Lymphangioleiomyomatosis: Causes, Symptoms, and Treatment Options
When you hear lymphangioleiomyomatosis, a rare, progressive lung disease that primarily affects women of childbearing age. Also known as LAM, it causes abnormal muscle-like cells to grow in the lungs, kidneys, and lymphatic system, slowly damaging lung tissue and making breathing harder over time. It’s not cancer, but it behaves like one — spreading and destroying healthy tissue without clear warning signs until it’s advanced.
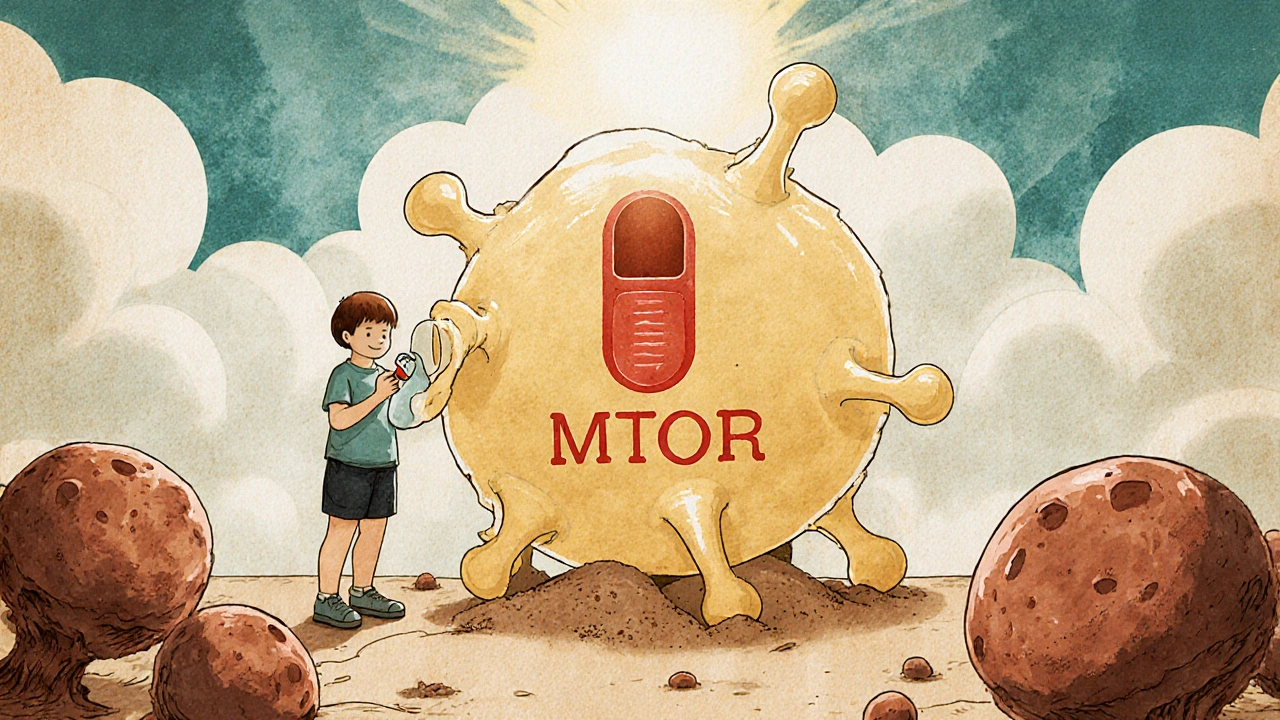
Lymphangioleiomyomatosis often shows up in women with tuberous sclerosis, a genetic disorder that causes benign tumors in multiple organs, but about half of all cases happen without any family history. The disease is tied to mutations in the TSC1 or TSC2 genes, which normally keep cell growth in check. When they fail, cells multiply uncontrollably, forming cysts in the lungs that replace air sacs. This isn’t just about aging or smoking — it’s a biological glitch that hits mostly women between 20 and 40, and it’s often misdiagnosed as asthma or COPD.
One of the biggest red flags is sudden chest pain or shortness of breath, especially if it comes with a collapsed lung (pneumothorax). Many patients have had multiple collapsed lungs before anyone connects the dots to LAM. Fatigue, wheezing, and coughing up blood are also common. Doctors use CT scans to spot the telltale cysts, and lung function tests track how fast the disease is moving. There’s no cure yet, but mTOR inhibitors, a class of drugs that block the overactive cell-growth pathway in LAM — like sirolimus and everolimus — have changed the game. These drugs don’t reverse damage, but they slow it down significantly, helping people keep their lungs working longer.
What you won’t find in most guides is how much lifestyle matters. Oxygen therapy, pulmonary rehab, and avoiding estrogen-heavy birth control can make a real difference. Some patients live for decades with careful management; others decline faster. The key is early detection and sticking with a specialist who’s seen this before. You’re not alone — there are registries, support groups, and clinical trials actively looking for better answers.
Below, you’ll find real-world comparisons of treatments, stories from people managing LAM, and clear breakdowns of what works — and what doesn’t — when it comes to breathing easier, avoiding hospital visits, and staying in control of your health.
Everolimus: How This Drug Is Changing Outcomes for Rare Disease Patients
Everolimus is transforming care for rare diseases like tuberous sclerosis and LAM by targeting abnormal cell growth. It shrinks tumors, improves lung function, and offers hope where few options existed.
Read More