Medicare Drug Coverage: What’s Included, What’s Denied, and How to Fight Back
When you enroll in Medicare drug coverage, the part of Medicare that pays for prescription medications, typically through private plans called Medicare Part D. Also known as Medicare Part D, it’s meant to help you afford the medicines you need — but the reality is often more complicated than the promise. Not every drug is covered, and even if it is, your plan might not pay for the one your doctor prescribed. You could be stuck with a non-formulary generic — a cheaper version of your medication that your plan doesn’t list as approved. That doesn’t mean you’re out of options. It just means you need to know how to ask for help.
Medicare drug coverage is shaped by decisions made by private insurers, not just the government. Plans create lists called formularies — basically, catalogs of drugs they’ll pay for. If your drug isn’t on that list, you’ll pay full price unless you file an exception. That’s where non-formulary generics, generic medications not included in a Medicare Part D plan’s approved list come in. These aren’t bad drugs. They’re often just less popular with insurers because they don’t come with rebates or marketing deals. But if your doctor says you need it, you have rights. Federal rules let you appeal these denials with clinical documentation, and many people succeed. Even more, Medicare drug negotiations, a new federal process allowing Medicare to directly negotiate prices for certain high-cost drugs are starting to change what’s available and how much you pay. This isn’t just about savings — it’s about access.
What you’ll find in the posts below isn’t theory. It’s what real people have dealt with: a denied claim for a blood pressure combo pill, a pharmacist explaining why your insulin isn’t covered, a patient who fought a drug coverage denial and won. You’ll learn how to read your plan’s formulary like a pro, when to use the teach-back method to make sure your doctor understands your coverage limits, and how to spot when a generic switch might require a dose change — because not all generics are equal. Some of these stories are about warfarin, levothyroxine, or antibiotics that lose potency if stored wrong — all things that matter when your coverage is shaky. You’ll see how Indian generic manufacturers, FDA medication guides, and insurance appeals all tie into the same problem: getting the right medicine at a price you can afford. This isn’t about guessing. It’s about knowing your rights, understanding your plan, and speaking up before your health pays the price.
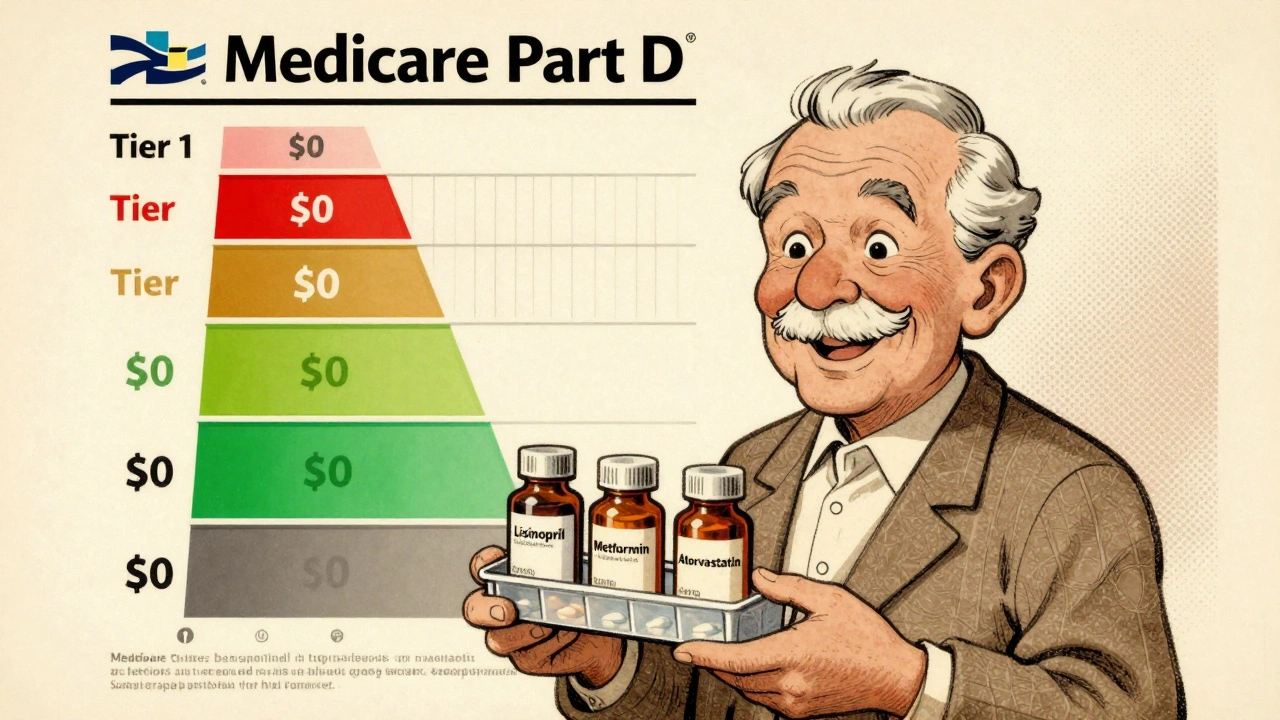
Medicare Part D Formularies: How Generic Coverage Works in 2025
Learn how Medicare Part D covers generic drugs in 2025 - including tiered costs, the $2,000 out-of-pocket cap, and how to save money on your prescriptions.
Read More