Immunosuppressant Drugs: What They Are, How They Work, and What You Need to Know
When your immune system goes too far—attacking your own body or a transplanted organ—immunosuppressant drugs, medications that intentionally lower immune system activity to prevent harmful overreactions. Also known as anti-rejection drugs, they’re life-saving for people with organ transplants, lupus, rheumatoid arthritis, and other autoimmune conditions. But they’re not harmless. These drugs don’t just calm the bad reactions—they lower your body’s defenses against infections, cancers, and even some vaccines. That’s why knowing how they work, who needs them, and what to watch for isn’t just helpful—it’s critical.
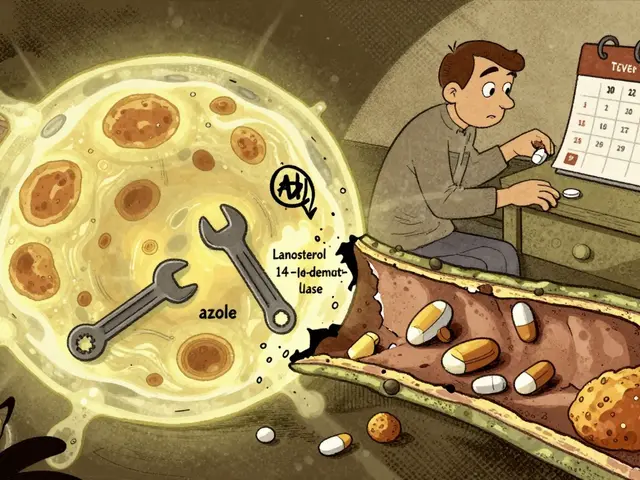
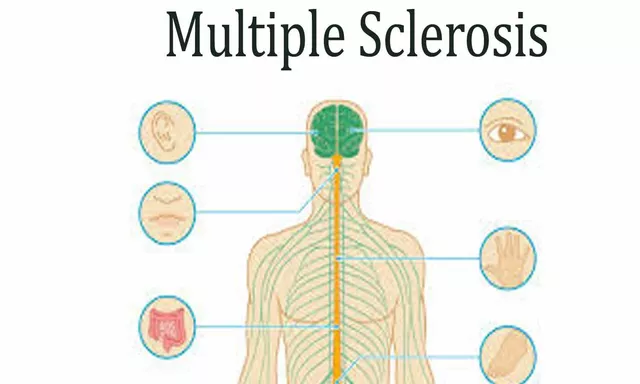
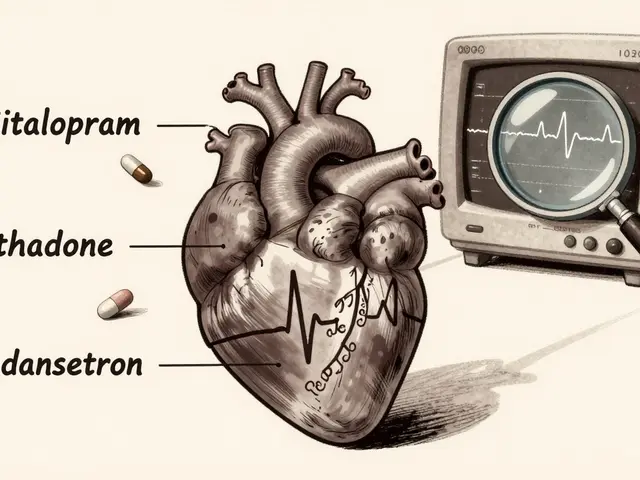
Organ transplant, the surgical replacement of a failing organ with a healthy one from a donor is the most common reason people take immunosuppressants long-term. Without them, the body sees the new kidney, liver, or heart as an invader and tries to destroy it. But these drugs don’t just protect the transplant—they can also help with autoimmune disease, conditions where the immune system mistakenly attacks healthy tissues like joints, skin, or nerves. Drugs like cyclosporine, tacrolimus, and mycophenolate are used for everything from severe psoriasis to Crohn’s disease. But they don’t pick and choose. They slow down your entire immune response. That means you’re more likely to get sick from a cold virus, or develop skin cancer from sun exposure. And they don’t play nice with other meds—drug interactions, harmful or reduced effects when two or more medications are taken together are common. Grapefruit juice, certain antibiotics, even some herbal supplements can spike drug levels in your blood and cause kidney damage or nerve problems.
Side effects aren’t just theoretical. People on these drugs report constant fatigue, shaky hands, high blood pressure, and unusual weight gain. Some lose their hair. Others get mouth sores or digestive issues that last for months. And because these drugs are often taken for years, the long-term risks pile up—kidney damage, increased risk of lymphoma, diabetes. That’s why monitoring isn’t optional. Regular blood tests, skin checks, and doctor visits aren’t just routine—they’re your safety net. You can’t just take the pill and forget it. You need to know your numbers, track your symptoms, and speak up when something feels off.
What you’ll find below isn’t a textbook. It’s real-world advice from people who’ve lived with these drugs, and the guides that help them stay safe. You’ll learn how to spot early signs of infection, what to ask your pharmacist about interactions, why some people need to avoid certain vaccines, and how to handle side effects without stopping treatment. These aren’t guesses. They’re based on patient experiences, FDA warnings, and clinical evidence. Whether you’re just starting immunosuppressants or have been on them for years, this collection gives you the tools to take control—not just survive, but stay well.
Organ Transplant Recipients: Immunosuppressant Drug Interactions and Side Effects
Organ transplant recipients must take lifelong immunosuppressant drugs to prevent rejection, but these medications carry serious side effects and dangerous drug interactions. Learn how tacrolimus, mycophenolate, and steroids impact health, what to watch for, and how modern protocols are improving outcomes.
Read More