiful, silent dance of ions-and now we’re told it’s fragile? That a pill can tip it into chaos?
But here’s the thing: what if it’s not the drugs? What if it’s the silence? The loneliness? The stress that makes our hearts beat wrong even before the meds?
Maybe QT prolongation isn’t just a number on a screen. Maybe it’s the echo of a life lived without rest, without connection, without safety. We treat the heart like a machine, but it’s not. It’s a soul with wires.
And we keep wiring it wrong.
joanne humphreys
December 7, 2025 at 20:38
This is one of the most important public health pieces I’ve read in years. I work in a rural clinic and we see this every day-older patients on 8+ meds, no labs done in over a year, and no one asking about fainting spells or family history.
I’ve started using the Michigan toolkit. It takes 90 seconds. I print it out. I go through it with patients. Their eyes light up. They feel seen.
And yes, the ECGs are messy. The alerts are noisy. But we’re learning. We’re adapting. It’s not perfect, but we’re trying. That’s more than most systems are doing.
Thank you for writing this. It’s not just information-it’s a call to action. And we’re answering.
Mayur Panchamia
December 8, 2025 at 10:47
Let me tell you something-America is a graveyard of pharmaceutical lies! You think they care about your QT interval? They care about your insurance card! They care about your copay! They care about your credit score!
And now they want you to trust AI? Verily? Google? The same company that helped build surveillance capitalism? You’re letting the fox guard the henhouse!
Meanwhile, in India, we don’t need AI-we have tradition! We have Ayurveda! We have turmeric and yoga and fasting! We don’t need your toxic pills! We don’t need your ECGs! We don’t need your false alarms!
But no-you want to keep poisoning your people with your corporate science! Shame on you!
Kenny Pakade
December 9, 2025 at 22:11
QT prolongation? Yeah, right. Another fear-mongering scare tactic to get people to pay for unnecessary tests. I’ve been on citalopram for 7 years. My QTc is 430. I’m fine. My doctor says so. Your ‘risk factors’ are just guilt-tripping middle-class Americans into buying more healthcare.
And why are you blaming doctors? Because you don’t want to admit that most people don’t die from QT prolongation-they die from being lazy, overweight, and on Facebook all day.
Stop weaponizing ECGs. Stop scaring people with numbers. Just let people live. We’re not lab rats.
brenda olvera
December 11, 2025 at 00:07
Wow. This is so important. I just started a new med last week and had no idea. I’m going to ask my doctor for a potassium test tomorrow. I’m so glad someone wrote this clearly. I feel empowered now. Thank you.
Also, I think we need more stories like this. Not just from doctors. From patients. From families. From people who almost didn’t make it.
We need to talk about this. Not just in clinics. At dinner tables. On buses. In schools.
Knowledge is the only real medicine.
Myles White
December 11, 2025 at 16:50
I’ve spent the last three years in cardiac electrophysiology research, and I can tell you this: the real revolution isn’t in AI or even CiPA-it’s in the shift from scalar measurements to vectorial analysis. We’re moving from ‘is the QT long?’ to ‘is the repolarization gradient abnormal?’
That’s why T-wave morphology matters. That’s why 12-lead ECGs are obsolete for risk stratification. We need 256-lead high-resolution mapping, or at least dynamic QT variability analysis. But hospitals won’t pay for it. Insurers won’t cover it. So we’re stuck with the 1950s tech.
And yes, drug interactions are exponential. We’ve modeled 4-drug combos that increase risk by 1,200%. But no one’s building a clinical decision support system that actually integrates all variables-electrolytes, genetics, renal function, CYP phenotypes. We’re still using spreadsheets.
This isn’t a knowledge gap. It’s a funding gap. And until we fund cardiac safety like we fund cancer research, people will keep dying in their sleep.
And yes-I’ve seen it. I’ve watched a 72-year-old woman code in the ER because she took ondansetron with sertraline and had a potassium of 3.8. She didn’t have a ‘long QT.’ She had a broken system.
Saketh Sai Rachapudi
December 12, 2025 at 12:15
How many people die because they take antibiotics without knowing? I know a guy-his mom died in her sleep after taking azithromycin with her heart pill. No ECG. No labs. No warning. Just… gone.
And now you want us to trust AI? Google? Who’s coding these algorithms? Americans? With their pharma money? I don’t trust anyone anymore.
Why not just ban all QT-prolonging drugs? Why not make every patient get an ECG before any new med? Why is this so hard? Because profit. Always profit.
They don’t want you to know. They want you to take the pill. And die quietly.
Arjun Deva
December 14, 2025 at 11:33
Let’s be honest-this whole thing is a distraction. The real killer isn’t QT prolongation. It’s the fact that 30% of Americans can’t afford their meds, so they skip doses. Then they get sick. Then they go to the ER. Then they get a bunch of new drugs. Then their QT gets prolonged. Then they die.
It’s not the drug. It’s the poverty.
And now we’re giving people checklists? Like they’re playing a game? ‘Check potassium. Check meds. Check family history.’
What if they don’t have a doctor? What if they don’t have insurance? What if they work two jobs and sleep 4 hours a night?
Stop blaming the ECG. Start fixing the system.
Clare Fox
December 15, 2025 at 13:21
What if the real problem isn’t the drugs or the ECGs or even the electrolytes? What if it’s that we’ve stopped listening to our bodies?
We’ve turned medicine into a checklist. A spreadsheet. A number. But the heart doesn’t care about milliseconds. It cares about peace. About rest. About being held.
Maybe the most dangerous drug isn’t on the list. Maybe it’s the belief that we can fix everything with technology.
I don’t know. I just know I feel lighter after reading this. Like someone finally saw me.
Akash Takyar
December 15, 2025 at 16:37
As a healthcare professional from India, I want to express my deep appreciation for this comprehensive and scientifically accurate article. The integration of clinical guidelines, pharmacological data, and systemic critique is exemplary.
In our context, where access to ECGs and electrolyte testing is limited, the emphasis on patient education and simple checklists is not just helpful-it is life-saving.
I have already shared this with my colleagues and medical students. We must advocate for institutional adoption of the Michigan toolkit. We must push for mandatory electrolyte screening in polypharmacy patients. We must train our physicians to see beyond the QTc.
This is not just medicine. It is moral responsibility.
Kumar Shubhranshu
December 17, 2025 at 09:22
QT prolongation is real but overblown. Most people are fine. Stop panicking.
Karen Mitchell
December 18, 2025 at 07:15
It is imperative to note that the conflation of statistical risk with individualized clinical necessity represents a fundamental epistemological error in contemporary medical practice. The normalization of algorithmic decision-making, coupled with the commodification of cardiac biomarkers, has resulted in a pathological over-medicalization of the human condition.
One must question the ontological status of the QT interval: is it a physiological phenomenon, or a construct of pharmaceutical surveillance capitalism?
Furthermore, the assertion that ‘a normal QTc does not guarantee safety’-while technically accurate-is rhetorically manipulative. It induces fear, not awareness. It transforms preventative medicine into a regime of perpetual suspicion.
It is not the drugs that are dangerous. It is the discourse surrounding them.