Medication Miscommunication: How Errors Happen and How to Stop Them
When you take a pill, you expect it to help—not hurt. But medication miscommunication, a breakdown in how drug information is shared between patients, doctors, and pharmacies happens more often than you think. It’s not always a mistake in the prescription. Sometimes it’s a pharmacist missing a warning, a patient forgetting to mention they take licorice daily, or a doctor not knowing a patient’s full drug history. This isn’t theoretical. People end up in the ER because their blood pressure meds stopped working after eating licorice, or their diabetes drug caused joint pain no one warned them about. These aren’t rare side effects—they’re red flags ignored because the system doesn’t connect the dots.
Drug interactions, when one medication changes how another works in your body are a major part of this problem. Licorice can make blood pressure meds useless. DPP-4 inhibitors like Januvia can trigger severe joint pain. Even something as simple as switching pharmacies without giving the full list of meds can lead to dangerous repeats or missing critical alerts. And it’s not just about pills—natural remedies like herbal supplements often get left out of the conversation, even though they can interfere with everything from HIV drugs to anticoagulants. Prescription errors, mistakes in dosage, timing, or drug choice don’t just come from handwriting or typos. They come from rushed appointments, unclear labels, and patients afraid to ask questions.
That’s why pharmacy transfer, the process of moving your prescriptions from one pharmacy to another isn’t just paperwork. It’s a safety checkpoint. If you don’t give your new pharmacy your complete list—including over-the-counter meds and supplements—you’re leaving gaps that could cost you your health. And when you’re on something like zidovudine or Combivir for HIV, or everolimus for a rare disease, missing a single detail can mean the difference between control and crisis.
The good news? You don’t have to wait for the system to fix itself. You can be the one who asks, “What does this interact with?” or “Could this cause side effects I haven’t noticed?” You can write down every pill you take—every day—and bring that list to every appointment. You can double-check your new pharmacy’s records after a transfer. Medication safety isn’t just the doctor’s job. It’s yours too. Below, you’ll find real stories and clear guides on how these errors happen, what to watch for, and exactly what steps to take so you’re never caught off guard again.
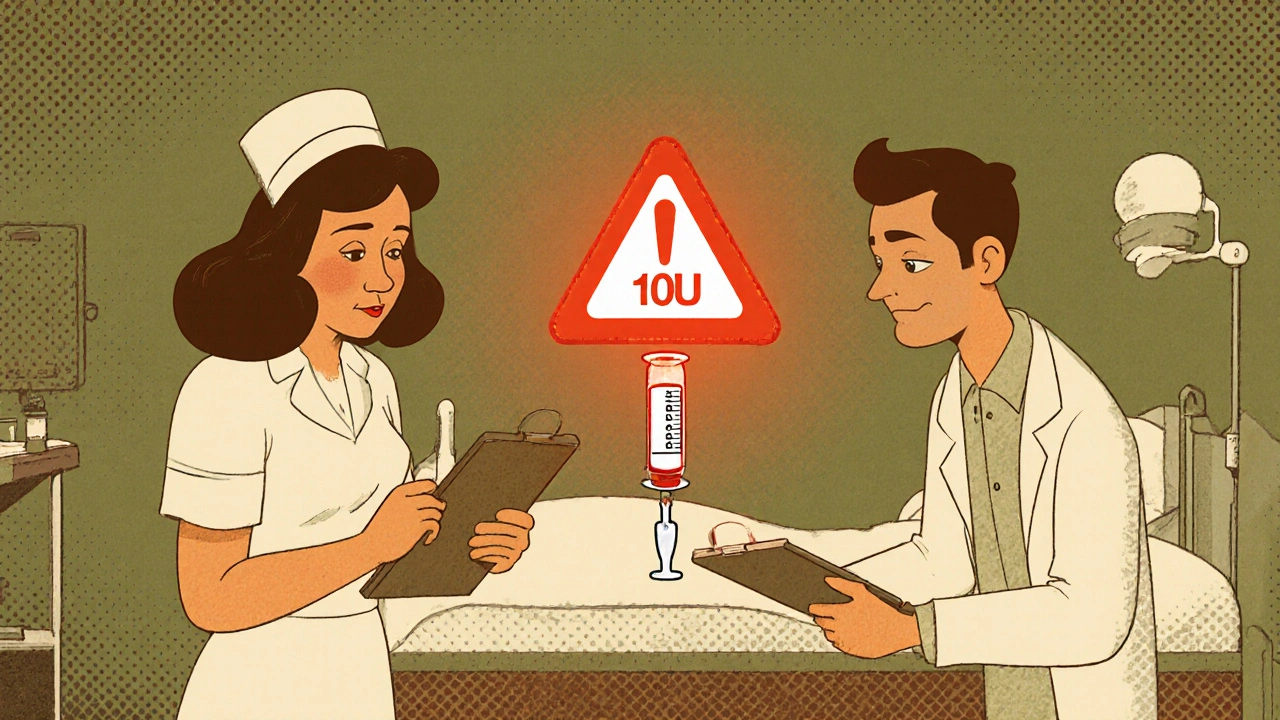
How to Verify Dose Changes and Avoid Miscommunication in Healthcare
Learn how to verify medication dose changes safely using proven protocols like independent double checks, SBAR communication, and targeted barcode scanning to prevent deadly errors in healthcare settings.
Read More