Liquid Antibiotics: What They Are, When They're Used, and What You Need to Know
When you or your child can’t swallow a pill, liquid antibiotics, a liquid form of antibiotic medication designed for easy swallowing and precise dosing. Also known as antibiotic suspension, it’s one of the most common ways to deliver antibiotics to people who need accurate, adjustable doses—especially young children, older adults, or those with swallowing issues. These aren’t just crushed pills mixed with water. They’re specially formulated suspensions with flavoring, stabilizers, and precise concentrations so each milliliter delivers exactly the right amount of medicine.
Liquid antibiotics are often used for pediatric antibiotics, antibiotic treatments specifically designed for infants and children, because kids rarely take pills reliably. Think of amoxicillin for ear infections or cephalexin for strep throat—both come in sweetened suspensions that taste better than you’d expect. But adults use them too, especially after surgery, during recovery from illness, or when they have trouble swallowing due to neurological conditions or throat issues. The key advantage? You can tweak the dose down to the milliliter, which matters when treating small bodies or adjusting for kidney or liver function.
Not all antibiotics come in liquid form, and not every liquid version works the same. Some need refrigeration, others can sit at room temperature. Some must be shaken well before each use—skip that step, and you might get too little or too much medicine. You also need to pay attention to expiration dates. Once mixed, many liquid antibiotics only last 7 to 14 days, even if the bottle says otherwise. Using expired liquid antibiotics doesn’t just mean the treatment won’t work—it could lead to antibiotic resistance or worse, a relapse that’s harder to treat.
There’s a reason antibiotic dosing, the precise measurement of antibiotic quantity based on weight, age, and infection severity is such a big deal. A child’s dose isn’t just a smaller version of an adult’s—it’s calculated by weight in kilograms. Too little and the infection won’t clear. Too much and you risk side effects like diarrhea, yeast infections, or even liver stress. That’s why the pharmacy label matters so much. If you’re unsure how much to give, ask. Don’t guess. Don’t use kitchen spoons. Use the measuring cup or syringe that comes with the bottle.
Some people avoid liquid antibiotics because they taste bad or think they’re less powerful than pills. That’s a myth. The effectiveness isn’t about form—it’s about the active ingredient and whether it’s absorbed properly. In fact, for some infections, liquid forms are preferred because they’re absorbed faster in the gut. But they’re not always the best choice. If you can swallow a pill and the antibiotic comes in tablet form, that’s often the more stable, longer-lasting option. Liquid versions are for when swallowing isn’t an option, not when it’s just inconvenient.
What you’ll find in the posts below isn’t just a list of liquid antibiotics. It’s real-world guidance on how to use them safely, how to spot interactions, and how to avoid common mistakes that lead to treatment failure. You’ll see how patient advocacy changed antibiotic access, how to verify doses when switching pharmacies, and why some people react badly to certain antibiotic families. Whether you’re giving medicine to a toddler, helping an elderly parent, or just trying to understand your own prescription, these posts give you the practical, no-fluff details you need to get it right.
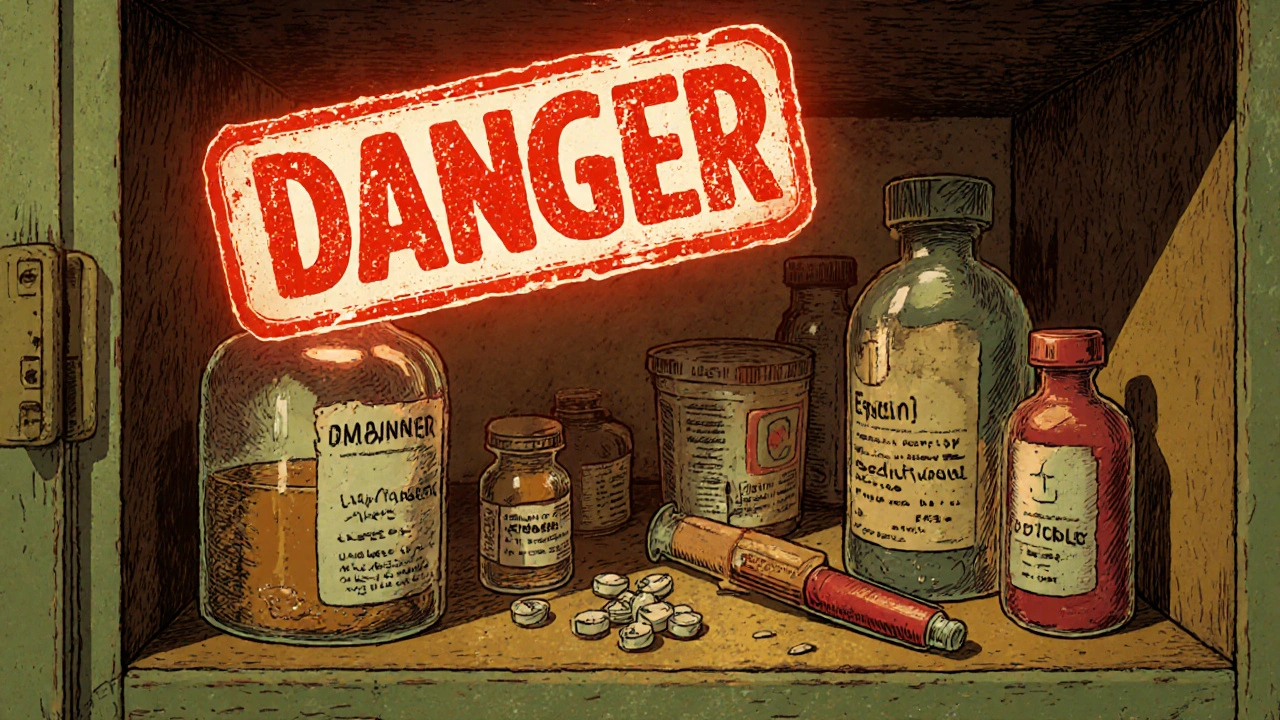
Medications You Should Never Use After the Expiration Date
Some medications lose potency after expiration, but others can become dangerous. Learn which drugs you should never use past their expiration date-including insulin, epinephrine, and liquid antibiotics-and how to store and dispose of them safely.
Read More