Autoimmune Overlap: Understanding PBC, PSC, and AIH Combined Features
When your liver starts acting up, it’s easy to assume it’s just one problem. But sometimes, it’s not that simple. A growing number of patients are being diagnosed with something more complex: autoimmune overlap syndromes, where features of two or more autoimmune liver diseases show up at the same time. The most common combinations involve Primary Biliary Cholangitis (PBC), Primary Sclerosing Cholangitis (PSC), and Autoimmune Hepatitis (AIH). These aren’t just rare oddities-they’re real, clinically significant conditions that demand a different approach to diagnosis and treatment.
What Exactly Is an Autoimmune Overlap Syndrome?
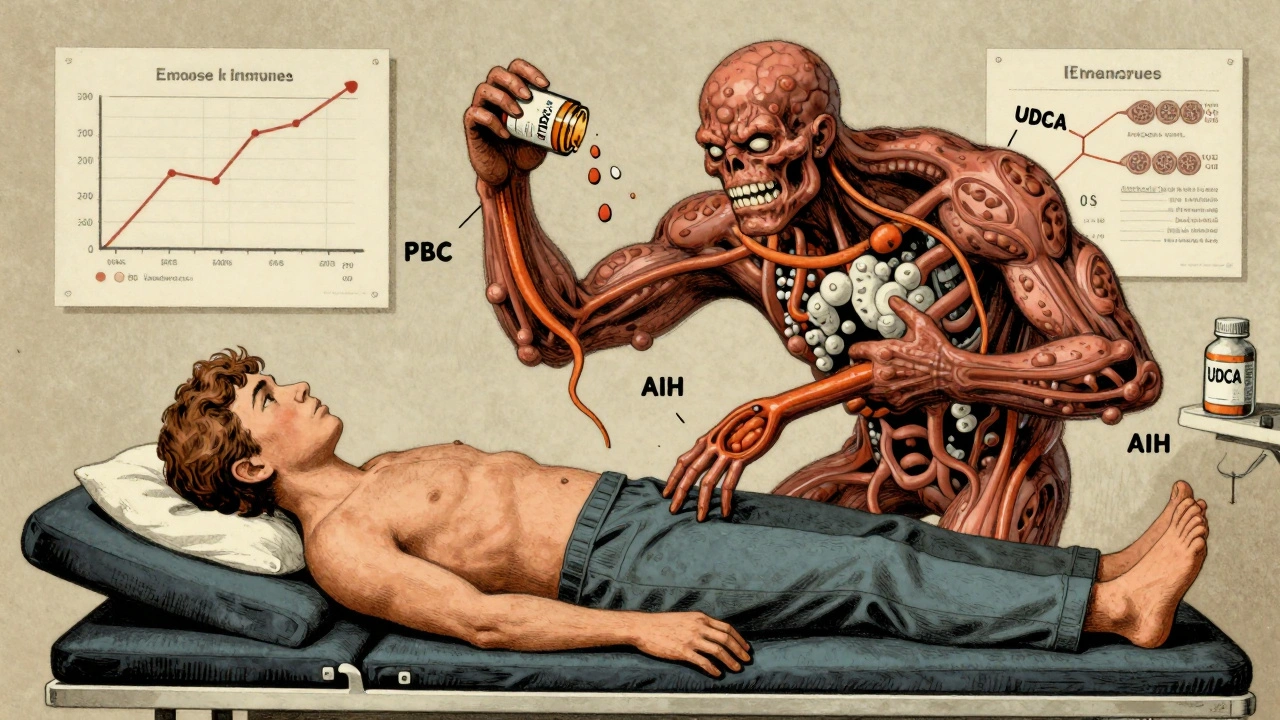
Imagine your immune system gets confused. Instead of attacking just one target, it starts hitting multiple parts of your liver at once. That’s essentially what happens in overlap syndromes. You might have the bile duct damage seen in PBC, the scarring of bile ducts typical of PSC, and the liver cell inflammation characteristic of AIH-all happening together.
This isn’t new. Doctors first noticed these mixed patterns in the 1970s. Back then, they called them "atypical cases." But as testing improved, it became clear these weren’t just random exceptions. They were distinct patterns that needed their own rules. Today, AIH-PBC overlap is the most frequently recognized form. Studies show it occurs in 1% to 3% of people with PBC and up to 7% of those with AIH. Some studies even report numbers as high as 19% among PBC patients. That’s not negligible.
But here’s the catch: PBC and PSC overlap? There’s no solid evidence it truly exists. Some case reports mention it, but experts agree it’s likely a misdiagnosis. The features don’t cleanly combine the way AIH and PBC do. So if you’re hearing about PBC-PSC overlap, be skeptical. The real focus should be on AIH-PBC-and to a lesser extent, AIH-PSC.
How Do These Diseases Differ on Their Own?
To understand overlap, you need to know the baseline. Each disease has its own fingerprint.
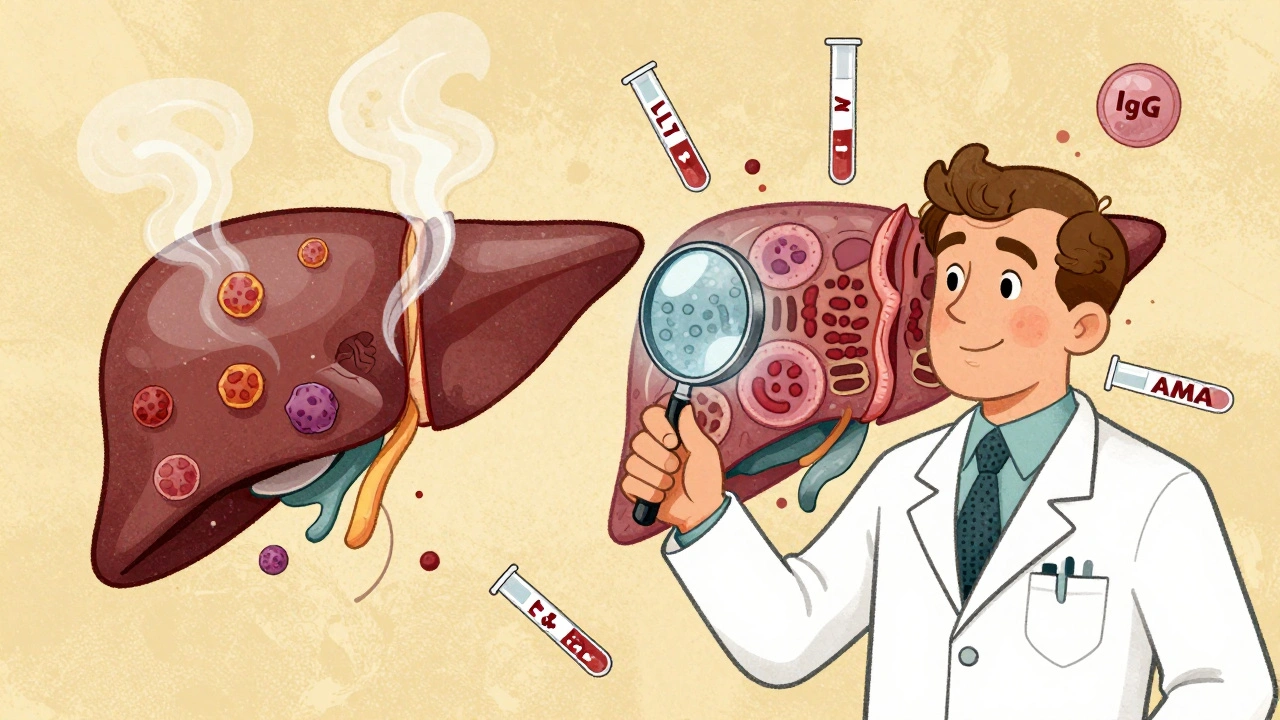
- Autoimmune Hepatitis (AIH) attacks liver cells directly. Blood tests show high ALT and AST-markers of liver cell damage. IgG levels are usually sky-high, and you’ll often see antinuclear antibodies (ANA) or smooth muscle antibodies (SMA). A liver biopsy shows interface hepatitis: immune cells creeping into the liver tissue like invaders.
- Primary Biliary Cholangitis (PBC) targets the small bile ducts inside the liver. That’s why alkaline phosphatase (ALP) and GGT spike. The classic sign? Anti-mitochondrial antibodies (AMA) in 90-95% of cases. IgM levels rise, not IgG. Biopsies reveal damaged bile ducts surrounded by immune cells-a pattern called nonsuppurative destructive cholangitis.
- Primary Sclerosing Cholangitis (PSC) affects larger bile ducts, both inside and outside the liver. ALP and GGT are elevated too, but AMA is negative. PSC patients often have inflammatory bowel disease, especially ulcerative colitis. The hallmark is a "beaded" appearance on imaging, caused by scarring and narrowing of ducts.
Now imagine someone has elevated ALP (PBC sign) AND high ALT (AIH sign). They test positive for AMA (PBC) AND ANA (AIH). Their biopsy shows both bile duct damage AND interface hepatitis. That’s not two diseases. That’s one disease wearing two masks.
How Do Doctors Diagnose an Overlap?
There’s no single test. No magic blood panel. Diagnosis is like putting together a puzzle with pieces from different boxes.
The most widely used framework for AIH-PBC overlap requires meeting at least two of three diagnostic criteria for both diseases:
- For PBC: Elevated ALP, positive AMA (or sp100/gp210 antibodies if AMA-negative), and bile duct damage on biopsy.
- For AIH: Elevated IgG, presence of ANA or SMA, and interface hepatitis on biopsy.
Some patients meet all three for each disease. Others meet two for one and two for the other. That’s still enough to call it overlap. The key is consistency across clinical, lab, and tissue findings.
But here’s where it gets messy. Not every hospital does full antibody panels. Not every doctor orders a biopsy unless the case is obvious. That’s why misdiagnosis happens in 15-20% of cases in community settings. A patient with AIH-PBC might be labeled just as PBC and put on ursodeoxycholic acid (UDCA)-and then keep getting sicker because their liver cells are still being attacked.
That’s why experts say: if you have PBC but your ALT is stubbornly high, or your IgG is climbing, or your biopsy looks "off," don’t ignore it. Dig deeper. Test for ANA and SMA. Look at IgG. Consider the biopsy.
Treatment Isn’t One-Size-Fits-All
This is where overlap syndromes really change the game.
PBC? Standard treatment is UDCA. It slows progression. Works well for most.
AIH? Steroids like prednisone, often paired with azathioprine. Suppresses the immune system’s attack on liver cells.
But if you have both? UDCA alone often isn’t enough. Studies show 30-40% of overlap patients don’t respond to UDCA alone. Their transaminases stay high. Their liver keeps getting damaged. That’s when steroids and immunosuppressants get added.
Some patients start with UDCA and later need steroids when AIH features emerge. Others get both from day one, especially if the biopsy shows clear interface hepatitis. The goal? Stop both the bile duct destruction and the liver cell attack.
And yes-liver transplant is still an option if things spiral. But even after transplant, outcomes can differ. Overlap patients may have higher risks of disease recurrence or complications compared to those with pure PBC or AIH. That’s why long-term follow-up isn’t optional. It’s essential.
What Symptoms Should You Watch For?
These diseases are sneaky. Many people feel fine for years. Fatigue is the big one-constant, crushing tiredness that doesn’t go away with sleep. It’s not just "being busy." It’s like your body’s battery is permanently drained.
Other signs:
- Itchy skin (especially with PBC)
- Jaundice (yellowing of skin or eyes)
- Pain in the upper right abdomen
- Joint pain or muscle aches
- Dry eyes or mouth
Some patients develop other autoimmune conditions too-rheumatoid arthritis, thyroid disease, colitis. That’s another red flag. Your immune system isn’t just targeting your liver. It’s on a rampage.
And here’s something rarely talked about: drug-induced overlap. A case report in 2020 described a patient who developed AIH-PBC after taking hydralazine, a blood pressure medication. Once they stopped the drug, symptoms improved-but the autoimmune damage stuck. That means even medications you think are safe can trigger this.
What’s the Long-Term Outlook?
Left untreated, 30-40% of overlap syndrome patients develop cirrhosis within 10 years. That’s similar to pure PBC or AIH. But here’s the difference: overlap patients often progress faster because they’re getting hit from two angles.
Early diagnosis and dual therapy can change that. Studies show patients who get the right combo of UDCA and immunosuppressants early have much better long-term survival. Their liver enzymes normalize. Fibrosis stabilizes. They avoid transplant.
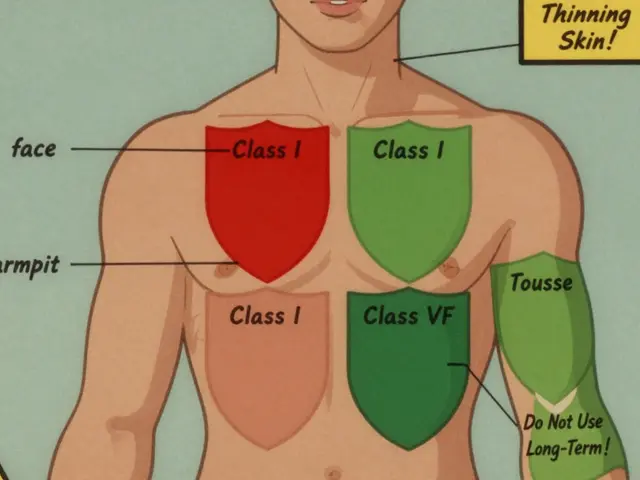
But if you’re misdiagnosed? You might get the wrong treatment. UDCA for AIH? It won’t touch the liver cell inflammation. Steroids for PBC? They help, but they don’t fix bile duct damage. And both carry side effects-weight gain, bone loss, infections. That’s why precision matters.
What’s Next in Research?
Scientists are moving away from thinking of these as separate diseases. Now, they see them as points on a spectrum. AIH, PBC, PSC-they’re all autoimmune liver diseases, just with different targets. Overlap syndromes aren’t anomalies. They’re the natural result of a system that’s lost its way.
New autoantibodies are being identified. Antibodies against sp100 and gp210, for example, help diagnose AMA-negative PBC. These could one day help spot overlap earlier.
Large studies led by the European Association for the Study of the Liver and the International Autoimmune Hepatitis Group are working to validate diagnostic criteria. Expected results? By 2025, we may have clearer guidelines-so doctors everywhere can spot overlap faster and treat it right.
One thing’s certain: if you have liver disease and something feels "off," speak up. Ask about antibody tests. Ask about biopsy. Don’t settle for a simple label if your numbers don’t add up. Your liver doesn’t care about neat categories. It just wants to be protected.
Can you have PBC and PSC at the same time?
While there are rare case reports, there’s no strong evidence that a true PBC-PSC overlap syndrome exists. The features of these two diseases don’t reliably combine. Most experts believe cases labeled as PBC-PSC overlap are either misdiagnosed or represent a different underlying condition. The only well-documented overlap syndromes involve AIH combined with either PBC or PSC.
Is autoimmune overlap syndrome rare?
It’s not extremely rare. AIH-PBC overlap occurs in 1-3% of PBC patients and up to 7% of AIH patients. Some studies report rates as high as 19% in PBC populations. That’s far more common than most people realize. Many cases go undiagnosed because doctors don’t test for both sets of markers or skip liver biopsies.
Do I need a liver biopsy if I have PBC?
Not always-but if your ALT is high, your IgG is elevated, or you have symptoms that don’t match typical PBC, a biopsy is critical. It’s the only way to confirm interface hepatitis, which is the hallmark of AIH. Without it, you might miss an overlap syndrome. Guidelines recommend biopsy when the diagnosis is uncertain or treatment response is poor.
Can medications cause autoimmune overlap?
Yes. There are documented cases where drugs like hydralazine triggered AIH-PBC overlap. The immune system can be fooled into attacking the liver after exposure to certain medications. If you develop liver enzyme abnormalities after starting a new drug, especially with multiple autoimmune markers, it’s worth considering drug-induced overlap.
What’s the difference between AIH-PBC and just having two separate diseases?
It’s not two diseases coexisting-it’s one immune system attacking the liver in two different ways at the same time. In true overlap, the same immune response causes both bile duct damage and liver cell inflammation. That’s why treatment needs to target both pathways. If you had two separate diseases, you’d expect different patterns of progression and response to therapy.





10 Comments
David Palmer
December 11, 2025 at 00:38
So you're telling me my liver's just confused? Like it forgot which part to hate? Cool. I'll just sit here and let it figure it out.
Michaux Hyatt
December 11, 2025 at 03:35
Hey, this is actually super helpful! I’ve been chasing answers for my sister’s weird liver numbers for months. The part about ALT staying high while on UDCA? That’s *exactly* what her docs ignored. Thanks for laying out the antibody combos - I’m printing this to take to her hepatologist tomorrow. You’re a lifesaver.
Aileen Ferris
December 12, 2025 at 21:10
aih-pbc overlap? more like aih-pbc ovelap 😂 i mean, come on. if you can’t spell it right, how can you trust the science? also, who even made up these acronyms? they sound like bad sci-fi villains.
Nikki Smellie
December 13, 2025 at 21:30
Did you know the pharmaceutical companies invented autoimmune overlap syndromes to sell more drugs? 😏 They need you to believe you have TWO diseases so they can prescribe BOTH treatments - and charge triple. AMA? ANA? All manufactured by Big Pharma to keep you hooked. The real cause? 5G towers + fluoridated water. Ask your doctor why they never mention this.
Michelle Edwards
December 15, 2025 at 09:54
I know how overwhelming this can feel - if you’re reading this and you’re newly diagnosed or confused, you’re not alone. Small steps matter. Ask for the biopsy. Ask for the full antibody panel. Even if your doctor says ‘it’s probably just PBC,’ your body is talking. Listen. You’ve got this. One test at a time.
Sarah Clifford
December 15, 2025 at 23:10
so like… my liver is having an identity crisis?? and now i have to take TWO types of pills?? i just wanted a nap and a burrito. why is everything so complicated now?? 😭
Regan Mears
December 17, 2025 at 03:37
Thank you for writing this with such clarity. I’ve been reading everything I can since my diagnosis last year - and this is the first time someone made sense of the overlap without jargon overload. The part about ‘one immune system attacking in two ways’? That’s the missing piece. I’ve been on UDCA for 18 months and my AST kept climbing. My doctor finally agreed to a biopsy after I showed him this. Turns out - interface hepatitis. We’re adding prednisone next week. I’m terrified… but also, finally hopeful.
Ben Greening
December 17, 2025 at 20:04
Interesting overview. The diagnostic criteria for AIH-PBC overlap remain inconsistently applied across institutions. While the International Autoimmune Hepatitis Group guidelines provide a framework, real-world practice varies widely. Biopsy interpretation, in particular, remains subjective. This may explain the wide variance in reported prevalence figures - from 1% to 19%. Further standardization is needed.
Neelam Kumari
December 18, 2025 at 02:49
Wow. So you're telling me someone actually *wrote* a whole article about this? And people pay doctors to read it? What a waste of time. If your liver is messed up, drink lemon water and stop stressing. Or just get a transplant. Problem solved. 🙄
Queenie Chan
December 19, 2025 at 12:44
It’s wild how the liver’s like a silent poet - screaming in enzymes and antibodies, but no one listens until the damage is baked into the architecture. I love how you framed overlap as not a glitch, but a symphony of immune missteps. It’s not two diseases dancing - it’s one broken heart trying to love two things at once, and getting punished for it. And the drug-induced cases? That’s the haunting twist. Like your own medicine turning traitor. I wonder if we’ll one day map these autoantibodies like constellations - each one a star in the chaos of our immune sky.