Drug Overdose: Causes, Risks, and How to Stay Safe
When someone takes too much of a medication or drug, it can lead to a drug overdose, a medical emergency where the body can’t process the substance, leading to life-threatening symptoms. Also known as toxic overdose, it happens with prescription drugs, illegal substances, or even supplements when used incorrectly or in combination. It’s not always about intent—many overdoses occur because people don’t realize how dangerous mixing drugs can be, or because a medication’s effect changes when taken with food, alcohol, or other pills.
A opioid overdose, a type of drug overdose caused by drugs like oxycodone, fentanyl, or heroin is the most common deadly form. These drugs slow breathing to a stop, and without quick help, death follows in minutes. But it’s not just opioids. Overdoses from benzodiazepines, sleep aids, or even high doses of acetaminophen can be fatal. What makes it worse is that many people take these drugs daily for pain or anxiety, and a small change—like skipping a meal, drinking alcohol, or switching to a new generic version—can push them over the edge. That’s why dose adjustments after switching generics, as covered in several posts here, matter more than most realize.
Naloxone, a life-saving medication that reverses opioid overdoses is now available without a prescription in many places. It’s not a cure, but it buys critical time. If you or someone you know uses opioids, even as prescribed, keeping naloxone on hand is as important as having a fire extinguisher. It’s not about assuming someone will overdose—it’s about preparing for the unexpected. And while naloxone works on opioids, it won’t help with overdoses from stimulants like cocaine or antidepressants, which require different emergency responses. That’s why knowing what you’re taking, and what it interacts with, is key. Posts on drug interactions, like how Bactrim spikes INR levels or how licorice messes with blood pressure meds, show how easily harmless-seeming combinations turn dangerous.
Many overdoses are preventable. Keeping a symptom diary, a tool to track side effects and unusual reactions to medications can catch early warning signs before things spiral. Recording changes in mood, sleep, breathing, or heart rhythm helps doctors spot trouble fast. So does knowing when to question a prescription label, how to store meds properly, or when to avoid expired drugs—topics covered in detail across these posts. You don’t need to be a medical expert to save a life. Just know the signs: slow or shallow breathing, blue lips, unresponsiveness. Call 911. Give naloxone if you have it. Stay with the person until help arrives.
There’s no shame in asking for help. Many people who overdose are managing chronic pain, anxiety, or depression. They’re not reckless—they’re trying to feel better. The system often fails them by not explaining risks clearly, not checking for interactions, or not offering alternatives. But you can take control. Know your meds. Know your risks. Know what to do if something goes wrong. Below, you’ll find real, practical guides on how to avoid dangerous drug combinations, recognize side effects early, and protect yourself from preventable harm—because when it comes to drug overdose, knowledge isn’t just power. It’s the difference between life and death.
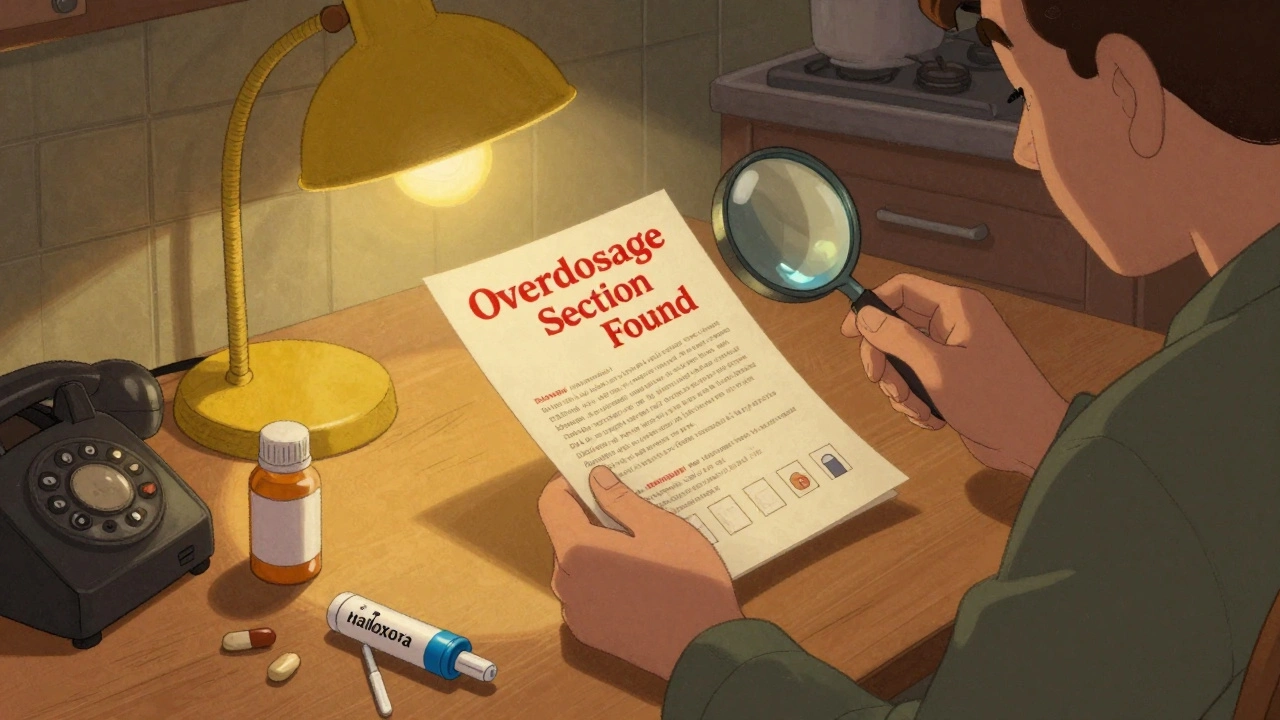
How to Read Medication Guides for Overdose Warnings and Antidotes
Learn how to read medication guides to spot overdose warnings and locate antidotes like naloxone. This guide shows you exactly where to look, what to do, and why it could save a life.
Read More