Overdose Reversal: How Antidotes Like Naloxone Save Lives
When someone overdoses, minutes matter. Overdose reversal, the immediate medical intervention that stops a life-threatening drug reaction. Also known as antidote administration, it’s not just for heroin or fentanyl—it applies to prescription painkillers, sleep aids, and even some antidepressants when taken in dangerous amounts. The most common tool? Naloxone, a fast-acting opioid blocker that can restore breathing in under five minutes. It’s not a cure, but it buys time—time for emergency help to arrive, time to get someone to a hospital, time to survive.
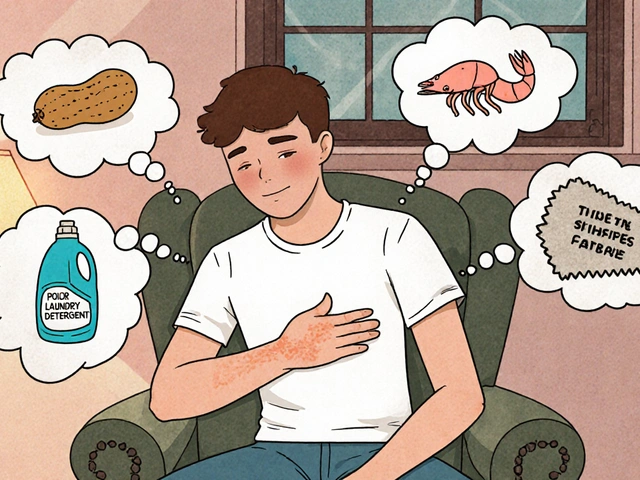
Overdose reversal doesn’t just happen in hospitals. It’s happening in parking lots, basements, and living rooms. Naloxone is now available without a prescription in most states, and many pharmacies hand it out for free. But knowing where to find it isn’t enough. You need to know when to use it. Signs aren’t always obvious: slow or shallow breathing, blue lips, unresponsiveness. If someone’s not waking up and you know they took opioids, don’t wait. Give naloxone. Call 911. Keep giving breaths if you’re trained. Overdose reversal works best when it’s fast, not perfect.
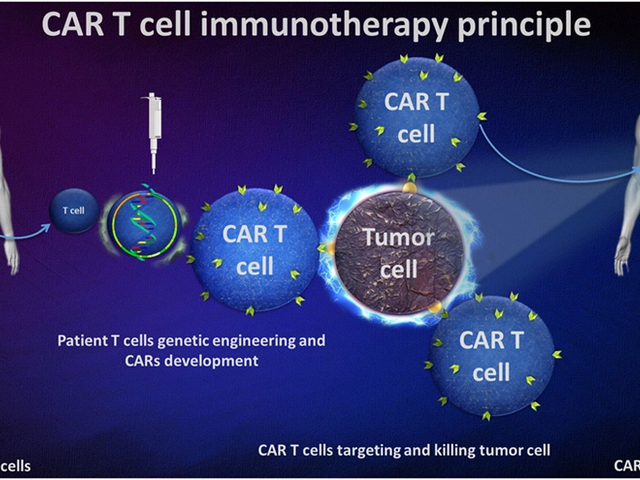
But naloxone isn’t the only player. Some overdoses involve benzodiazepines, antidepressants, or heart medications—each needing different approaches. Overdose reversal means knowing which antidote fits which poison. For example, flumazenil reverses certain sedatives, while glucagon helps with insulin overdoses. And then there’s the hidden layer: people who take multiple meds and don’t realize the risks. That’s why reading your medication guide matters. That’s why keeping a symptom diary helps. That’s why knowing your drug interactions—like how Bactrim can spike your INR or how licorice messes with blood pressure meds—is part of prevention.
Most people think overdose reversal is for addicts. It’s not. It’s for the grandma taking too much painkiller. The college student mixing sleep aids and alcohol. The veteran on opioids after surgery. The person who didn’t know their generic switch changed the dose. This isn’t about judgment. It’s about readiness. The posts below show you how to spot overdose warnings, where to find antidotes, how to store life-saving meds like epinephrine, and why some drugs can’t wait until the expiration date. You won’t need all of this—but if you need one thing, it could save a life. Here’s what you need to know before the next emergency hits.

Naloxone Readiness Plan: How to Keep Patients Safe on Opioids
A naloxone readiness plan saves lives by ensuring quick access to overdose-reversing medication for anyone on opioids. Learn how to store, use, and distribute naloxone effectively.
Read More