OBRA '90 and How It Changed Drug Pricing, Generics, and Patient Access
When OBRA '90, the Omnibus Budget Reconciliation Act of 1990. Also known as the 1990 Budget Act, it fundamentally changed how the U.S. government regulates prescription drug costs, especially for Medicaid and Medicare beneficiaries. Before OBRA '90, many patients paid full price for medications with no oversight. The law didn’t just tweak rules—it rewrote the playbook for drug access, pricing, and safety.
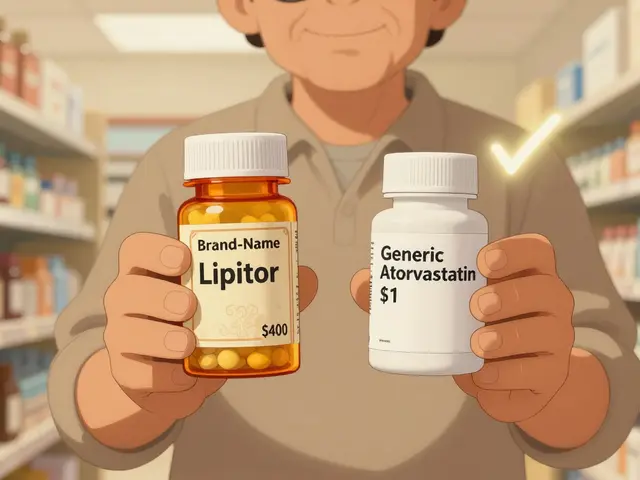
One of its biggest impacts was on generic drugs, lower-cost versions of brand-name medications approved by the FDA. OBRA '90 required states to use the lowest-cost generic available for Medicaid patients unless a doctor specifically wrote "do not substitute." That single rule pushed pharmacies to switch patients to generics, saving billions. It also forced manufacturers to report average wholesale prices, making it harder to hide inflated costs. This transparency laid the groundwork for today’s drug pricing debates and the push for Medicare to negotiate prices.
OBRA '90 also created the first formal formulary restrictions, lists of approved medications covered by insurance plans. Before this, many Medicaid programs covered almost anything. The law allowed states to limit which drugs were covered, but only if they offered exceptions for medical necessity. That balance—control with flexibility—became the model for private insurers and later Medicare Part D. It’s why today, if your insurance denies a generic, you can still appeal under federal rules.
It didn’t stop there. OBRA '90 mandated medication therapy management, a system where pharmacists review a patient’s entire drug list to catch dangerous interactions. This was the first federal push for pharmacists to act as drug safety monitors, not just dispensers. Today, you see the legacy in pharmacist-led reviews for seniors on multiple prescriptions—like those taking warfarin or levothyroxine, where small changes can cause big problems.
The law also tied drug rebates to Medicaid pricing, which pushed manufacturers to lower prices just to stay in the program. That’s why generic drugs in the U.S. are so cheap compared to brand-name ones—and why India’s generic exports now supply half the world. OBRA '90 didn’t fix everything, but it created the foundation for everything that followed: the $2,000 out-of-pocket cap in Medicare Part D, the push for combination generics, and even the rules that now require you to get a symptom diary if you’re tracking drug reactions.
What you’ll find in the posts below isn’t just a list of articles—it’s the direct result of OBRA '90’s ripple effects. From how you get your blood pressure meds to why your insurance denies a generic, from how dose changes after switching generics can be risky to how expired antibiotics still linger in medicine cabinets—all of it connects back to this 1990 law. This isn’t history. It’s your prescription label, your pharmacy bill, and your safety net—all shaped by a single piece of legislation.

Pharmacist Counseling Scripts: Training Materials for Generic Patient Talks
Pharmacist counseling scripts ensure patients understand their medications, improve adherence, and meet legal requirements. Learn the core structure, best practices, and how to adapt scripts for real-world pharmacy settings.
Read More