Bipolar Depression vs. Unipolar Depression: Key Differences in Diagnosis and Treatment
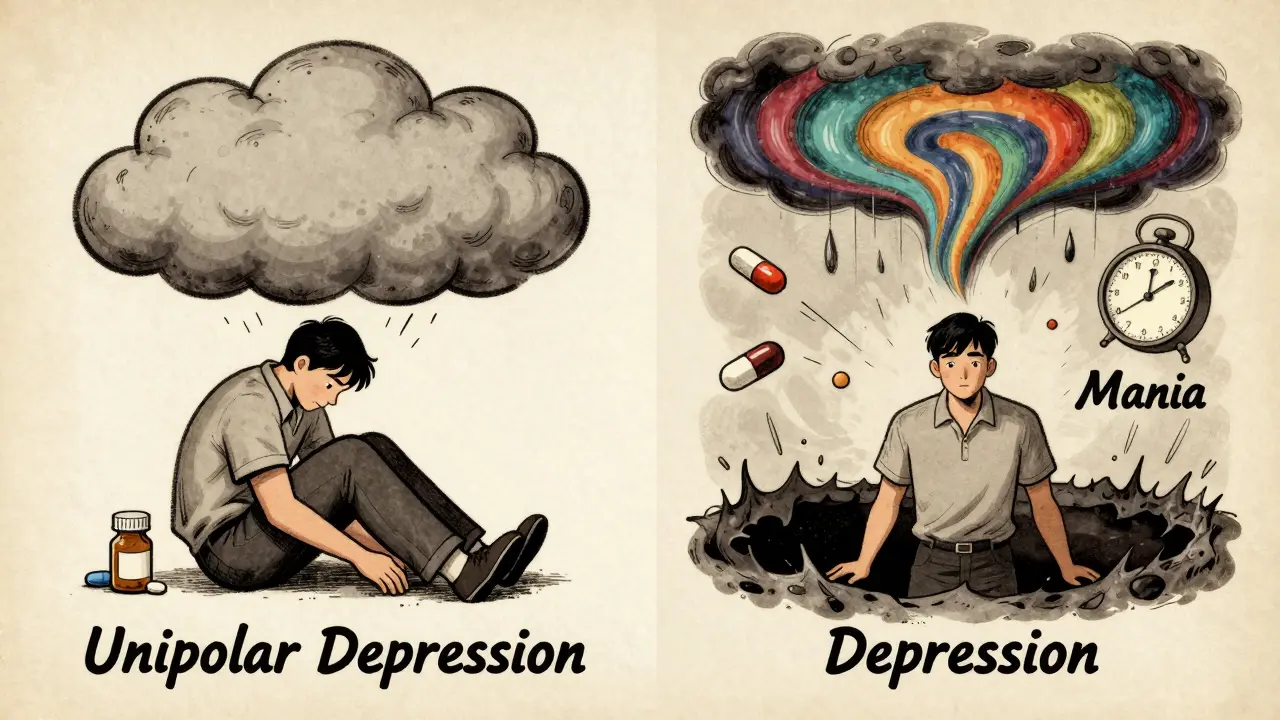
It’s easy to assume all depression is the same. If you’re feeling low, tired, and hopeless, your doctor might just call it depression and hand you an antidepressant. But that simple label can be dangerous. Bipolar depression and unipolar depression - also called Major Depressive Disorder (MDD) - look almost identical on the surface. Both involve deep sadness, loss of energy, trouble sleeping, and difficulty concentrating. But beneath that similarity lies a critical difference that changes everything: treatment, outcome, and sometimes, survival.
What’s the Real Difference?
Unipolar depression means you only experience depressive episodes. No highs. No bursts of energy. No impulsivity. Just the weight of sadness, sometimes for months or years. This is what most people think of when they hear "depression." It’s the most common form - affecting nearly 8% of U.S. adults in 2021, according to the National Institute of Mental Health. Bipolar depression is different. It’s not a standalone condition. It’s the low point of bipolar disorder. People with bipolar disorder swing between deep depression and either full-blown mania (in bipolar I) or hypomania (in bipolar II). Hypomania might look like being unusually energetic, needing less sleep, talking fast, or making risky decisions. But it’s not always obvious - especially when someone is in a depressive episode and doesn’t mention their past highs. The key? History. If you’ve ever had a period where you felt "too good," unusually confident, or reckless - even if it lasted just a few days - you’re not dealing with unipolar depression. You’re dealing with bipolar depression. And that changes your treatment plan completely.How Doctors Tell Them Apart
There’s no blood test or brain scan that can tell the difference. Diagnosis relies on careful questioning and history-taking. Clinicians use tools like the Mood Disorders Questionnaire (MDQ) and the Hypomania Checklist-32 (HCL-32) to screen for hidden manic or hypomanic symptoms. A patient might not remember or recognize their own hypomania. They might say, "I was just productive," or "I didn’t need sleep - that’s normal for me." But there are subtle clues that trained eyes catch:- Early morning waking - more common in bipolar depression (57% vs. 39%)
- Morning worsening of mood - happens in 63% of bipolar cases, compared to 41% in unipolar
- Psychomotor retardation - feeling physically slowed down - affects 68% of bipolar patients vs. 42% of unipolar
- Psychotic symptoms - hallucinations or delusions - appear in 22% of bipolar depression cases, but only 8% in unipolar
- Family history - if a parent or sibling has bipolar disorder, your risk jumps from 1-2% to 5-10%
Why Misdiagnosis Is So Common - and So Dangerous
About 40% of people with bipolar disorder are initially diagnosed with unipolar depression. That’s not a small error. It’s a systemic problem. Why? Because many patients don’t volunteer their manic or hypomanic episodes. They don’t see them as a problem. They might even enjoy the energy. Doctors, under time pressure, focus on the obvious: the depression. The consequences are brutal. A 2017 study found that misdiagnosed bipolar patients spent an average of 8.2 more years on the wrong treatment before getting the right diagnosis. During that time, 63% of them ended up in the hospital because antidepressants triggered mania or rapid cycling. One Reddit user, u/BipolarSurvivor, shared: "I was on Prozac for 7 years. I went from 2 episodes a year to 12. I lost my job. My relationships fell apart. It wasn’t depression - it was the drugs. The STEP-BD study showed that 76% of bipolar patients treated with antidepressants alone experienced mood destabilization. That’s not a side effect - that’s a direct harm.
Treatment: One Size Does NOT Fit All
This is where the difference becomes life-or-death. For unipolar depression, first-line treatment is clear: SSRIs like sertraline or escitalopram. About 60-65% of people respond within 8-12 weeks. If that doesn’t work, SNRIs like venlafaxine or duloxetine are next. Psychotherapy - especially Cognitive Behavioral Therapy (CBT) - helps reframe negative thinking patterns. Many people with a single episode can stop medication after 6-12 months of stability. For bipolar depression, antidepressants are risky. They’re not first-line. They’re not even second-line. They’re last-resort - and only used with a mood stabilizer. First-line treatments for bipolar depression include:- Lithium - the oldest mood stabilizer. It reduces depressive episodes by 48% compared to placebo.
- Quetiapine (Seroquel) - an atypical antipsychotic. It’s one of the few FDA-approved treatments for bipolar depression, with a 58% response rate.
- Lurasidone (Latuda) - another antipsychotic approved for bipolar depression. It works without causing weight gain or sedation as much as others.
Long-Term Management: Lifelong vs. Time-Limited
Unipolar depression can be episodic. After one episode, some people never have another. Even after multiple episodes, if someone stays well for two years, doctors may consider slowly tapering medication. Bipolar disorder is chronic. Stopping mood stabilizers is like turning off a fire alarm. The relapse rate? 73% within five years if treatment stops. That’s why most people with bipolar disorder need to stay on medication for life - not because they’re broken, but because their brain chemistry needs constant balance.
Emerging Hope: New Tools and Science
The field is changing. In 2019, the FDA approved esketamine (Spravato) for treatment-resistant unipolar depression. It works fast - sometimes in hours. For bipolar depression, cariprazine (Vraylar) was approved the same year, offering remission in 36.6% of patients vs. 23% on placebo. New research is even more exciting. A 2023 Lancet Psychiatry study identified a 12-gene pattern that distinguishes bipolar from unipolar depression with 83% accuracy. That’s not in clinics yet - but it’s coming. Digital tools are also helping. Apps that track sleep, activity, and speech patterns can detect subtle mood shifts before a person even notices them. This could catch hypomania early - before it spirals.What You Should Do If You’re Unsure
If you’ve been diagnosed with depression but:- Antidepressants didn’t help - or made you feel worse
- You’ve had periods of high energy, impulsivity, or reduced need for sleep
- Family members have bipolar disorder or have been hospitalized for mood swings
- You’ve cycled through moods faster than once a year
Final Thought: Diagnosis Is Not a Label - It’s a Map
Getting the right diagnosis isn’t about being "bipolar" or "depressed." It’s about finding the right path forward. One path leads to antidepressants and time-limited therapy. The other leads to mood stabilizers, routine, and lifelong management. Get it wrong, and you risk years of unnecessary suffering. Get it right, and you can live a full, stable life.Don’t accept a diagnosis without asking: "Could this be bipolar?" It’s not a scary word. It’s a necessary one.
Can you have bipolar depression without ever having a manic episode?
No. By definition, bipolar depression only occurs in people who have had at least one manic or hypomanic episode. If someone has only ever experienced depression, they have unipolar depression (Major Depressive Disorder). However, hypomanic episodes can be subtle - they might be mistaken for productivity, creativity, or just being "on fire." Many people don’t realize these episodes were abnormal until later.
Are antidepressants always bad for bipolar depression?
Not always, but they’re risky. Antidepressants alone can trigger mania, rapid cycling, or mixed episodes in people with bipolar disorder. The FDA and major guidelines (NICE, APA) strongly advise against using them without a mood stabilizer. However, once mood is stabilized with lithium, quetiapine, or lurasidone, some doctors may cautiously add an antidepressant for a short time - but only if the depression is severe and hasn’t responded to other treatments.
How long does it take to diagnose bipolar depression correctly?
On average, it takes 8 to 10 years from first symptom onset to correct diagnosis. Many people see multiple doctors, try several medications, and experience multiple hospitalizations before someone connects the dots between depressive episodes and past hypomanic symptoms. This delay is why screening tools and family history are so important.
Can bipolar depression turn into unipolar depression?
No. Bipolar disorder is a lifelong condition. Once someone has had a manic or hypomanic episode, they have bipolar disorder - even if they haven’t had one in years. The depressive episodes may become more frequent, but the underlying condition doesn’t change. However, some people with bipolar disorder go long periods without mania - especially with proper treatment - which can make them feel like they’ve "gotten over it." That’s not recovery from bipolar disorder - it’s successful management.
Is bipolar depression more severe than unipolar depression?
It’s not necessarily more severe in terms of depressive symptoms - both can be equally debilitating. But bipolar depression comes with higher risks: more frequent episodes, faster cycling, greater risk of suicide, and the danger of antidepressant-induced mania. Studies show bipolar depression has higher rates of hospitalization, work loss, and functional impairment over time - not because the sadness is worse, but because the illness is more complex and harder to treat correctly.




12 Comments
Scottie Baker
January 13, 2026 at 21:58
Man, I was on Lexapro for 3 years. Thought I was just 'depressed.' Turned out I was cycling every 3 weeks. My doctor never asked about sleep or energy spikes. I thought I was just 'a high-energy person.' Turns out I was one bad prescription away from losing everything. Don't let them gaslight you into thinking it's just 'bad mood.'
Kimberly Mitchell
January 14, 2026 at 14:06
This article is pure pseudoscience dressed up as clinical wisdom. You're pathologizing normal human variation. People have ups and downs. Not everything needs a DSM label and a lifetime of pills. The pharmaceutical industry loves this narrative. Wake up.
Anny Kaettano
January 15, 2026 at 10:30
As a therapist who’s seen hundreds of cases, I can confirm: the MDQ and HCL-32 are underused. Too many clinicians rely on the patient’s self-report, but hypomania is often invisible to the person experiencing it. I always ask: 'Did you ever feel so good you couldn’t sit still? Did you spend money you didn’t have? Did you think you could run a marathon on 3 hours of sleep?' Those are the red flags. Not the sadness.
Jesse Ibarra
January 16, 2026 at 17:54
Wow. Just wow. This is exactly the kind of overmedicalized nonsense that turns healthy people into patients. You’re telling people their creativity is a disorder. Their confidence is 'hypomania.' Their productivity is 'pathology.' This isn’t medicine-it’s control. The real epidemic isn’t bipolar disorder-it’s the psychiatric industrial complex.
Gregory Parschauer
January 18, 2026 at 01:28
Let me just say this: if you’re not prescribing lithium first-line for suspected bipolar depression, you’re not just negligent-you’re endangering lives. SSRIs are like handing a drunk person a chainsaw. The data is 20 years old and still holds. Quetiapine? Fine. Lurasidone? Acceptable. But if you’re skipping mood stabilizers because you’re too lazy to do a proper history? You’re not a doctor-you’re a vending machine for prescriptions.
Diana Campos Ortiz
January 18, 2026 at 05:39
I was diagnosed at 22 with MDD. Took 12 years to get the right diagnosis. My mom had bipolar. I never connected it. I thought my 'good spells' were just me being 'on my game.' Turns out I was burning out every 4 months. IPSRT changed my life. I sleep, eat, and walk at the same time every day. It’s boring. It’s also the only thing keeping me alive.
Vinaypriy Wane
January 19, 2026 at 19:22
Can I just say-this is why we need better training for primary care doctors? They’re the first point of contact. They have 12 minutes. They see 'sadness' and write 'SSRI.' They don’t ask about sleep patterns, family history, or energy spikes. I’ve seen it too many times. It’s not malice-it’s ignorance. And ignorance kills.
Robin Williams
January 20, 2026 at 22:59
bro i had a manic episode in college and i thought i was just a genius who didn’t need sleep. turned out i maxed out 3 credit cards and sent 17 emails to my ex saying i was the chosen one. now i take quetiapine and i’m chill as hell. it’s not a curse. it’s just a different brain wiring. stop shame. start science.
jefferson fernandes
January 21, 2026 at 14:49
For the record: bipolar depression isn’t 'worse' than unipolar. It’s just more complex. The sadness feels the same. The fatigue is identical. The tears? Same. But the risk of being triggered by a simple antidepressant? That’s the hidden killer. We need to stop treating depression like a one-size-fits-all hoodie. It’s a custom suit. Get measured properly.
Acacia Hendrix
January 22, 2026 at 16:34
It’s fascinating how the literature on bipolar depression has evolved. The 2023 Lancet Psychiatry gene panel is a watershed moment-12-gene signature with 83% specificity. This is the beginning of biomarker-driven psychiatry. We’re moving from phenomenology to molecular phenotyping. The future of diagnosis is no longer clinical interview-it’s transcriptomic profiling. We’re on the cusp of a paradigm shift.
Alan Lin
January 24, 2026 at 08:55
Thank you for writing this with such precision. As someone who’s spent years advocating for mental health literacy, I can say this is one of the clearest, most accurate summaries I’ve seen. The statistics are sobering, the treatment distinctions are vital, and the call for better screening is urgent. Please share this with every primary care clinic, every ER, every college counseling center. Lives depend on this knowledge.
mike swinchoski
January 24, 2026 at 18:12
You're all overthinking this. Depression is depression. You take pills. You talk to someone. You get better. Stop making it sound like a sci-fi movie with gene panels and lithium and IPSRT. It's just sadness. You don't need all this jargon. Just be nice to yourself.