When Expired Medications Become Toxic and Dangerous: What You Need to Know
Most people assume that if a pill or liquid medicine is past its expiration date, it’s just weaker-maybe it won’t work as well, but it won’t hurt you. That’s the myth. The truth is more complicated. For the vast majority of medications, expiration means reduced effectiveness, not danger. But for a small group of critical drugs, going past that date isn’t just risky-it can be life-threatening.
What Does an Expiration Date Really Mean?
The expiration date on your medicine isn’t a random guess. It’s the last day the manufacturer guarantees the drug will work as intended and remain safe under proper storage conditions. This requirement became law in the U.S. in 1979, after the FDA started forcing drugmakers to prove their products wouldn’t break down into harmful substances over time. Here’s the twist: the FDA’s own Shelf Life Extension Program, run with the Department of Defense since the 1980s, tested over 100 medications and found that 90% of them were still fully potent 5 to 15 years after their labeled expiration date-when stored correctly. So why do we still throw out pills that might still work? The answer isn’t science. It’s caution. Manufacturers set conservative dates to cover worst-case scenarios: heat, humidity, poor packaging. But for most people, the real danger isn’t the medicine aging-it’s how it’s stored.When Expired Medications Turn Toxic
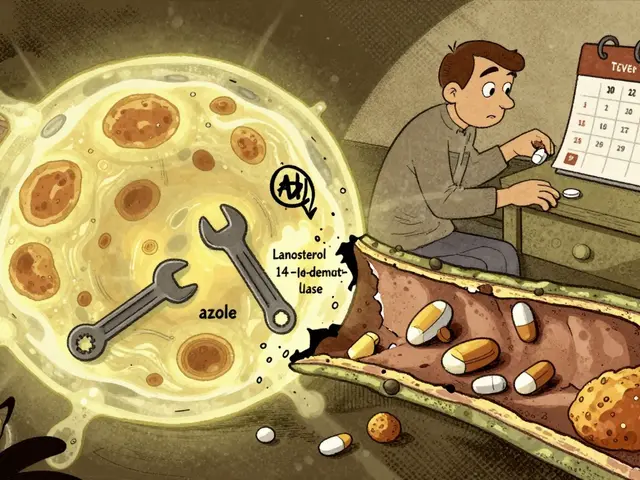
Not all expired drugs are created equal. Most solid pills-like blood pressure meds, antidepressants, or allergy tablets-just lose strength over time. But a few specific medications break down into chemicals that can damage your body. Tetracycline is the classic example. In 1963, three patients developed kidney damage after taking expired tetracycline. The drug degraded into epitetracycline and anhydro-4-epitetracycline-both toxic to the kidneys. This case is still cited today, even though modern packaging and manufacturing have made this far less likely. Still, it’s the only well-documented case of toxicity from an expired antibiotic in over 60 years. Nitroglycerin, used for chest pain, is another high-risk drug. It breaks down quickly into nitrogen oxides, which don’t just make it less effective-they can leave you without any relief during a heart attack. Research from the Cleveland Clinic shows it loses half its potency within three months of expiration. If you’re relying on this for angina, using an expired tablet could mean the difference between life and death. Insulin is equally dangerous. After expiration, it starts forming clumps called fibrils. These clumps don’t just reduce how well the insulin works-they can cause erratic blood sugar spikes and crashes. Studies show insulin can lose 20-30% of its potency each year after expiration. For someone with type 1 diabetes, that’s not a minor inconvenience. It’s a medical emergency waiting to happen. Liquid antibiotics like amoxicillin-clavulanate are risky for two reasons. First, they lose potency fast-sometimes within weeks after opening. Second, they can grow bacteria or form allergenic compounds. One parent reported their child developed severe diarrhea after taking a liquid antibiotic that expired just three days earlier. That’s not just a failed treatment-it’s a reaction to a degraded chemical. EpiPens are the most urgent case. Epinephrine, the life-saving drug inside, degrades rapidly. A 2017 study in the Annals of Internal Medicine found that one year after expiration, EpiPens lost 85% of their potency. If you use one during an allergic reaction and it doesn’t work, you won’t get a second chance.Storage Matters More Than You Think
Your bathroom isn’t a medicine cabinet. It’s a steam room. The FDA says medications should be stored in a cool, dry place-between 59°F and 77°F with 35-45% humidity. The average bathroom? 90°F and 80% humidity. That’s a recipe for degradation. Insulin stored in the fridge stays potent for up to 12 months after opening. Left on the counter? It drops to 70% potency in the same time. Nitroglycerin tablets stored in their original glass bottle with amber protection last longer than those in plastic. Even aspirin isn’t safe-after two years past expiration, it breaks down into acetic acid and salicylic acid, increasing the chance of stomach irritation by 50%. If your medicine smells weird, looks discolored, or feels sticky or crumbly, toss it. That’s not a myth-that’s chemistry.
What’s Safe to Use After Expiration?
The good news? Most of your medicine is probably fine. Solid pills-like ibuprofen, acetaminophen, loratadine, or metformin-often retain 70-90% of their potency even 10 years past expiration if kept in a cool, dark place. The FDA’s SLEP program found that in controlled conditions, these drugs degrade slowly and predictably. Antihistamines like Benadryl? Still effective. Blood pressure meds like lisinopril? Still working. Even some antibiotics in tablet form, like doxycycline, can last years beyond their date. The problem isn’t toxicity-it’s whether they’ll still treat your infection. But here’s the catch: if you’re treating something serious-a heart condition, an infection, an allergy-waiting to see if it works isn’t worth the risk. You don’t want to find out your expired medicine failed when it matters most.Why Do Doctors Still Say ‘Don’t Use Expired Medicines’?
You’ll hear conflicting advice. The FDA, CDC, and DEA all say: never use expired drugs. But pharmacists and researchers often say: it’s mostly safe. Why the disconnect? First, liability. If you take an expired drug and get sick, the doctor or pharmacist could be sued-even if the drug wasn’t the cause. So they err on the side of caution. Second, the real danger isn’t poisoning-it’s treatment failure. A 2023 editorial in JAMA Internal Medicine put it bluntly: “The real tragedy isn’t poisoned patients from expired drugs-it’s the untreated heart attack because expired nitroglycerin didn’t work when needed most.” Third, people don’t store medicine properly. A 2023 Consumer Reports survey found 68% of U.S. adults have used an expired medication. Only 0.3% reported toxicity. But 12% said the medicine didn’t work. That’s the real cost: missed diagnoses, untreated infections, uncontrolled pain.
What Should You Do?
Here’s a simple guide:- Never use expired nitroglycerin, insulin, EpiPens, liquid antibiotics, or eye drops.
- Use with caution if expired for less than a year: blood pressure pills, antidepressants, antihistamines, pain relievers. Check for discoloration or odd smells.
- Throw away anything that looks, smells, or feels wrong-even if it’s within the date.
- Store properly: cool, dry, dark place. Not the bathroom. Not the car. Not the kitchen window.
- Dispose safely: Use a drug take-back program. Walgreens and CVS have drop boxes. The DEA’s National Prescription Drug Take-Back Day collected over 900,000 pounds of expired meds in 2023.
The Bigger Picture: Waste vs. Safety
The U.S. spends $8.2 billion a year replacing expired medications. The FDA’s own data shows most of that waste is unnecessary. The NIH estimates that extending expiration dates for common drugs could save billions and reduce environmental waste. In 2024, the FDA launched a pilot program to extend expiration dates for 20 critical medications based on real-time stability data. Companies like Pfizer and Merck are investing hundreds of millions in smart packaging that tracks how your medicine is stored and adjusts its expiration date automatically. This isn’t about ignoring science. It’s about updating rules to match it. For now, though, the rule is simple: if it’s one of the high-risk drugs, don’t risk it. For everything else, use your judgment-but never assume an old pill will save your life. Better safe than sorry.Can expired medications make you sick?
Most expired medications won’t make you sick-they just won’t work as well. But a few, like expired tetracycline, nitroglycerin, insulin, and liquid antibiotics, can break down into toxic or harmful substances. These cases are rare, but the risks are serious. If you’re unsure, don’t take it.
Is it safe to take expired painkillers like ibuprofen or Tylenol?
Yes, if they’ve been stored properly. Studies show ibuprofen and acetaminophen retain 70-90% of their potency even 10+ years past expiration. But if the pills are cracked, discolored, or smell strange, throw them out. The risk isn’t toxicity-it’s that they won’t relieve your pain.
Why do pharmacies put expiration dates on prescriptions?
Pharmacies put expiration dates on prescriptions for legal and safety reasons. Federal law requires manufacturers to set expiration dates based on stability testing. Pharmacies follow those dates to avoid liability. Even if the drug is still good, the date protects both you and the provider.
What’s the safest way to dispose of expired medicine?
Use a drug take-back program. Many pharmacies like CVS and Walgreens have drop boxes. You can also check for National Prescription Drug Take-Back Day events. Never flush pills or throw them in the trash without mixing them with coffee grounds or cat litter first-this prevents accidental ingestion by kids or pets.
Can I trust the expiration date on over-the-counter medicine?
Yes, but understand what it means. The date is a guarantee of full potency and safety under proper storage. If you’ve kept your medicine in a hot, humid place, it may degrade faster. Always check the appearance and smell. If it looks off, don’t use it-even if it’s within the date.




15 Comments
June Richards
February 1, 2026 at 14:12
I took my grandma's expired ibuprofen last week and my headache vanished 😎😂 who needs pharma profits anyway?
Sami Sahil
February 1, 2026 at 19:51
bro this is so true!! i use expired meds all the time and never had a prob. my mom says i’m gonna die but i’m still here 😎💪
franklin hillary
February 1, 2026 at 21:42
Let’s be real - the FDA doesn’t care if your aspirin works after 12 years. They care about liability. The drug companies set expiration dates so they can sell you the same bottle every 18 months. It’s a business model, not a science. The Shelf Life Extension Program proved it. 90% of drugs still potent decades later. We’re being manipulated to consume. And now they want smart packaging that tracks your humidity? That’s not safety - that’s surveillance capitalism with a stethoscope.
Ishmael brown
February 3, 2026 at 10:28
I’ve got a theory… what if the real danger isn’t the expired meds… but the fact that we’re all so dependent on them? We’ve been trained to panic if a pill’s date passes. Meanwhile, our bodies are perfectly capable of healing… if we just stopped medicating every sneeze. 🤔💊
Nancy Nino
February 3, 2026 at 20:54
I must say, this article was exquisitely researched and presented with a level of academic rigor one rarely encounters in digital media. One does wonder, however, whether the author has ever considered the psychological implications of encouraging laypersons to make pharmacological judgments based on visual inspection. The notion that ‘if it looks off, toss it’ is charmingly naive. What, precisely, constitutes ‘off’? Is that a subjective standard? A clinical one? Or merely a culturally conditioned aversion to discoloration?
Jaden Green
February 3, 2026 at 22:08
Look, I’m not some conspiracy theorist, but let’s be honest - the entire pharmaceutical industry is built on fear. They tell you your aspirin will turn into poison after 2025 so you’ll buy a new bottle. They scare you into ditching insulin because ‘it might not work’ when the real issue is that they don’t want you using the same vial for five years. And don’t even get me started on how they charge $500 for an EpiPen that costs $2 to make. This isn’t medicine. It’s a rent-seeking racket disguised as public health.
Lu Gao
February 5, 2026 at 05:11
I love how people say 'tetracycline is the only documented case of toxicity'... but they forget that 1963 was before modern packaging, storage, and quality control. Today? Almost impossible. But the myth lives on because fear sells. Also, 'don't use expired meds' is the easiest answer for doctors. It's not science - it's laziness with a medical license. 🧪😅
Angel Fitzpatrick
February 5, 2026 at 11:22
You think this is about medicine? Nah. This is a psyop. The government, Big Pharma, and the CDC are all in cahoots to keep you dependent. They don’t want you knowing that pills last 15 years because then you’d stop buying new ones. They’re also using expiration dates to track your consumption habits via pharmacy databases. Your EpiPen isn’t expired - it’s being monitored. The smart packaging? That’s a RFID chip. They’re building a pharmacological surveillance state. You think you’re safe? You’re just another data point in their algorithm.
Donna Macaranas
February 6, 2026 at 07:25
I keep all my meds in a shoebox under my bed. Never had an issue. I mean, I’ve got a 2018 bottle of Zyrtec that still works fine. If it looks like a pill and tastes like a pill, I’m gonna take it. No drama. No panic. Just life.
Rachel Liew
February 8, 2026 at 05:03
i just wanna say thank you for writing this. i’ve been scared to use my dad’s old blood pressure pills and this helps me feel less guilty. i keep them in a drawer, not the bathroom. i’ll keep checking for weird smells. you’re right - it’s not about fear, it’s about being smart. ❤️
Ed Di Cristofaro
February 9, 2026 at 20:20
You people are idiots. If it’s expired, throw it out. End of story. I don’t care if NASA says it’s still good - I’m not risking my life because some guy on Reddit says aspirin lasts 12 years. I’m not your guinea pig.
Melissa Melville
February 10, 2026 at 20:26
So… we’re supposed to trust the FDA’s 1979 rules… but also trust the DoD’s 1980s tests that say it’s fine? Funny how the same government that says ‘don’t use expired meds’ also stores millions of doses for decades in military stockpiles. I guess the real rule is: don’t use expired meds… unless you’re in the military. Then it’s fine. 🤷♀️
Naomi Walsh
February 11, 2026 at 20:44
The entire premise of this article is flawed. You’re treating expiration dates like they’re arbitrary when in fact they’re the product of rigorous stability testing under controlled conditions - conditions that the average person’s bathroom absolutely does not replicate. To suggest that ‘most meds are fine’ is not only scientifically irresponsible, it’s dangerously romanticized. You’re not a pharmacist. You’re not a chemist. You’re just someone who doesn’t want to buy new pills.
Bryan Coleman
February 13, 2026 at 14:18
i used to work at a pharmacy. we used to get calls from people asking if they could use their 3-year-old insulin. we’d say no. then they’d say ‘but my cousin’s dog took expired antibiotics and lived’. we’d say ‘your cousin’s dog isn’t a type 1 diabetic’. it’s not about the pill. it’s about the person. don’t gamble with your health.
Naresh L
February 14, 2026 at 21:17
It’s fascinating how we’ve turned medicine into a ritual of consumption rather than a tool of restoration. We treat expiration dates as sacred texts, yet we ignore the deeper question: why do we need so many pills in the first place? If a drug’s potency declines over time, perhaps the real issue isn’t the shelf life - but the fragility of our own biology. We’ve outsourced healing to chemicals, and now we’re terrified of what happens when those chemicals… age. Maybe the expiration date isn’t on the bottle. Maybe it’s on us.