Generic Drugs: What They Are, Why They Matter, and When to Watch Out
When you hear generic drugs, lower-cost versions of brand-name medications that contain the same active ingredients and meet the same FDA standards. Also known as non-brand medications, they make up nearly 90% of prescriptions in the U.S. and are why millions can afford their daily pills. But here’s the thing: just because they’re cheaper doesn’t mean they’re all the same. For most people, switching from brand to generic is smooth and safe. For others—especially those on drugs like warfarin, levothyroxine, or phenytoin—it can trigger serious side effects if not handled right.
That’s where NTI drugs, narrow therapeutic index medications where tiny differences in dosage can cause big health risks come in. These aren’t just any pills. A 5% change in absorption can mean your blood thinning goes from safe to dangerous, or your thyroid levels swing out of control. That’s why doctors sometimes adjust your dose after switching to a generic version. And it’s also why some pharmacies won’t swap your levothyroxine without checking with your doctor first.
Then there’s the global side of this. Indian generic drugs, high-quality, low-cost medicines produced in India and shipped worldwide are the backbone of affordable healthcare across Africa, Latin America, and even parts of Europe. India makes 20% of the world’s generics and over 60% of its vaccines. These aren’t knockoffs—they’re FDA-approved, rigorously tested, and often cheaper than the brand names sold in the U.S. But here’s the catch: not every generic you get at your local pharmacy comes from the same factory. Some are made in the U.S., others in India, China, or Germany. And while all must meet the same legal standards, your body might react differently to each formulation.
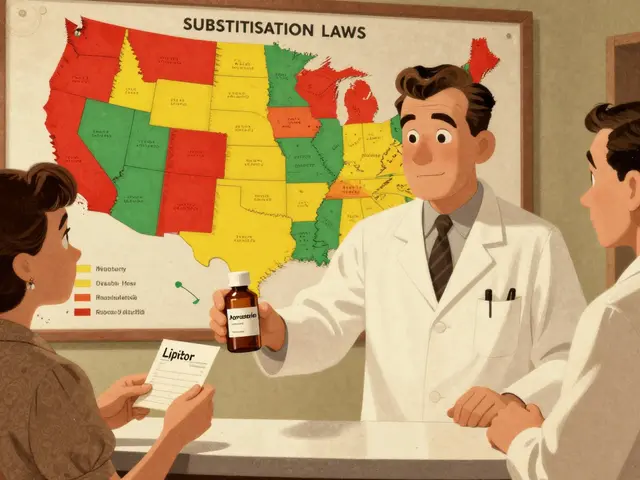
Price differences between countries aren’t just about profit. They’re about policy. In the U.S., drugmakers charge what the market will bear. In Canada, Germany, or Australia, governments negotiate prices. That’s why a 30-day supply of a generic blood pressure pill might cost $4 in Canada and $40 in the U.S.—even if it’s the exact same tablet. And when your insurance denies coverage for a generic you need, it’s not always about cost—it’s about formulary rules, bureaucratic delays, and sometimes, plain oversight.
So what should you do? Know your meds. If you’re on a drug where small changes matter, ask your pharmacist if your generic is the same as last time. Keep a log if you notice new side effects after a switch. Check your prescription label for the manufacturer name—it’s often printed in tiny text, but it matters. And if your doctor doesn’t mention dose changes when switching, ask. You’re not being difficult—you’re being smart.
The posts below dig into exactly this: how to spot when a generic switch needs attention, why Indian manufacturers dominate the market, how insurance fights you over coverage, and what to do when your blood pressure meds stop working after a refill. You’ll find real stories, real data, and real steps to protect yourself. No fluff. Just what you need to know before your next pharmacy visit.
Federal Food, Drug, and Cosmetic Act: How It Built the Legal Foundation for Generic Drugs
The FD&C Act laid the groundwork for drug safety in the U.S., but it was the Hatch-Waxman Amendments that created the legal pathway for generic drugs. Today, 90% of prescriptions are generic-saving billions thanks to this system.
Read More
Why Most Drugs Don't Have Authorized Generics - And What It Means for Your Prescription Costs
Not all drugs have authorized generics - because they're not meant to be widely available. They're strategic tools used by brand manufacturers to control competition and protect profits, not to lower prices for everyone.
Read More
Future of Global Generic Markets: Key Trends and Predictions for 2025-2030
The global generic drug market is growing rapidly, driven by rising chronic diseases and cost pressures. India and China lead manufacturing, while biosimilars and regulatory shifts are reshaping the industry. Discover key trends shaping the future of affordable medicine.
Read More
Planning for Patent Expiry: What Patients and Healthcare Systems Need to Do Now
Patent expiry means cheaper drugs-but only if you plan ahead. Learn what patients and healthcare systems need to do before brand-name drugs lose exclusivity and generics take over.
Read More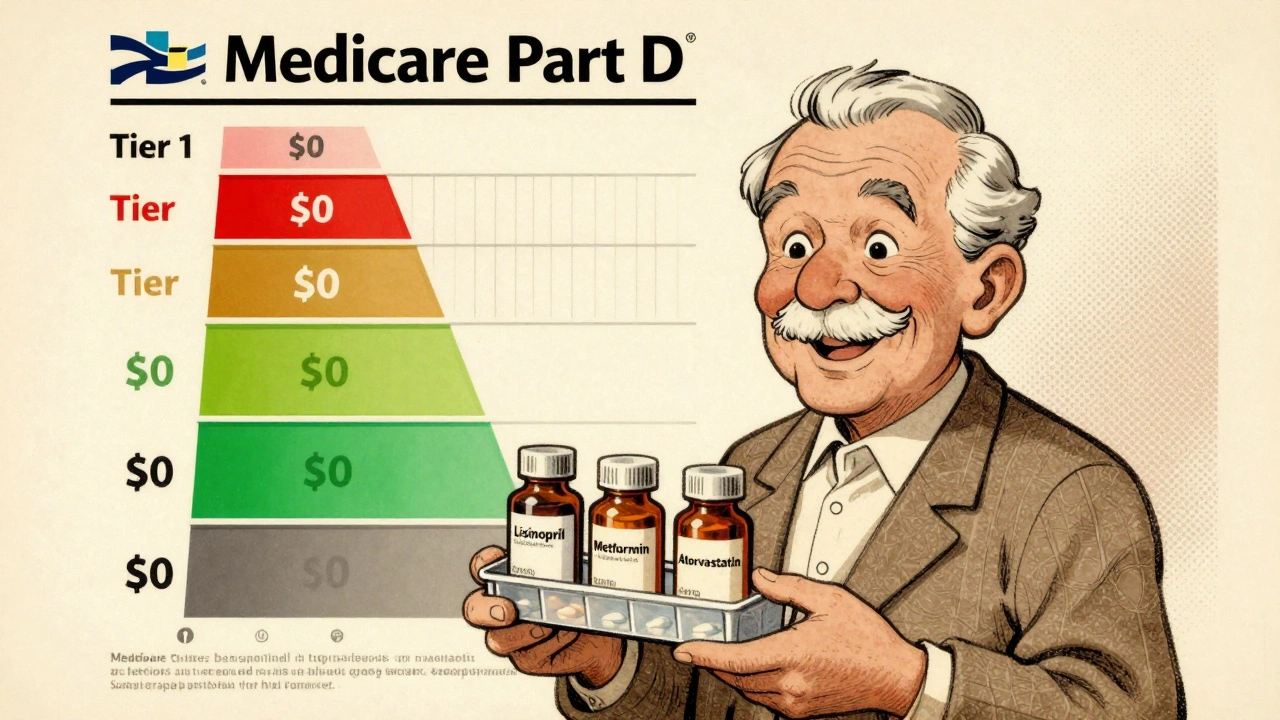
Medicare Part D Formularies: How Generic Coverage Works in 2025
Learn how Medicare Part D covers generic drugs in 2025 - including tiered costs, the $2,000 out-of-pocket cap, and how to save money on your prescriptions.
Read More