Severe Pancreatitis from Medications: Warning Signs and Treatment
Medication Risk Checker for Severe Pancreatitis
Check if your current medications may put you at risk for severe pancreatitis. Select the medications you're taking below. We'll identify high-risk medications and provide guidance on next steps.
Your Medication Risk Assessment
When you take a new medication, you expect relief-not a life-threatening reaction. But for some people, common prescriptions can trigger severe pancreatitis, a dangerous inflammation of the pancreas that can turn deadly in days. Unlike gallstones or alcohol, which are the usual suspects in pancreatitis, drug-induced cases fly under the radar. They don’t come with obvious red flags. By the time symptoms hit, it’s often too late. The good news? If caught early, stopping the drug can reverse it. The bad news? Most doctors don’t think of it until it’s advanced.
What Exactly Is Drug-Induced Severe Pancreatitis?
Severe pancreatitis isn’t just bad stomach pain. It’s when the pancreas starts digesting itself, triggering massive inflammation, tissue death, and organ failure. In drug-induced cases, this happens because a medication messes with the pancreas-either by poisoning its cells, triggering an immune reaction, or blocking its ducts. The result? Blood tests show lipase levels three times higher than normal. CT scans reveal dead tissue. Patients fight for breath, their bodies in full-blown crisis.
It’s rare-only 1.4% to 3.6% of all acute pancreatitis cases-but when it happens, it’s serious. About 20% of these drug-triggered cases turn severe, with mortality rates between 15% and 30%. That’s higher than gallstone-related severe pancreatitis. And unlike alcohol damage, which builds slowly, drug-induced cases can explode after just a few weeks on a medication-even one you’ve taken for years.
Which Medications Are Most Likely to Cause It?
Not every drug causes this. But eight classes have strong evidence linking them to severe pancreatitis. These aren’t obscure chemicals-they’re everyday prescriptions.
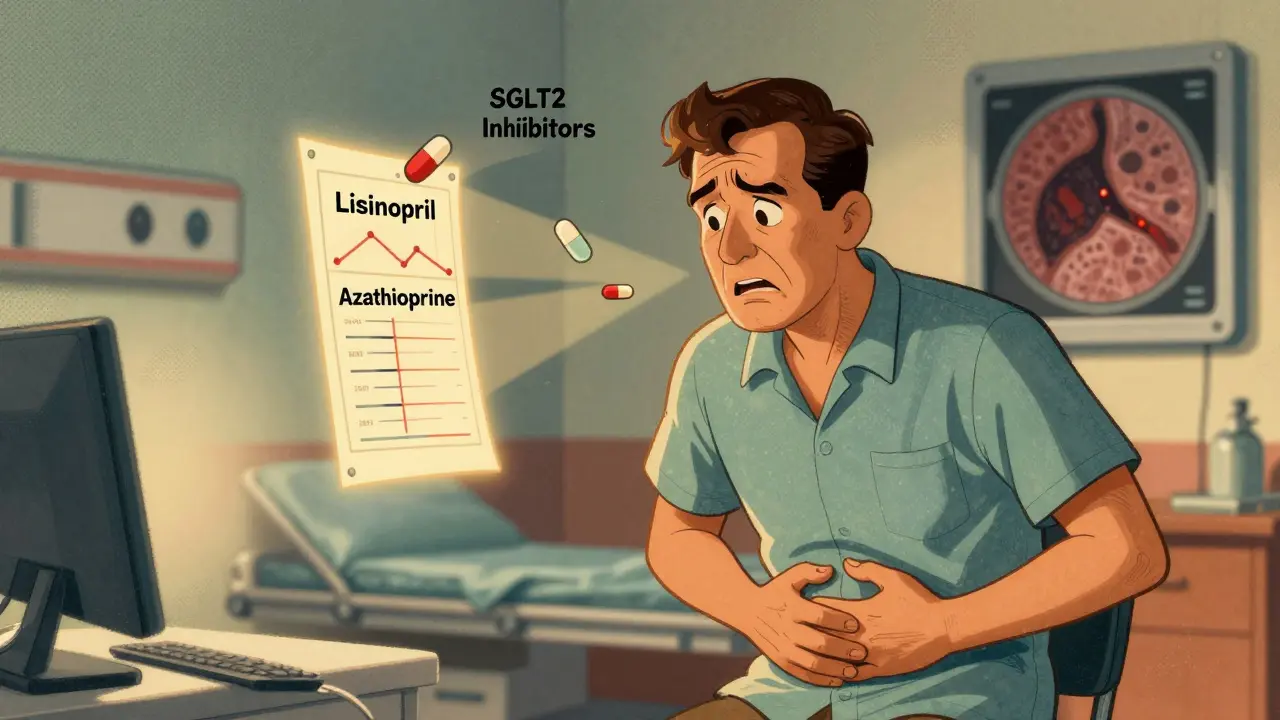
- ACE inhibitors like lisinopril and enalapril-used for high blood pressure
- Diuretics like furosemide and hydrochlorothiazide-commonly prescribed for swelling or fluid retention
- Antidiabetic drugs such as exenatide (Byetta) and sitagliptin (Januvia)-especially after the FDA added black box warnings in 2021
- Statins like simvastatin and atorvastatin-even people on them for years can suddenly develop it
- Valproic acid-used for seizures and bipolar disorder, with up to 22% of users developing necrotizing pancreatitis
- Azathioprine-a key drug for Crohn’s disease and autoimmune conditions, linked to 18% severe cases
- Oral contraceptives with ethinyl estradiol-rare, but documented in younger women
- SGLT2 inhibitors like canagliflozin and dapagliflozin-newer diabetes drugs with a 4.3-fold spike in pancreatitis reports since 2022
What’s scary is how long it can take. One woman on lisinopril for six years developed severe pain and was hospitalized with lipase levels over 1,200 U/L. Her doctor didn’t connect the dots until after she’d spent five days in the hospital. Another patient on azathioprine for Crohn’s had pain dismissed as ‘gastritis’-by the time they scanned her pancreas, 40% of it was dead.
Warning Signs You Can’t Ignore
The pain doesn’t come on like a stomach bug. It’s different.
- Deep, constant upper abdominal pain-often radiating straight through to your back
- Pain that wakes you up at night-not relieved by antacids or position changes
- Nausea and vomiting that won’t stop, even after hours
- Fever above 38°C (100.4°F) with a racing heart (over 90 bpm)
- Swollen or tender abdomen-you can’t touch it without flinching
These symptoms usually appear 7 to 14 days after starting the drug, but sometimes it takes months. That’s why many miss it. If you’re on any of the high-risk medications above and develop new, persistent pain-don’t wait. Don’t assume it’s indigestion. Demand a lipase test. Blood tests for amylase are less reliable. Lipase is the real indicator.
How Doctors Diagnose It
There’s no single test that says, ‘This drug caused it.’ Diagnosis is a puzzle.
First, they rule out gallstones, alcohol use, high triglycerides, and genetic causes. Then they look at timing. If your symptoms started within four weeks of beginning a new medication-and improved within eight weeks of stopping it-that’s considered ‘probable.’ If you took the drug again and got sick again? That’s ‘definite.’ But no doctor will rechallenge you. It’s too risky.
Imaging is critical. A contrast-enhanced CT scan shows if there’s necrosis-dead tissue. If more than 30% of the pancreas is damaged, it’s classified as severe. Blood tests will show elevated lipase, plus signs of organ failure: low blood pressure, low oxygen, high white blood cell count. The Revised Atlanta Classification system is the standard used in hospitals today.
Here’s the catch: up to 40% of reported drug cases might be coincidence. Statins are taken by millions. Some people will get pancreatitis anyway. But when the timing matches, the risk goes up. And if you’re older, on five or more medications, or have a history of autoimmune disease-you’re at higher risk.
How It’s Treated-Step by Step
There’s no magic pill. Treatment is aggressive, fast, and focused on three things: stopping the drug, supporting the body, and preventing death.
- Stop the medication immediately-within 24 hours of suspicion. Delaying increases complications by 37%.
- Aggressive IV fluids-250 to 500 mL per hour for the first 24 to 48 hours. This keeps blood flowing to the pancreas and prevents organ shutdown. Doctors monitor hematocrit to keep it between 35% and 44%.
- Pain control-start with IV acetaminophen. If that’s not enough, use morphine in small doses (2-4 mg every 2-3 hours). Avoid meperidine-it’s outdated and risky.
- Feed the gut, not the IV-if you can’t eat, get nutrition through a tube placed into the small intestine (nasojejunal). Start within 48 hours. Starving the pancreas doesn’t help. Feeding it gently does.
- Antibiotics only if infected-don’t use them unless there’s confirmed necrosis with infection. Meropenem is the go-to if needed.
Most patients need to stay in the hospital for 5 to 10 days. Severe cases can mean weeks in the ICU. But here’s the hopeful part: if you stop the drug early, 65% to 75% of people recover fully. No permanent damage. No lifelong restrictions.
Why This Is Getting Worse
Drug-induced pancreatitis is rising. Why?
More people are on more drugs. The average patient over 60 takes 5.2 medications. Many are on statins, blood pressure pills, and diabetes drugs-all on the high-risk list. The FDA recorded over 4,200 drug-linked pancreatitis cases in 2022-up nearly 13% from the year before. SGLT2 inhibitors alone saw an explosion in reports.
Hospitals are waking up. Since 2021, CMS stopped paying for severe pancreatitis cases deemed preventable. So now, 78% of U.S. academic hospitals use automated alerts in electronic records. If you’re on azathioprine and your chart shows abdominal pain? The system flags it. That’s saving lives.
Research is moving fast too. The NIH launched the Drug-Induced Pancreatitis Registry in January 2023. So far, 317 patients are enrolled. Scientists are working on a genetic test to screen for TPMT mutations before prescribing azathioprine-those with the mutation have a 30x higher risk.

What You Can Do Right Now
If you’re on any of the high-risk medications:
- Know the symptoms. Don’t brush off persistent upper abdominal pain.
- Ask your doctor if your meds are on the list. Many don’t know.
- Keep a symptom journal. Note when pain started, what you were taking, and how it changed.
- If you have pain, demand a lipase test-not just amylase. Lipase is more accurate.
- If you’re on azathioprine, valproic acid, or SGLT2 inhibitors, talk to your doctor about genetic testing or alternatives.
Don’t wait for a crisis. One patient on Reddit said it best: ‘I thought it was heartburn. I almost died because no one thought to check my lipase.’
When to Seek Emergency Help
Go to the ER immediately if you have:
- Pain that lasts more than 24 hours
- Pain that radiates to your back
- Fever, rapid heartbeat, or trouble breathing
- Vomiting that won’t stop
Bring a list of all your medications-including supplements and over-the-counter drugs. Many people forget things like fish oil, vitamin E, or herbal products. Some of those can trigger it too.
Can you get pancreatitis from taking a medication for years?
Yes. Drug-induced pancreatitis isn’t limited to new prescriptions. People on statins, ACE inhibitors, or azathioprine for years can suddenly develop it. There’s no set timeline-it can happen after weeks, months, or even years of use. The key is new or worsening symptoms, not how long you’ve been on the drug.
Is pancreatitis from drugs always permanent?
No. In fact, most cases resolve completely if the medication is stopped early. About 65% to 75% of mild-to-moderate cases fully recover with no lasting damage. Even severe cases can improve significantly if treated fast. The pancreas has a strong ability to heal-unless there’s extensive necrosis or repeated episodes.
What’s the difference between lipase and amylase tests?
Both are enzymes released by the pancreas during inflammation. But lipase stays elevated longer and is more specific to the pancreas. Amylase can rise from other issues like salivary gland problems or kidney failure. For diagnosing pancreatitis, lipase is the gold standard. Doctors should always check lipase first.
Can I restart the medication if my symptoms go away?
Never restart a drug that caused severe pancreatitis. Even if you feel fine, the risk of recurrence is extremely high-and the second episode is often worse. Your doctor will find a safe alternative. For example, if lisinopril caused it, they’ll switch you to a different class of blood pressure medicine like a calcium channel blocker.
Are there any natural remedies or diets that help?
No. There’s no diet, supplement, or herbal remedy that treats severe drug-induced pancreatitis. In fact, some supplements like high-dose vitamin E or fish oil have been linked to pancreatitis themselves. Treatment requires medical intervention: IV fluids, pain control, and feeding support. Home remedies can delay care and worsen outcomes.
Can this happen to young people?
Yes. While most cases occur in people over 60 due to polypharmacy, younger people aren’t immune. Women on oral contraceptives, teens on valproic acid for seizures, and young adults on azathioprine for Crohn’s disease have all developed severe pancreatitis. Age isn’t a shield-medication use is the risk factor.
What Comes Next
The future is about prevention. Genetic screening before prescribing azathioprine. Real-time alerts in hospital systems. Better labeling on drug inserts. But until then, your best defense is awareness. If you’re on a medication and feel something’s off-especially persistent pain-speak up. Push for a lipase test. Don’t let a routine prescription become a life-threatening event.





12 Comments
Robert Way
January 15, 2026 at 17:05
so i was on lisinopril for 3 years and one day my stomach felt like someone was stabbing me from inside and i just thought i ate bad tacos lol
turned out my lipase was 1400 and i was in the hospital for a week
doc said it was the med but i had to beg for the test
why dont they just put warnings on the bottles like cigarettes??
Sarah Triphahn
January 16, 2026 at 02:54
of course the system ignores this until you're half-dead
pharma makes billions on these drugs and doctors are too busy scrolling through their phones to connect the dots
it's not negligence, it's profit-driven ignorance
you think they care about your pancreas? they care about your insurance co-pay
they'll give you a pill for pain but won't stop the pill causing it
this is capitalism in action: sick people = more prescriptions
the real tragedy? you'll get better, go back on another med, and do it all over again
they'll just swap one killer drug for another
you're not a patient, you're a revenue stream
Jason Yan
January 16, 2026 at 07:43
hey, i just want to say this post is seriously important
i've been on statins for 8 years and never thought about pancreatitis
but after reading this, i went to my doctor and asked for a lipase test just to be safe
turns out mine was normal, but we talked about alternatives just in case
you know what? that's the whole point
you don't need to be sick to ask questions
your body talks to you, you just have to listen before it screams
if you're on any of these meds, don't wait for the pain to wake you up at 3am
take 5 minutes today and write down everything you're taking
then ask your doc: could any of these be hurting me?
it's not paranoia, it's self-care
and yeah, i know it's scary to think your meds might be dangerous
but the truth is, sometimes the thing meant to help you is quietly hurting you
and that's okay
you're not weak for asking
you're smart for listening
shiv singh
January 17, 2026 at 05:26
you people are so naive
they know this happens
they just don't care
the FDA is a joke
pharma owns them
your doctor gets kickbacks
your insurance wants you on pills, not healthy
you think this is an accident?
no
it's business
you're a walking wallet
and you're paying for it
with your organs
with your sleep
with your life
stop being a victim
start being angry
Sarah -Jane Vincent
January 18, 2026 at 01:16
ok but have you considered that maybe it's not the drugs?
maybe it's your gut biome?
or your stress?
or the fact that you're drinking almond milk and eating gluten-free bread and now your body is confused?
or maybe you're just a hypochondriac who googles symptoms at 2am?
every time someone says 'my med gave me pancreatitis' it's always the same thing
they never mention their 7 energy drinks a day
or their 3-hour Netflix binges
or their 400mg of ashwagandha they take with their 12 other supplements
the real culprit? modern life
not lisinopril
your lifestyle is killing you
not the pharmacy
Henry Sy
January 18, 2026 at 13:33
bro i was on sitagliptin for 11 months
one morning i woke up and my stomach felt like a warzone
threw up for 14 hours straight
went to er, they gave me omeprazole and sent me home
i came back 3 days later with jaundice
they finally did the lipase test
levels were off the charts
they pulled me off the drug and i was fine in 3 weeks
but now i'm scared to take anything
i just stare at my pill bottle like it's a snake
what if the next one kills me too?
they don't even tell you this stuff on the commercials
they show people hiking and laughing
not lying on a hospital bed screaming
Dylan Livingston
January 19, 2026 at 14:54
how quaint
you treat medical advice like a Reddit thread
as if a blog post with bullet points replaces 8 years of med school
you think a lipase test is some magic wand?
do you know how many things elevate lipase?
bowel obstruction
renal failure
salivary gland tumors
even a good cry can raise it
and you're just going to stop your blood pressure med because some guy on the internet said so?
your pancreas doesn't care about your outrage
it cares about evidence-based medicine
and if you're not a board-certified gastroenterologist, shut up and take your pills
and stop giving people dangerous ideas
you're not a doctor
you're a viral content consumer
Andrew Freeman
January 19, 2026 at 17:31
my uncle died from this
he was on valproic acid for 12 years
they said it was 'gallbladder issues'
he went to 3 different docs
no one checked lipase
he was 54
they buried him in a week
now i check my own labs
if i'm on a new med i ask for lipase before i even take the first pill
no one ever said no
they just looked at me weird
but i'm alive
and i'm not gonna be another statistic
says haze
January 20, 2026 at 18:23
the real issue isn't the drugs
it's the epistemic collapse of medical authority
we've replaced clinical judgment with algorithmic triage
and now patients are forced to become amateur diagnosticians
but the irony? the very systems meant to protect us-electronic health records, automated alerts-are underfunded, poorly implemented, and often ignored
so we're left with this
a Reddit post as our last line of defense
how tragic
that the most vulnerable among us must become amateur epidemiologists
to survive a system designed to keep them docile
and yet
we're told to trust the experts
while the experts are too busy coding CPT codes to look up
the very names of the drugs that are killing us
Alvin Bregman
January 22, 2026 at 02:02
i live in a small town
our doctor is one guy who does everything
he prescribes blood pressure meds, diabetes meds, antibiotics, you name it
he doesn't even have a specialist on call
so when my neighbor got sick from her statin
he didn't know what to do
he just said 'maybe cut back on the cheese'
we need more specialists
and better training
not just for doctors
but for everyone who takes meds
because we're all just trying to get better
and no one told us it could kill us
Anna Hunger
January 23, 2026 at 11:56
As a registered nurse with over 15 years of experience in critical care, I have witnessed firsthand the devastating impact of drug-induced pancreatitis. The clinical presentation is often subtle, and the delay in diagnosis can be fatal. I commend the author for highlighting the critical importance of lipase testing and early intervention. In our unit, we now have a mandatory checklist for patients on high-risk medications, and we routinely educate patients on the warning signs. Knowledge is power, and this information could very well save a life. Please share this with your healthcare providers and loved ones. This is not alarmism-it is advocacy.
Vicky Zhang
January 24, 2026 at 19:29
i just want to say thank you for posting this
i'm 28 and on exenatide for type 2 diabetes
i've had weird stomach pain for 3 weeks
i thought it was stress or my new keto diet
but after reading this
i called my doctor today
and asked for a lipase test
she said yes right away
and i'm getting it tomorrow
i don't want to be the person who almost died because i didn't ask
i'm scared
but i'm doing something
and that's better than waiting
thank you for giving me the courage to speak up