Chemotherapy HBV Risk: What You Need to Know About Hepatitis B Reactivation
When you’re undergoing chemotherapy, a treatment that uses drugs to kill cancer cells, often by targeting fast-growing cells in the body. Also known as cancer chemotherapy, it’s a life-saving tool—but it can also weaken your immune system in ways you might not expect. One hidden danger is hepatitis B virus (HBV) reactivation, a condition where a dormant HBV infection suddenly becomes active again due to immune suppression. This isn’t rare—it happens in up to 20% of people who carry HBV and start chemotherapy, even if they never had symptoms. Many people don’t know they have HBV. They might have been infected years ago, cleared the virus on their own, or never felt sick. But the virus can still hide in their liver. When chemotherapy hits, that hidden virus can flare up, causing severe liver damage, liver failure, or even death.
That’s why HBV screening, a simple blood test to check for hepatitis B surface antigen (HBsAg) and core antibody (anti-HBc). Also known as liver viral panel, it’s now standard before starting most cancer treatments. Doctors don’t just test for active infection—they look for signs of past exposure too. If you test positive, you’ll likely get antiviral prophylaxis, a preventive course of antiviral drugs like entecavir or tenofovir taken before and during chemotherapy. Also known as HBV suppression therapy, it reduces reactivation risk by over 90%. Skipping this step isn’t worth the risk. Even if you feel fine, your liver might be quietly carrying HBV. And if you’re getting chemo for lymphoma, leukemia, or breast cancer, your risk is higher. Some treatments, like rituximab or stem cell transplants, are especially dangerous for people with hidden HBV.
It’s not just about the drugs you take—it’s about knowing your body’s history. If you’ve ever had a blood transfusion, used IV drugs, had unprotected sex, or were born in a region where HBV is common (Asia, Africa, Eastern Europe), you’re at higher risk. Talking to your oncologist about HBV screening isn’t optional—it’s essential. Most people who get screened and treated early never have problems. But those who don’t? They end up in the hospital, sometimes with irreversible damage. This isn’t a guess. It’s backed by guidelines from the CDC, WHO, and major cancer societies. You’re not being paranoid. You’re being smart.
What you’ll find below are real, practical posts that dig into how chemotherapy affects your body beyond cancer cells—how drugs interact with viruses, what blood tests really mean, and how to protect your liver while fighting cancer. These aren’t theory pieces. They’re guides written for people who need to understand what’s happening to their body, and how to take control of it.
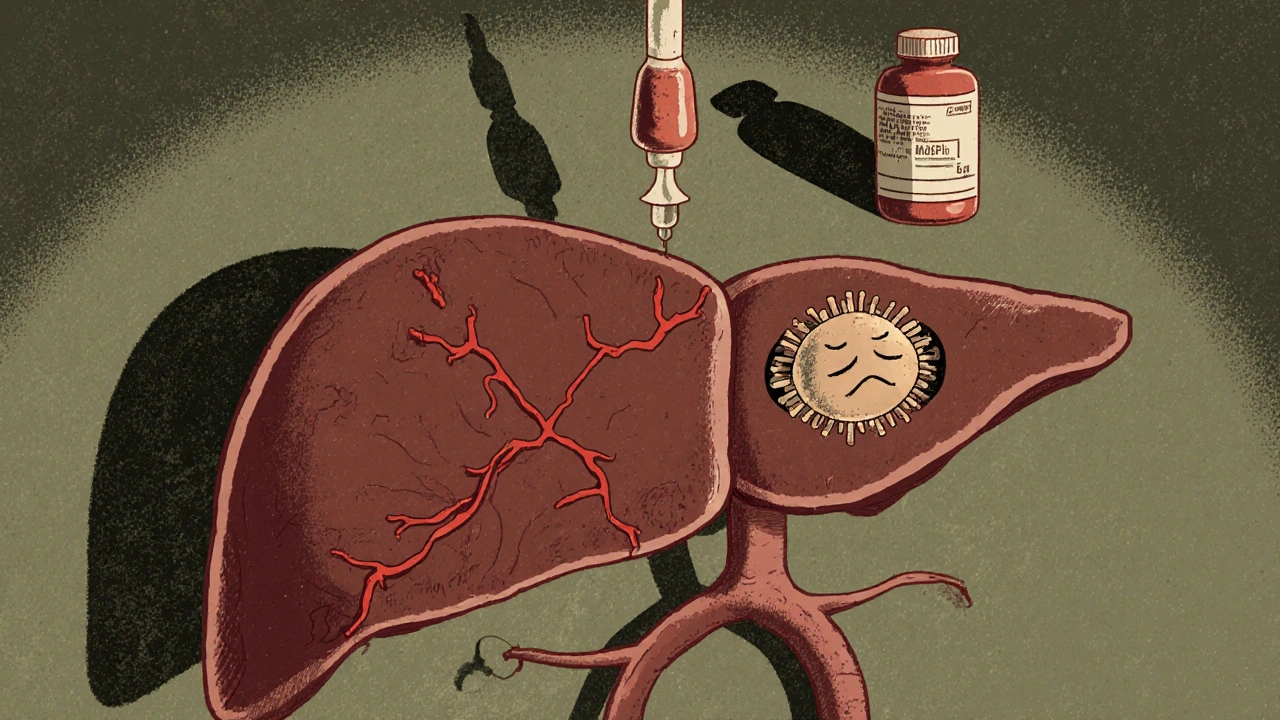
HBV Reactivation: How Biologics and Chemotherapy Trigger Liver Danger - And How to Stop It
HBV reactivation can cause liver failure in patients on chemotherapy or biologics. Screening for hepatitis B before treatment and using antiviral prophylaxis can prevent deadly complications - but too many patients still go unprotected.
Read More