Blood Sugar Control: Your Guide to Stable Glucose Levels
When talking about blood sugar control, the process of keeping blood glucose within a healthy range. Also known as glucose regulation, it’s the cornerstone of feeling steady and avoiding long‑term health issues.
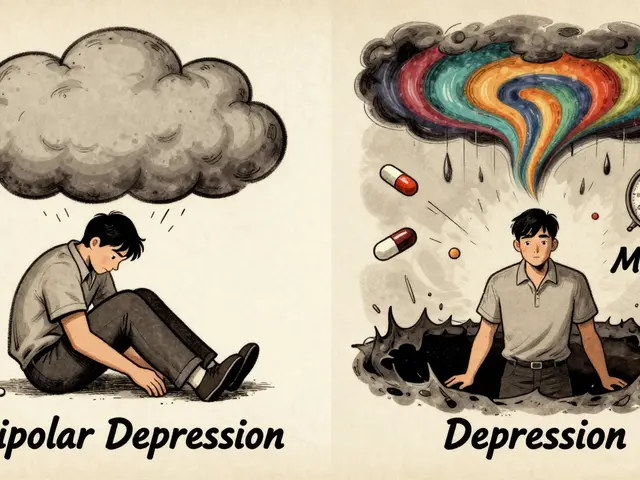
One of the biggest forces behind blood sugar control is diabetes, a chronic condition where the body struggles to manage glucose. Whether you have type 1, type 2, or gestational diabetes, the disease shapes every decision you make about meals, activity, and medication. Recognizing diabetes as the primary context helps you pick the right tools and strategies, because the condition directly influences how your body processes sugar.
Key Elements of Effective Blood Sugar Control
Effective blood sugar control needs regular monitoring, and that’s where a glucometer, a handheld device that measures blood glucose levels becomes essential. By checking your numbers before meals, after exercise, and before bed, you create a feedback loop that guides food choices and medication timing. The act of monitoring empowers you to spot trends, avoid surprise spikes, and adjust on the fly.
Another crucial piece is insulin therapy, the use of injected or pumped insulin to lower blood glucose. Insulin directly influences blood sugar control by facilitating glucose uptake into cells, especially for people with type 1 or advanced type 2 diabetes. Choosing the right type—rapid‑acting, long‑acting, or an automated pump—depends on your lifestyle, eating patterns, and how your body responds.
Diet acts like the fuel control lever. A low‑glycemic diet, a eating plan focused on foods that raise blood sugar slowly helps smooth out peaks and valleys. Think whole grains, legumes, non‑starchy vegetables, and berries instead of sugary drinks or refined carbs. Pairing carbs with protein or healthy fats further blunts spikes, making it easier for insulin (or your pancreas) to keep pace.
Physical activity is the hidden catalyst that makes everything else work better. Even short walks after meals improve insulin sensitivity, meaning your cells need less insulin to pull glucose from the bloodstream. Strength training builds muscle mass, which acts as a glucose sink, enhancing long‑term control. Consistency matters more than intensity, so aim for a mix of cardio and resistance work each week.
Supplements can fine‑tune the system, but they’re not magic bullets. Elements like chromium, magnesium, and cinnamon have modest evidence for helping glucose metabolism, especially when paired with a solid diet and medication plan. Always check with a healthcare professional before adding anything, because interactions with insulin or oral drugs can shift your numbers unexpectedly.
Finally, education and mindset seal the deal. Knowing how stress hormones like cortisol raise blood sugar helps you adopt coping tactics—mindfulness, deep breathing, or a hobby break. Sleep quality also plays a role; poor rest can blunt insulin response, leading to higher readings. By treating blood sugar control as a daily habit rather than a single action, you set yourself up for sustainable success.
Below, you’ll find a curated collection of articles that dive deeper into each of these topics—from comparing diabetes medications to mastering glucometer use, from meal‑planning tricks to exercise routines that boost insulin sensitivity. Use these resources to build a personalized plan that keeps your glucose steady and your life on track.

Exercise and Diabetes: Proven Physical Activity Plans to Control Blood Sugar
Learn proven exercise plans to control blood sugar in type 1 and type 2 diabetes. Discover how walking, strength training, and HIIT lower HbA1c, improve insulin sensitivity, and reduce complications-backed by the latest clinical guidelines.
Read More
Vidagliptin and Insulin Reduction in Type 2 Diabetes: What the Evidence Says
Explore how vidagliptin, a DPP‑4 inhibitor, can lower insulin needs in type 2 diabetes, backed by trial data, safety info, and practical tips.
Read More