INR Elevation: What It Means, Why It Happens, and How to Manage It
When your INR, International Normalized Ratio, a standardized measure of how long it takes your blood to clot. Also known as prothrombin time ratio, it’s a critical number for anyone taking blood thinners like warfarin. goes too high, your blood takes longer than normal to clot. That might sound good if you’re trying to prevent clots—but too much of a good thing can lead to dangerous bleeding. An INR above 4.5 is considered elevated and increases your risk of internal bleeding, even from minor injuries.
INR elevation usually happens because of changes in your medication, diet, or other drugs you’re taking. warfarin, a common anticoagulant used to prevent strokes and blood clots is especially sensitive. Even small shifts in dosage, or switching to a generic version, can push your INR out of range. That’s why doctors often adjust doses after switching generics—something covered in multiple posts here. Your liver also plays a big role. If it’s not working well, maybe due to disease or medication interactions, it can’t process warfarin properly, leading to higher INR. And then there’s diet. vitamin K, a nutrient found in leafy greens that helps your blood clot directly opposes warfarin’s effect. Eating more spinach or kale one week and less the next can swing your INR up or down.
It’s not just about warfarin. Other anticoagulants don’t require INR monitoring, but if you’re on warfarin, your INR is your lifeline. Too low, and you risk a stroke or clot. Too high, and you risk bleeding into your brain, gut, or joints. That’s why regular testing matters—sometimes weekly, sometimes monthly. And it’s not just about the number. Symptoms like unusual bruising, nosebleeds, dark stools, or headaches can signal trouble before your test results come back. Many people don’t realize how many factors affect INR: antibiotics, herbal supplements like garlic or ginseng, even changes in alcohol intake. The posts here dig into these connections—how switching meds, expired drugs, or liver issues can all tie back to your INR.
If your INR is elevated, don’t panic, but don’t ignore it either. Your doctor might hold your next dose, lower the amount, or give you vitamin K to bring it down. But the real win? Prevention. Keep your diet steady. Tell every new doctor you’re on warfarin. Use the same pharmacy every time. Check for interactions before taking anything new—even over-the-counter painkillers. The more you understand what moves your INR, the less likely you are to end up in the ER because of a simple mistake.
Below, you’ll find real-world guides from people who’ve been there—how to handle dose changes after switching generics, what to watch for with liver transplants and immunosuppressants, and why expired meds or licorice can quietly mess with your clotting. This isn’t theory. It’s what keeps people safe.

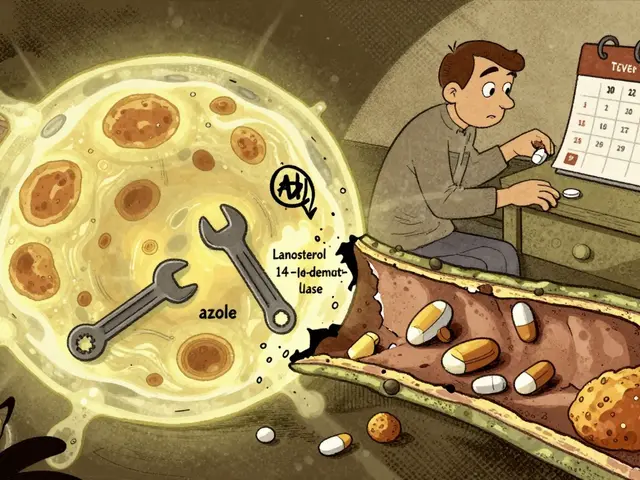
Trimethoprim-Sulfamethoxazole and Warfarin: How This Antibiotic Can Raise Your INR and Increase Bleeding Risk
Trimethoprim-sulfamethoxazole (Bactrim) can dangerously raise INR levels in people taking warfarin, increasing bleeding risk. Learn how this interaction works, who’s most at risk, and what to do if your INR spikes.
Read More