High-Alert Drugs: What They Are, Why They Matter, and Which Ones Can Hurt You
When we think of medicine, we assume it’s safe—especially when prescribed by a doctor. But some drugs are so powerful, so risky, that even a small mistake can lead to death. These are called high-alert drugs, medications with a high risk of causing serious harm if used incorrectly. Also known as dangerous drugs, they’re not rare—they’re in hospitals, pharmacies, and homes across the country, and many people don’t even know they’re taking one. The Institute of Medicine found that medication errors injure over a million Americans every year, and high-alert drugs are behind a huge chunk of those cases. It’s not always the doctor’s fault, or the pharmacist’s. Sometimes it’s a misread label, a confusing dose, or a mix-up with another pill that looks similar. The truth? You don’t need to be a medical professional to help prevent these mistakes—you just need to know what to look for.
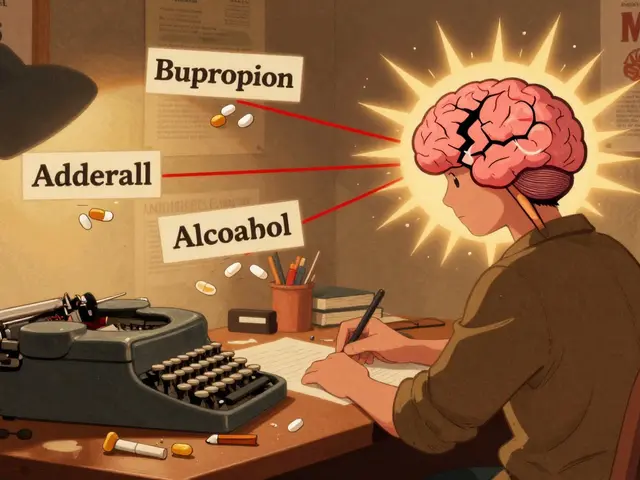
Some of the most common high-alert drugs, medications with a high risk of causing serious harm if used incorrectly include insulin, blood thinners like warfarin, opioids like morphine, and IV potassium. These aren’t just any pills—they’re the kind that can drop your blood sugar to dangerous levels, cause a stroke, stop your breathing, or trigger cardiac arrest if given wrong. Even something as simple as licorice, a common herbal supplement that can interfere with blood pressure medications can turn a routine treatment into a crisis. Or consider DPP-4 inhibitors, diabetes drugs linked to severe joint pain and FDA warnings. They’re not labeled as high-alert, but their side effects can be just as life-changing. And then there’s zidovudine, an early HIV drug that saved lives but carried heavy side effects—a reminder that even life-saving drugs carry hidden risks if not monitored closely.
What ties these together isn’t just their strength—it’s how easily they’re misunderstood. A patient might take two painkillers thinking they’re different, not realizing both contain acetaminophen. Someone on blood pressure meds might eat licorice daily, unaware it’s canceling out their treatment. A caregiver might misread a syringe label and give ten times the insulin dose. These aren’t accidents caused by carelessness—they’re failures in communication, labeling, and education. That’s why knowing the names, the risks, and the red flags matters. You don’t need to memorize a list. You need to ask: Is this drug on the high-alert list? What happens if I take too much? What should I avoid mixing it with?
The posts below cover real cases where these drugs caused harm—and how people fought back. You’ll find guides on spotting dangerous interactions, understanding FDA warnings, and protecting yourself when you’re on multiple medications. Whether you’re managing diabetes, treating pain, or caring for someone with HIV or epilepsy, this isn’t just about knowing the names of drugs. It’s about knowing when to pause, ask questions, and demand clarity. Because with high-alert drugs, ignorance isn’t just risky—it’s deadly.
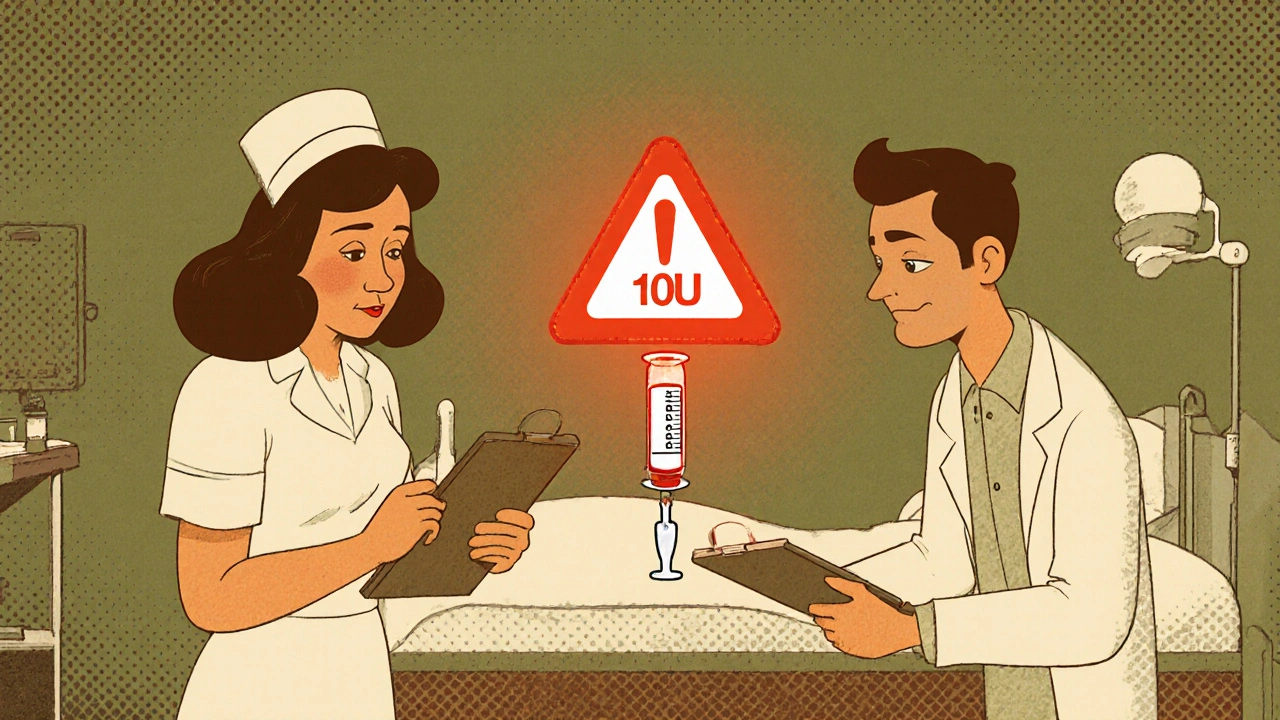
How to Verify Dose Changes and Avoid Miscommunication in Healthcare
Learn how to verify medication dose changes safely using proven protocols like independent double checks, SBAR communication, and targeted barcode scanning to prevent deadly errors in healthcare settings.
Read More