Restless Leg Syndrome: Why Dopaminergic Medications Are No Longer First-Line and What Works Better
For decades, if you had restless leg syndrome (RLS), your doctor likely prescribed a dopamine agonist like Mirapex or Requip. It made sense-these drugs worked fast, often easing symptoms within an hour. But today, that approach is outdated, risky, and often backfires. The truth is, dopaminergic medications for RLS are no longer the go-to solution. In fact, leading sleep experts now warn that using them long-term can make your symptoms worse, not better.
What Happens When Dopamine Medications Don’t Work Anymore
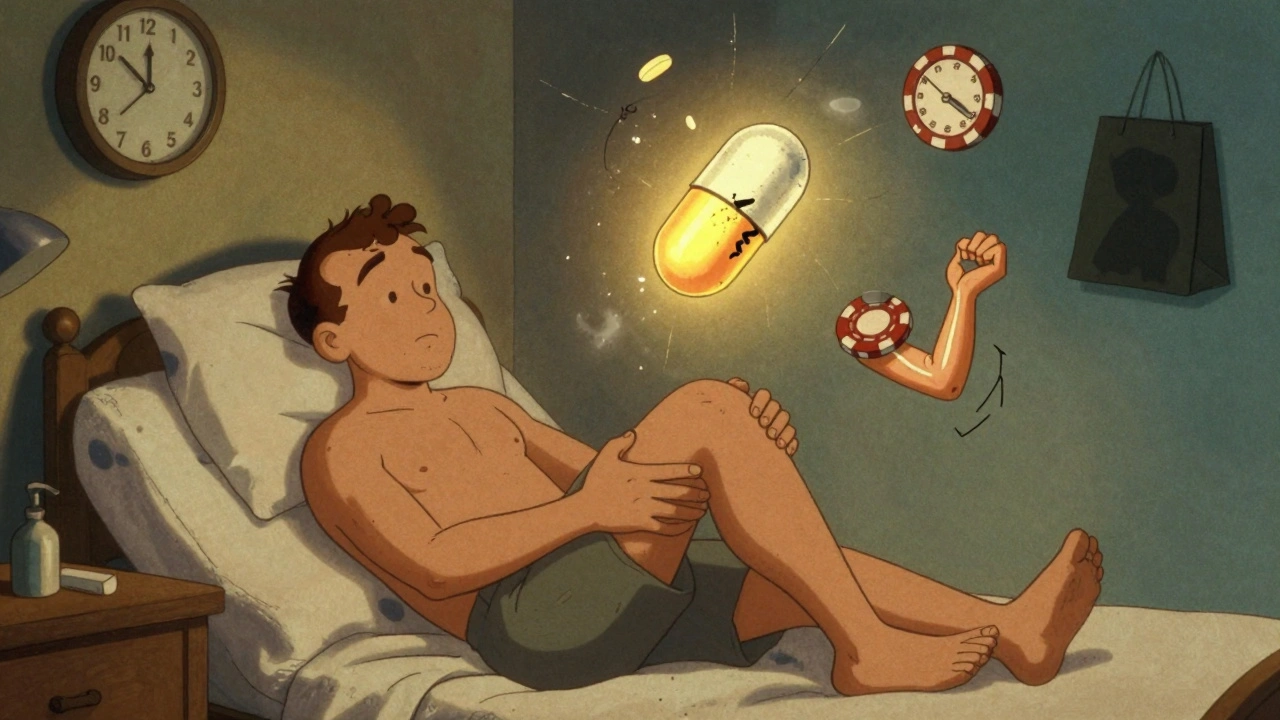
Restless leg syndrome causes an irresistible urge to move your legs, usually at night or when you’re sitting still. The discomfort is hard to describe-creeping, tingling, crawling-something that only movement can temporarily relieve. For years, dopamine drugs like pramipexole and ropinirole were the standard. They mimic dopamine, a brain chemical thought to be low in people with RLS. But here’s the catch: after months or years of daily use, something called augmentation kicks in. That’s when your symptoms start earlier in the day-maybe at 2 p.m. instead of 8 p.m. They get stronger. They spread from your legs to your arms. You’re not just dealing with RLS at night anymore-you’re dealing with it all day. A 2018 study in Neurology found that 40% to 60% of people on dopamine agonists developed augmentation within one to three years. That’s more than half. And it doesn’t stop there. The International Restless Legs Syndrome Study Group (IRLSSG) found that patients on these drugs see their symptom scores jump by 5 to 10 points on the standard rating scale. That’s a huge increase in discomfort. Worse, 30% to 40% of people start feeling the urge in their arms and hands. You can’t just move your legs anymore-you need to move your whole body.The Hidden Dangers: Impulse Control and Addiction
Beyond augmentation, dopamine agonists carry another silent risk: impulse control disorders. Studies show that 6.1% of RLS patients on these drugs develop compulsive behaviors like gambling, shopping, binge eating, or hypersexuality. That’s more than 12 times higher than in the general population. These aren’t side effects you can easily spot. Many patients don’t realize they’re acting out of character until a loved one points it out-or a bank statement shows $10,000 in online casino bets. The FDA added black box warnings to all dopamine agonists in 2022, the strongest safety alert possible. Still, many patients are still being prescribed them without being told the full picture. One Reddit user, "RLSWarrior42," described how after two years on Mirapex, his symptoms exploded. "It took six months to taper off," he wrote. "The rebound was brutal. I thought I was going crazy."What’s Replacing Dopamine Drugs? The Real First-Line Options
The American Academy of Sleep Medicine (AASM) updated its guidelines in December 2024-and it was a game-changer. Dopamine agonists are now officially second-line therapy. First-line? Alpha-2-delta ligands. These include gabapentin enacarbil (Horizant), pregabalin (Lyrica), and gabapentin. They don’t touch dopamine. Instead, they calm overactive nerve signals in the spinal cord. That’s why they don’t cause augmentation. They don’t make symptoms worse over time. They just work. A 2023 meta-analysis in JAMA Neurology compared pramipexole (0.5 mg) to pregabalin (150 mg). At 12 weeks, both reduced symptoms by about the same amount. But at 52 weeks? Pregabalin held steady. Pramipexole lost 35% of its effectiveness due to augmentation. That’s not a minor difference-it’s the difference between managing your life and being controlled by your symptoms. Gabapentin enacarbil is especially effective. Approved by the FDA in 2011, it’s dosed once daily at 600 mg. Studies show 40% to 60% symptom reduction on the IRLSSG scale. And unlike dopamine drugs, it doesn’t carry impulse control risks. Side effects? Dizziness (26% of users), drowsiness, and sometimes weight gain-about 2.5 kg over 12 weeks. Most people tolerate it well.Why Do Some Doctors Still Prescribe Dopamine Drugs?
The answer? Habit and speed. Dopamine agonists work fast. If you’re in pain tonight, a pill that helps by morning feels like a miracle. Alpha-2-delta ligands take days-or even weeks-to build up in your system. That’s harder for patients to stick with, and harder for doctors to recommend when someone’s desperate. But here’s the reality: if you’re taking dopamine agonists daily, you’re not just treating RLS-you’re setting yourself up for a bigger problem down the road. The 2024 AASM guidelines say: avoid dopamine agonists for daily use beyond six months. And if you’ve been on them longer? You’re already at risk. A 2020 study in the European Journal of Neurology found that 70% of patients on daily carbidopa-levodopa (Sinemet) developed augmentation after six months. That’s why most neurologists now reserve it for occasional use only-like if you’re flying or need a one-time fix.
What About Opioids? Are They Safe?
Low-dose opioids like oxycodone (5 mg) can reduce RLS symptoms by 50% to 70%. That’s powerful. But they’re not a first-line option. The risk of misuse is real-even at low doses. A 2021 study in Pain Medicine found only 0.8% of RLS patients on opioids under 30 mg morphine equivalent daily developed misuse. That’s low, but not zero. And if you have a history of substance use, it’s a hard no. Doctors who use opioids for RLS do so cautiously, usually only after other options fail. They monitor closely. They don’t prescribe for long-term daily use. And they never combine them with alcohol or sedatives.Non-Medication Strategies That Actually Work
Medication isn’t the whole story. In fact, lifestyle changes can cut your symptoms by 20% to 30%-without any pills.- Cut caffeine. 80% of RLS patients consume caffeine daily. Coffee, soda, energy drinks-even dark chocolate-can trigger or worsen symptoms. Try switching to decaf after noon.
- Avoid alcohol. Alcohol makes RLS worse in 65% of people. It doesn’t help you sleep better-it just delays the discomfort until later.
- Check your iron. RLS is linked to low brain iron. If your serum ferritin is below 75 mcg/L, oral iron supplements (100-200 mg elemental iron daily) can improve symptoms by 35% in 12 weeks. Ask your doctor for a blood test.
- Improve sleep hygiene. Go to bed and wake up at the same time every day. Keep your bedroom cool and dark. Avoid screens an hour before bed.
- Move before bed. A 10-minute walk or light stretching can help. But don’t overdo it-intense exercise right before bed can make symptoms worse.
What to Do If You’re Already on a Dopamine Drug
If you’re on pramipexole, ropinirole, or rotigotine and you’ve been taking it daily for more than six months, here’s what you need to do:- Don’t stop cold turkey. That can cause severe rebound symptoms.
- Work with your doctor to reduce your dose by 25% every one to two weeks.
- Start an alpha-2-delta ligand like gabapentin enacarbil or pregabalin during the taper. This helps prevent withdrawal and keeps symptoms under control.
- Ask for a ferritin blood test. If you’re low in iron, start supplementation.
- Eliminate caffeine and alcohol for at least four weeks and track your symptoms.
The Big Picture: A Shift in How We Treat RLS
The treatment landscape has changed. In 2010, 75% of new RLS prescriptions were for dopamine agonists. By 2024, that number dropped to 20%. Meanwhile, alpha-2-delta ligands now make up 65% of new prescriptions. The market reflects this too: dopamine agonist sales for RLS are projected to fall from $360 million in 2024 to $120 million by 2030. Alpha-2-delta drugs? They’ll grow to nearly $900 million. This isn’t just a trend-it’s science. Experts like Dr. John Winkelman and Dr. Arthur Walters have spent decades studying RLS. Their message is clear: dopamine agonists are not the answer for chronic RLS. They’re a temporary fix that leads to long-term harm. The real goal isn’t just to quiet your legs at night. It’s to live without fear that your symptoms will get worse tomorrow. That’s why the new standard is clear: start with what’s safe, what lasts, and what doesn’t make things worse.Frequently Asked Questions
Are dopamine agonists still used for restless leg syndrome?
Yes, but only in limited cases. Dopamine agonists like pramipexole and ropinirole are no longer first-line treatment. They’re now reserved for patients with infrequent symptoms (less than three nights a week) or those who can’t tolerate other options. Long-term daily use is strongly discouraged due to the high risk of augmentation and impulse control disorders.
What is augmentation in restless leg syndrome?
Augmentation is when RLS symptoms worsen due to long-term use of dopamine medications. Symptoms start earlier in the day (often 2-6 hours sooner), spread to other body parts like the arms, become more intense, and occur more frequently. It’s a direct side effect of the drug, not a progression of the disease. Up to 80% of patients on daily dopamine agonists for five years develop augmentation.
What are the best alternatives to dopamine agonists for RLS?
The top alternatives are alpha-2-delta ligands: gabapentin enacarbil (Horizant), pregabalin (Lyrica), and gabapentin. These drugs calm nerve signals without affecting dopamine, so they don’t cause augmentation. They’re now the first-line recommendation by the American Academy of Sleep Medicine. Iron supplements are also recommended if ferritin levels are below 75 mcg/L.
How long does it take for gabapentin enacarbil to work for RLS?
Unlike dopamine agonists, which work within an hour, gabapentin enacarbil takes several days to build up in your system. Most people notice improvement within one to two weeks, with full effect by four weeks. It’s not fast, but it’s sustainable-without the risk of worsening symptoms over time.
Can lifestyle changes really help with restless leg syndrome?
Yes. Cutting caffeine, avoiding alcohol, improving sleep habits, and getting regular movement can reduce symptoms by 20% to 30%. Iron deficiency is a major contributor-about 35% of patients with low ferritin see improvement after 12 weeks of iron supplements. Lifestyle changes aren’t a cure, but they’re a powerful foundation for any treatment plan.
Should I stop my dopamine medication on my own?
No. Stopping dopamine agonists abruptly can cause severe rebound symptoms. Always work with your doctor to taper off slowly-usually reducing the dose by 25% every one to two weeks. Start a replacement medication like gabapentin enacarbil during the taper to keep symptoms under control. Never make changes without medical guidance.






10 Comments
David Brooks
December 7, 2025 at 15:36
This article literally saved my life. I was on Mirapex for 4 years and woke up one day with my arms twitching at 3 p.m. I thought I was losing it. Tapered off with gabapentin enacarbil and now I sleep like a baby. No more gambling debts, no more crawling skin-just peace. Thank you for writing this.
Jennifer Anderson
December 9, 2025 at 04:54
omg i had no idea dopamine drugs could make rls worse?? i was on ropinirole for 2 years and thought it was just getting worse with age. i just started pregabalin last week and my legs feel like they finally chill out at night. also cut out coffee after 2pm and holy crap it helped. thanks for the heads up!!
Oliver Damon
December 10, 2025 at 14:31
The shift in clinical guidelines reflects a broader paradigm in neurology: moving from symptomatic palliation to disease-modifying, non-dopaminergic modulation. The augmentation phenomenon is a classic iatrogenic paradox-intended therapeutic action inducing pathological sensitization of postsynaptic receptors. Alpha-2-delta ligands act via voltage-gated calcium channel inhibition, reducing excitatory neurotransmitter release in the dorsal horn, thereby suppressing spinal hyperexcitability without triggering dopaminergic downregulation. The meta-analytic data from JAMA Neurology is robust: sustained efficacy at 52 weeks versus rapid tolerance with agonists. This isn't anecdotal-it's evidence-based neuropharmacology.
Kurt Russell
December 11, 2025 at 17:24
IF YOU’RE ON A DOPAMINE DRUG AND STILL THINK IT’S WORKING-YOU’RE BEING LIED TO BY YOUR OWN BRAIN. AUGMENTATION IS SILENT. IT HITS YOU WHEN YOU’RE TOO DEEP. I TOOK 6 MONTHS TO TAPER. I CRIED. I PANICKED. BUT NOW? I WALK MY DOG AT 8PM WITHOUT FEELING LIKE MY LEGS ARE BEING STABBED. GABAPENTIN ENACARBIL IS A GIFT. DON’T WAIT UNTIL YOUR ARMS START MOVING ON THEIR OWN. DO IT NOW.
Ryan Sullivan
December 11, 2025 at 22:00
Let’s be honest-this is just another case of Big Pharma pivoting to sell more expensive generics. Gabapentin is off-patent, so now it’s ‘first-line.’ Meanwhile, dopamine agonists were proven effective in thousands of clinical trials. The ‘augmentation’ narrative feels like a scare tactic to justify a cost-cutting shift. And let’s not pretend iron supplements are magic-unless you’re anemic, they’re placebo at best. This reads like a Reddit manifesto disguised as medical advice.
Wesley Phillips
December 12, 2025 at 16:58
so like... dopamine bad iron good caffeine bad but also i just took a shot of espresso and my legs are fine so idk man maybe its all in my head lmao
Kyle Oksten
December 14, 2025 at 08:20
There’s a critical distinction between symptom suppression and treatment. Dopamine agonists suppress. Alpha-2-delta ligands modulate. The former masks, the latter restores balance. If your doctor hasn’t checked your ferritin in the last year, they’re not treating RLS-they’re managing a side effect cascade. This isn’t about preference. It’s about neurobiology. And if you’re still on a dopamine agonist past six months, you’re not just at risk-you’re already in the danger zone.
Sam Mathew Cheriyan
December 14, 2025 at 08:59
they dont want you to know the real truth. dopamine agonists are banned in europe because they make you turn into a zombie and the government is hiding it. gabapentin is just a gateway drug to get you hooked on the real solution: magnetic therapy from the moon. also your ferritin test is fake. they inject mercury into your blood to make you think you’re low. i got cured by sleeping with a magnet under my pillow and chanting in latin.
Ted Rosenwasser
December 15, 2025 at 08:31
Interesting how the article cites JAMA and Neurology like they’re gospel, but completely ignores the 2021 Cochrane review that found no significant long-term advantage of gabapentin over placebo in mild RLS. Also, the 600mg dose of gabapentin enacarbil? That’s a prescription for daytime sedation. I’m a neurologist. I’ve seen patients become human puddles on the couch. This isn’t medicine-it’s wellness influencer content dressed in academic jargon.
Helen Maples
December 15, 2025 at 10:13
David, your comment is exactly why this article matters. You’re not alone. If you’re reading this and you’re still on Mirapex-stop waiting for your doctor to bring it up. Print this article. Take it to your appointment. Say, ‘I want to transition to gabapentin enacarbil and get my ferritin checked.’ You deserve to sleep without fear. And if your doctor resists? Get a second opinion. Your legs are worth it.